| Author | Affiliation |
|---|---|
| Dilani Weerasuriya, MD | Department of Emergency Medicine, Emory University, Atlanta, Georgia |
| Sophia Sheikh, MD | Department of Emergency Medicine, Emory University, Atlanta, Georgia Georgia Poison Control, Atlanta, Georgia |
| Brent W. Morgan, MD | Department of Emergency Medicine, Emory University, Atlanta, Georgia Georgia Poison Control, Atlanta, Georgia |
ABSTRACT
Introduction:
Self-exposure is a leading method for suicide both in the United States and worldwide and thus is a major preventable public health issue. Surrogate decision makers are tasked with making medical decisions for the patient while keeping the patient’s wishes in mind. Decisions related to code status become more complicated when the patient’s situation is the result of a suicidal act. The objectives were to 1) determine how frequently Do Not Resuscitate orders (DNR orders) are placed for the intentionally self-exposed (ISE) patient using the Regional Poison Control Center (RPCC) data, and 2) identify if DNR orders in intentionally self-exposed patients were placed before or after development of poor prognostic signs.
Methods:
We analyzed all exposure-related deaths reported to the RPCC from January 1, 2000 to December 31, 2010. We reviewed data for the following: exposure intent, exposure substance, outcome, age, code status, date of DNR/withdrawal of care order, previous suicide attempts, and poor prognostic signs.
Results:
Of the 476 total deaths, nearly half were the result of an intentional self-exposure (n= 235; 49.4%). Most deaths, when code status was reported, had advanced cardiac life support, or “full codes” (n=131; 55.6%). Of the total deaths with a DNR or withdrawal of care order (n=104), over half were from an ISE (n=55; 52.9%). A higher percentage of the ISEs had a DNR order/withdrawal of care order; however, it was not a statistically significant difference OR 1.23 (95% CI 0.64, 2.37). of intent, patients treated as full codes were on average 19.5 years younger than the DNR orders group. Only 2 DNR orders were placed prior to development of poor prognostic signs. Unintentional self-exposures consumed a mean of 1.4 substances (range 1 to 4). ISEs consumed a mean of 2.3 substances (range 1 to 19).
Conclusion:
People are often asked to make life-and-death decisions for a loved one. The nature of the exposure can complicate the issue if the exposure has an antidote or is known to have a limited effect. Further study is needed to assess the extent of these cases and to identify optimal management guidelines or policy to aid both the medical teams caring for these patients and the surrogate decision makers.
INTRODUCTION
Death by suicide has increased 60% over the past several decades and is one of the top 3 causes of death in those younger than 44 years in many countries.1 It is the 10th most common cause of death in the United States. Self-poisoning is a leading method for suicide both in the U.S. and worldwide and thus is a major preventable public health issue.2–4
Care of the severely ill patient, whose ability to communicate is impaired, is dictated by the medical team and the patient’s surrogate decision makers (family members, legal guardians, etc). In most situations, surrogate decision makers are tasked with making medical decisions for the patient while keeping the patient’s wishes in mind. In one study of 668 Do-Not-Resuscitate (DNR) patients (none were self-poisonings), most of the DNR orders were placed solely by a surrogate decision maker (n=389; 58%) and a substantial number by both the patient and the surrogate decision maker (n=88; 13%).5 Not surprisingly, surrogate decision makers took significantly longer to reach a decision compared to patients (6.6 days versus 3.2 days).5 Decisions related to code status, however, become more complicated when the patient’s situation is the result of a suicidal act. Case reports describe patients who place DNR orders prior to attempting suicide to prevent institution of life-saving medical treatment.6,7In a chart review of 191 hospitalized geriatric patients with major depressive disorder or bipolar disorder, close to half wanted to have a DNR order (n=91; 48%). Patients with suicidal ideation (n=50; 26%) were significantly more likely to choose to have a DNR order (60% versus 43%).8 How should prior DNR orders be handled in this unique population? Are surrogate decision makers for the self-poisoned patient more likely to place DNR orders since they are tasked with thinking of the patient’s wishes? Should a DNR order placed by the surrogate decision makers be upheld when effective treatment for the poisoning is available?
The latter question was raised by a unique case reported to the Regional Poison Control Center (RPCC). A depressed male ingested a large amount of alprazolam in a suicide attempt. During his hospital course, the patient developed respiratory depression requiring ventilator support. His family, however, refused intubation and requested a DNR order out of respect for the patient’s wishes as he had multiple previous suicide attempts. This decision prompted his nurse to call the RPCC to inquire about treatment options and guidance on how to handle the situation. The RPCC suggested discussing the temporary nature of his current condition with his family as the mental and respiratory suppression caused by the alprazolam could be treated until the medication was fully eliminated from the body. However, his family kept the DNR order in place and the patient remained unsupported and died. This case, like others reported in the literature, posed challenging ethical dilemmas for the family and the treating medical team. The frequency of these cases and the best management approach is unknown.
The objectives of this study were to 1) determine how frequently DNR orders are placed in the intentionally self-exposed patient using RPCC data; and 2) identify if the DNR order in the intentionally self-exposed patient was placed before or after development of poor prognostic signs.
METHODS
An exposure was defined as contact (ingestion, inhalation, dermal contact, or injection) with a substance foreign to the human body. Intentional self-exposure was defined as an exposure related to a foreign substance with intent to harm oneself. Unintentional self-exposure was defined as an exposure related to a foreign substance without intent to harm oneself. Malicious exposure was defined as an intentional exposure in a patient by an individual with intent to harm the patient. We analyzed all exposure-related deaths reported to the RPCC from January 1, 2000, to December 31, 2010. A trained coder reviewed the data for the following variables: exposure intent, exposure substance, outcome, age, code status, date of DNR/withdrawal of care order, and previous suicide attempts. The presence of poor prognostic signs, including ventilator support, use of vasopressors, severe acidosis (defined as pH<7 or bicarbonate <5), and poor neurologic function, was also recorded by the reviewer from RPCC data, if available. If prognostic signs were reported, the reviewer would determine whether the signs were present before or after determination of code status. We performed statistical analysis using Microsoft Excel 2007.
RESULTS
Table 1 shows the distribution of RPCC patient deaths by exposure intent and code status. Most of the 476 total deaths were the result of intentional self-exposures (n= 235; 49.4%). Nearly half had a reported code status (n=236; 49.6%). From those with a known code status, the majority were treated as full codes (n=131; 55.6%). Over half of the total deaths with a DNR or withdrawal of care order (n=104) were the result of an intentional self-exposure (ISE) (n=55; 52.9%). Ethnicity was not reported because it was not recorded in the RPCC data.
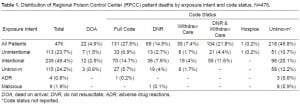
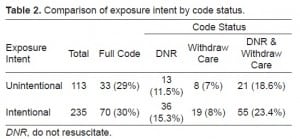
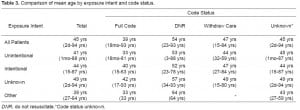
Table 2 compares exposure intent by code order status. A slightly higher percentage of ISE had a post-exposure DNR order; however, this difference was not statistically significant, OR 1.23 (95% CI 0.64, 2.37). In other words, intentional exposures did not have statistically significant higher odds of having a DNR order placed than unintentional self-exposures. Table 3 details the mean age of patients by exposure intent and code status. Regardless of intent, patients in whom advanced cardiac life support (full codes) was used were on average 19.5 years younger than the group in which it was not (the DNR group).
Only 2 DNRs were placed prior to development of poor prognostic signs, 1 of which was coded as intent unknown and the other as suspected ISE. The latter case involved a female who reportedly mistook paraquat for Robutussin. The only symptom at time of DNR order placement was oral swelling.
The most common exposure reported in the DNR group was acetaminophen for both the intentionally and unintentionally self-exposed groups. In those treated as full codes, anticonvulsant medications were the most common exposures reported for the intentionally exposed group and stimulant/street drugs were the most frequent exposures reported in the unintentionally exposed group. Patients with unintentional self-exposures consumed a mean of 1.4 substances per individual (range 1 to 4). Patients with ISEs consumed a mean of 2.3 substances per individual (range 1 to 19).
DISCUSSION
Regarding our first objective, to determine how frequently DNR orders are placed in the ISE patient, we found that DNR orders are not placed significantly more often than in the unintentionally self-exposed patient. One explanation for the slightly increased incidence of DNR orders in those with ISEs is that these patients tended to consume nearly double the amount of toxic substances as the unintentionally self-exposed. Thus, it is reasonable to suppose that these individuals tended to be more symptomatic, thereby leading their families to request DNR orders based not on the patients’ wishes, but rather on the poor prognosis of meaningful recovery. This is supported by our finding that the overwhelming majority (98%) of DNR and withdrawal of care orders were placed after poor prognostic factors were apparent, thus fulfilling our second objective of identifying when the DNR order in the intentionally self-exposed patient is typically placed.
Surrogate decision makers for the ISE are faced with difficult decisions. They are instructed to keep the patient’s wishes in mind when making medical decisions while knowing that their loved one wanted to die. They report many negative feelings, including guilt, ambivalence, and conflict.9 Surrogate decision makers may be influenced by several other factors as well, such as: 1) their own morals and beliefs on life and suicide; 2) personal guilt for not being able to help the patient; 3) fear of making medical decisions friends and other family may not agree with; 4) society’s views on suicide; and 5) hopelessness. One study found that multiple DNR orders were placed by family members who felt unable to cope with the psychological stress of having a suicidal family member.10 Since most of the ISE patients were treated as full codes (had advanced cardiac life support), it is apparent that factors other than the patient’s implied wishes are playing a major role in the surrogate’s decision. Additionally, our finding that the group who received advanced cardiac life support tended to be significantly younger than the average age of the group that did not receive it lends further support to the idea that the decisions of the surrogate are motivated by reasons external to those of the patient. A similar age-based bias was found by Fader et al.11
LIMITATIONS
Our results are limited by factors inherent to poison center data, such as incomplete data reporting and documentation. Additional limitations include convenience sampling and selection bias, as only cases reported to the RPCC were available for analysis.
CONCLUSION
Making life and death decisions for a loved one is stressful. Such decisions become extremely complex when compounded with the knowledge that the family’s loved one chose suicide. The nature of the exposure can further complicate the issue if the exposure has an antidote or is known to exert its effects for a limited time. While the majority of deaths reported to the poison center were managed as full codes, the frequency with which cases of ISE have DNR orders placed is high. Further study is needed to fully assess the extent of these cases and to identify optimal management guidelines or policy to aid both the medical teams caring for these patients and the surrogate decision makers. Such guidelines should address the following questions: Is a DNR order appropriate when an exposure is reversible? How are ISE individuals with prior DNR orders to be managed? When is a DNR order appropriate in the ISE? Should surrogate decision makers be offered counseling prior to making such decisions?
Footnotes
Supervising Section Editor: Abigail Hankin, MD, MPH
Submission history: Submitted January 4, 2012; Revision received March 12, 2012; Accepted March 14, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.11725
Address for Correspondence: Dilani Weerasuriya, MD
Emory University, 425 Chapel St. SW #1412, Atlanta, Georgia, 30313
Email: dweeras@emory.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. World Health Organization Suicide Prevention. Available at:http://www.who.nt/mental_health/prevention/suicide/suicideprevent/en/. Last accessed November 28, 2011.
2. National Institute of Mental Health Suicide in the U.S.: Statistics and Prevention. Available at:http://www.nimh.nih.gov/health/publications/suicide-in-the-us-statistics-and-prevention/index.shtml. Last accessed November 28, 2011.
3. National Center for Injury Prevention and Control Suicides due to Alcohol and/or Drug Overdose. Available at: http://www.cdc.gov/violenceprevention/pdf/NVDRS_Data_Brief-a.pdf. Last accessed November 28, 2011.
4. Ajdacic-Gross V, Weiss MG, Ring M, et al. Methods of suicide: international suicide patterns derived from the WHO mortality database. Available at: http://www.who.int/bulletin/volumes/86/9/07-043489/en/. Last accessed 11/28/11.
5. Torke AM, Sachs GA, Heift PR, et al. Timing of do-not-resuscitate orders for hospitalized older adults who require a surrogate decision maker. J Am Geriatr Soc. 2011;59(7):1326–31. [PMC free article][PubMed]
6. Cook R, Pan P, Silverman R, et al. Do-not-resuscitate orders in suicidal patients: clinical, ethical, and legal dilemmas. Psychosomatics. 2010;51(4):277–82. [PubMed]
7. Sontheimer D. Suicide by advance directive? J Med Ethics. 34(9):e4. [PubMed]
8. Lifton I, Kettle P. Suicidal ideation and the choice of advance directives by elderly persons with affective disorders. Psychiatric Services. 2000;51(11):1447–9. [PubMed]
9. Handy C, Sulmasy D, Cindy M, et al. The surrogate’s experience in auizing a do not resuscitate order.Palliative and Supportive Care. 2008;6:13–19. [PubMed]
10. Wasserman D. Passive euthanasia in response to attempted suicide: one form of aggressiveness by relatives. Acta Psychiatrica Scandinavica. 1989;79(5):460–467. [PubMed]
11. Fader A, Gambert S, Nash M, et al. Implementing a “Do-Not-Resuscitate” (DNR) policy in a nursing home. Journal of the American Geriatrics Society. 1989;37(6):544–548. [PubMed]


