| Author | Affiliation |
|---|---|
| Jeremy Brown, MD | The George Washington University School of Medicine, Washington, DC |
| Rita Fleming, MD | The George Washington University School of Medicine, Washington, DC |
| Jamie Aristzabel, MD | The George Washington University School of Medicine, Washington, DC |
| Rocksolana Gishta, BA | The George Washington University School of Medicine, Washington, DC |
ABSTRACT
Introduction:
Physicians are taught that the pelvic exam is a key part of the evaluation of a woman presenting with abdominal pain or vaginal bleeding. However, the exam is time consuming and invasive, and its use in the emergency department (ED) has not been prospectively evaluated. We evaluated how often the findings of the pelvic exam changed management in a cohort of consecutive female patients presenting with acute abdominal pain or vaginal bleeding.
Methods:
We enrolled women who required a pelvic exam together with the providers caring for them in an academic ED from September 2004 to August 2005. We collected the results of the general history and physical exam. The provider was asked to predict the findings of the pelvic exam, and these were compared with the actual findings of the exam.
Results:
One hundred eighty-three patients were prospectively entered into the study. When compared with predicted findings, the pelvic exam was as expected in 131 patients (72%). In a further 40 patients (22%), the findings of the pelvic exam were not as predicted, but resulted in no change in the clinical plan. In 12 cases (6%) the exam revealed a finding that was both unexpected and changed the clinical plan. Only one of these patients was admitted. Of the 24 patients who were admitted, four had a pelvic exam that revealed unexpected results, but only one of these cases caused the physician to change the care planned for the patient.
Conclusion:
In 94% of women with acute abdominal pain or vaginal bleeding, the results of the pelvic exam were either predictable or had no effect on the clinical plan. This suggests that there may be a subset of women with abdominal pain or vaginal bleeding in whom a pelvic exam may safely be deferred.
INTRODUCTION
From early in their training, physicians were taught that all women with lower abdominal pain or vaginal bleeding should have a pelvic exam as part of their evaluation. The exam is thought to add valuable information that will aid the physician in reaching the correct diagnosis, and most emergency medicine and general surgery texts describe the pelvic exam as a key part of the evaluation of a woman presenting to the emergency department (ED) with these symptoms. However, performing a pelvic exam in a busy ED is often challenging. It requires that the patient be placed in an examination room that offers privacy and that a chaperone be present for the duration of the exam. Furthermore, the reliability and accuracy of the exam itself has been questioned.1,2 It can be uncomfortable as well as being emotionally and physically invasive and is a source of anxiety and embarrassment.3–6 Given all this, we wondered how the pelvic exam actually changes the management of ED patients with abdominal pain or vaginal bleeding. Is there important information that can only be obtained through the performance of the pelvic examination, or would the ED management be largely unaffected by the findings of placed in an examination room that offers privacy and that a chaperone be present for the duration of the exam. Furthermore, the reliability and accuracy of the exam itself has been questioned.1,2 It can be uncomfortable as well as being emotionally and physically invasive and is a source of anxiety and embarrassment.3–6 Given all this, we wondered how the pelvic exam actually changes the management of ED patients with abdominal pain or vaginal bleeding. Is there important information that can only be obtained through the performance of the pelvic examination, or would the ED management be largely unaffected by the findings of the exam? To provide some preliminary answers to this we performed a pilot study to examine the influence of the pelvic exam on the management of women with acute abdominal pain or vaginal bleeding in the ED. We also decided to study the role of the pelvic exam in patients who were admitted, since this subgroup is generally more sick and the findings of the pelvic exam may play a greater role in determining their clinical pathway.
METHODS
We performed a prospective cohort study of a convenience sample of women in whom the attending physician determined that a pelvic examination was required because of a complaint of abdominal pain or vaginal bleeding. The pelvic exam was performed on patients needing a bimanual exam to assess for tenderness, as well as those requiring a visual examination to look for bleeding or discharge. The study was performed in a large urban academic ED that treats 60,000 patients each year. Trained research assistants enrolled consecutive patients for 16 hours a day over a one-year period, September 2004 through August 2005.
During the study period, research assistants approached consecutive female patients with abdominal pain or vaginal bleeding for whom the physician or provider felt that a pelvic exam was necessary. If the patient gave her written consent, the treating physician or provider was asked to consent to the study as a secondary subject. Once informed consent from both the patient and her ED physician or provider had been obtained, a two-part survey was completed by the patient and the physician or provider. The surveys were structured instruments with fixed options for answers. The patient survey gathered demographics and data about medical history and the primary complaint. The provider survey collected the reasons for performing the pelvic exam and predictions about what the exam would show based on the information already gathered from the patient’s history and general physical exam. The provider then performed the pelvic exam in the usual way and was interviewed a second time by the research assistant. In this second interview, the provider was asked to report the actual findings of the pelvic exam and to record if the pelvic exam findings changed the patient’s ED management – although the exact change in management was not recorded. Results of laboratory and radiographic tests were also collected and correlated with the predicted and actual findings of the pelvic exam. Researchers also recorded the results of other laboratory and radiological testing as well as the final discharge diagnosis.
The Institutional Review Board approved the study. We excluded the following patients from further analysis; a) patients who had been examined by a medical students (because of inexperience); b) patients with a suspected vaginal foreign body (direct visualization is required); c) patients who had the exam to obtain cultures (pelvic exam was required to obtain cultures), and d) patients in whom the exam was performed to look for products of conception (visualization is required).
RESULTS
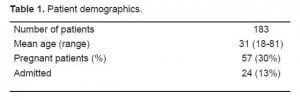
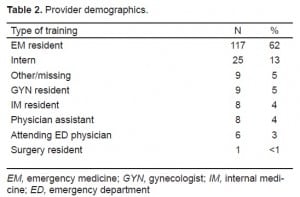
A total of 320 patients with a mean age of 31 agreed to participate in the study, of whom 26 were pregnant. We excluded 42 patients who had been examined by medical students, eight who had a suspected vaginal foreign body, 40 who had the exam to obtain cultures, and 43 who had the exam to look for products of conception. In these final 43 cases, the pelvic exam was performed before the results of a pregnancy test confirmed that the patient was pregnant. The provider determined the need to look for products of conception based on the patient’s unconfirmed history of being pregnant. Data about the overall impression of the pelvic exam were incomplete in four cases, which were also excluded from the analysis. This resulted in 183 patients enrolled in the study, on whom the pelvic examination had been performed to obtain clinical information unobtainable from a routine history and abdominal exam (Table 1). The levels of experience of the providers are shown in Table 2; the majority of the providers performing the pelvic examination were emergency medicine residents (n=117, 63%).
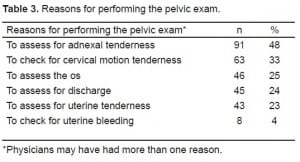
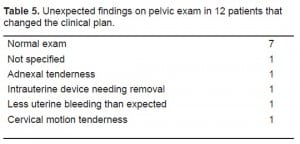
The reasons for performing the pelvic exam are shown in Table 3, and providers were able to give more than one reason for doing the exam. The most common reasons were to assess for adnexal tenderness, (n=90, 48%), cervical motion tenderness (n=61, 33%), and to asses the cervical os (n=44, 25%). The findings most commonly predicted were a normal exam (n=66, 36% of all exams done), uterine bleeding (n=44, 24%) and adnexal tenderness (n=44, 24%). The overall provider impression of the pelvic exam was that it was either as expected or was unexpected but resulted in no change in plan for 171 cases (94%) [Table 4]. In the remaining 12 cases (6%) the exam revealed a finding that was both unexpected and changed the clinical plan (Table 5).
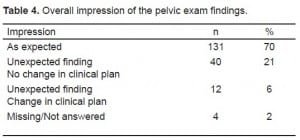
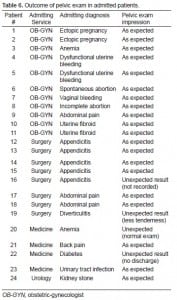
The overall admission rate was 13% (n=24). Of the 24 patients admitted, 20 had a pelvic exam that was as predicted, three had an unexpected finding that resulted in no change in the clinical plan, and one had a finding that caused the physician to change the care planned for that patient, who was admitted with a diagnosis of anemia (Table 6).
DISCUSSION
The pelvic exam has long been required as an essential part of the physical exam for women with abdominal pain regardless of the presumed etiology. This is because it is thought to add important information, and thus should be performed despite its invasive nature. For example, in the chapter on the approach to acute abdominal pain in one standard emergency medicine textbook, authors suggest that “…it is wise to maintain a low threshold for performing a pelvic examination in the evaluation of abdominal pain, particularly in women of reproductive age, regardless of where in the abdomen the pain is localized.”7 A recent video teaching the technique of the pelvic exam states that “[a]ny patient with genital or pelvic symptoms should…undergo a gynecological exam”.8 Standard textbooks of surgery share this approach, which may be traced back to the early surgical texts.9–11J.W MacDonald’s12 Clinical Textbook of Surgical Diagnosis and Treatment, published in 1898, states that mistakes made in the diagnosis of appendicitis occur because “the surgeon has neglected the imperative duty of making a vaginal examination…diagnosis of appendicitis in a female should never be entertained until pelvic inflammation, especially of the ovaries and tubes, has been excluded.”
Although these authors emphasis the importance of the pelvic exam, our pilot study demonstrated that out of this sample of 183 ED patients, the findings from pelvic exam changed the management in only 12 cases (6%). In all other cases, the findings of the pelvic exam – even when not correctly predicted based on the history and standard physical exam – made no difference in the patients’ ED management. In the subgroup of 24 patients who were admitted, only one had a pelvic exam with an unexpected result that changed the clinical plan. This patient was admitted with a diagnosis (anemia) that was not made as a result of the pelvic exam. This suggests that even in sicker patients requiring hospital admission, the pelvic exam rarely changed clinical management.
To our knowledge this is the first study to prospectively evaluate the role of the pelvic exam in managing patients in the ED, but prior research has questioned the use of the exam in general. Close et al1 reported that the inter-rater reliability of ED physicians performing pelvic exams was poor: emergency physicians agreed on the presence of cervical motion tenderness only 17% of the time and of the presence of an adnexal mass only 23% of the time. Even under ideal exam conditions – an anesthetized patient being examined for an adnexal mass by a gynecologist – the pelvic exam had a positive predictive value of 0.26–0.69.2 Dart et al13 concluded that no constellation of physical findings could confirm or exclude the diagnosis of ectopic pregnancy with certainty. The claim that the pelvic exam is a reliable decision aid in ED patients with abdominal pain or bleeding has been called a “medical myth.”14 We believe that its role in the ED should be questioned still further as a result of our findings, but there are at least two ways to interpret our findings. The first is to conclude that since 6% of patients had a finding on pelvic exam that changed the clinical plan, the exam is important and needs to be performed in all patients with abdominal pain or vaginal bleeding. This position is not one that we entirely disagree with, and our findings do not suggest that the exam is to be entirely discarded in the ED. Rather, the results suggest the possibility that in many, or perhaps most patients, the exam added little or no new information beyond that already gathered by taking a medical history and performing a general physical exam. Another interpretation of our results is that since the pelvic exam changed the clinical management on only 6% of the cases, it should not simply be performed in all women with abdominal pain or vaginal bleeding. By analogy, in the early evaluation of the need to obtain radiographs in every patient with an acute ankle injury, one study found that the yield for clinically important fractures was 13%, leading the authors to conclude that there was a “great potential for a more efficient use of radiography in ankle injury, possibly through the use of guidelines.”15 The suggestion was not that radiographs are useless, but rather that there are clinical situations in which they could safely be avoided. We believe that our results suggest a similar possibility regarding the use of pelvic exams.
It is certainly not our suggestion that this exam is uniformly unimportant. The pelvic exam plays a vital role in the prevention and diagnosis of many diseases, and as such must be part of every physician’s skill set. Our findings do not suggest that women do not require a pelvic exam as part of their comprehensive health exam and have no bearing on the use of the pelvic exam as part of routine pre-or post-natal care. Our study addresses the role of this exam in the evaluation of women with undifferentiated abdominal or pelvic pain, as well as vaginal bleeding in the context of the ED. It is in this set of patients – those who formed the subjects in our prospective study – that the pelvic exam rarely changed the clinical plan that had already been made, based on information from the history and general physical exam. Of course the predictability of exam findings does not always mitigate the necessity of their verification. However, when this verification comes at an emotional cost or is accompanied by significant operational challenges, its necessity should be reconsidered.
Several reasons support the reevaluation of the need for a pelvic examination for every woman in the ED with abdominal pain. As we have already mentioned, logistic considerations make the exam both time consuming and labor intensive. The number of rooms in which a pelvic exam may be performed is usually limited to one or two in a typical ED, and it is often the case that several patients need to be moved in order for a room to become available. Moreover, some findings – such as adnexal tenderness or cervical motion tenderness – are often non-specific, and their presence or absence does not allow the ED physician to conclude with confidence that pelvic pathology (as opposed to an abdominal pathology) is present or absent. Finally, there is good evidence that the pelvic exam is both physically uncomfortable and emotionally distressing for many women. There have been various interventions studied with the aim of reducing the physical and psychological distress of the exam. These have tested alternative positions, foot rests, and using different types of gowns.5,16,17 Despite these and other efforts, however, the exam remains uncomfortable: 41% of women who underwent a pelvic exam in the ED described the exam as being either moderately or severely painful.18
LIMITATIONS
Like any clinical study, our methods have limitations. First, we did not ask the providers to specify their management plan prior to or following the completion of the pelvic exam. Rather, providers were asked a more general question of whether the exam changed their management, without specifying the changes that may have occurred. Secondly, we did not record the way in which any unexpected finding changed the plan. As a result, we are not able to determine how particular unexpected findings correlate with any change in management. Finally, we used no objective criteria to determine the need for cervical cultures, and this group was excluded from the analysis. Despite these limitations we believe our study raises some important questions about the role of a routine pelvic exam in the ED.
CONCLUSION
In this pilot study of women with acute abdominal pain or vaginal bleeding in the ED, the pelvic exam rarely offered additional information beyond that already obtained by history and a general physical exam. Further work with a larger sample of patients should be undertaken to determine if these results are valid in other ED settings, and if there is a group of women with abdominal pain or vaginal bleeding in whom the pelvic exam may safely be omitted. In its evaluation of the United States healthcare system in the twenty-first century, the Institute of Medicine identified both the provision of effective services and respect for a patient’s physical comfort and preferences as two of its six core aims.19 Reevaluating the importance of performing a pelvic exam in every woman with acute abdominal pain would certainly be in keeping with these recommendations.
Footnotes
Supervising Section Editor: Judith R. Klein, MD
Submission history: Submitted: January 1, 2010; Revision received February 26, 2010; Accepted June 14, 2010.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: Jeremy Brown, MD, Department of Emergency Medicine, The George Washington University Medical Center, 2150 Pennsylvania Ave., Washington DC 20037
Email: jbrown@mfa.gwu.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Close RJ, Sachs CJ, Dyne PL. Reliability of bimanual pelvic examinations performed in emergency departments. West J Med. 2001;175:240–4. [PMC free article] [PubMed]
2. Padilla LA, Radosevich DM, Milad MP. Accuracy of the pelvic examination in detecting adnexal masses. Obstet Gynecol. 2000;96:593–8. [PubMed]
3. Larsen M, Oldeide CC, Malterud K. Not so bad after all…, Women’s experiences of pelvic examinations. Fam Pract. 1997;14:148–52. [PubMed]
4. Moettus A, Sklar D, Tandberg D. The effect of physician gender on women’s perceived pain and embarrassment during pelvic examination. Am J Emerg Med. 1999;17:635–7. [PubMed]
5. Seymore C, DuRant RH, Jay MS, et al. Influence of position during examination, and sex of examiner on patient anxiety during pelvic examination. J Pediatr. 1986;108:312–7. [PubMed]
6. Seehusen DA, Johnson DR, Earwood JS, et al. Improving women’s experience during speculum examinations at routine gynaecological visits: randomised clinical trial. BMJ. 2006;333:171.[PMC free article] [PubMed]
7. Tintinalli JE, Kelen GD, Stapczynski JS. American College of Emergency Physicians Emergency medicine : a comprehensive study guide. 5th ed. New York: McGraw-Hill, Health Professions Division; 2000.
8. Edelman A, Anderson J, Lai S, et al. Videos in clinical medicine. Pelvic examination. N Engl J Med.2007;356:e26. [PubMed]
9. Townsend CM, Beauchamp RD, Evers M, et al. Sabiston textbook of surgery : the biological basis of modern surgical practice. Philadelphia: Saunders; 2004.
10. Norton J, Bollinger RR, Chang A, et al. Surgery: Basic science and clinical evidence. New York: Springer; 2001.
11. Corson JG, Williamson R, et al. Surgery. London: Mosby; 2001.
12. Macdonald JW. A clinical textbook of surgical diagnosis and treatment. Philadelphia: W. B. Saunders; 1898.
13. Dart RG, Kaplan B, Varaklis K. Predictive value of history and physical examination in patients with suspected ectopic pregnancy. Ann Emerg Med. 1999;33:283–90. [PubMed]
14. Brown T, Herbert ME. Medical myth: Bimanual pelvic examination is a reliable decision aid in the investigation of acute abdominal pain or vaginal bleeding. CJEM. 2003;5:120–2. [PubMed]
15. Stiell IG, McDowell I, Nair RC, et al. Use of radiography in acute ankle injuries: physicians’ attitudes and practice. CMAJ. 1992;147:1671–8. [PMC free article] [PubMed]
16. Olson BK. Patient comfort during pelvic examination. New foot supports vs metal stirrups. JOGN Nurs. 1981;10:104–7. [PubMed]
17. Williams JG, Park LI, Kline J. Reducing distress associated with pelvic examinations: a stimulus control intervention. Women Health. 1992;18:41–53. [PubMed]
18. Patton KR, Bartfield JM, McErlean M. The effect of practitioner characteristics on patient pain and embarrassment during ED internal examinations. Am J Emerg Med. 2003;21:205–7. [PubMed]
19. Institute of Medicine Committee on quality of health care in America: crossing the quality chasm.Washington DC: National Academy Press; 2001.


