| Author | Affiliation |
|---|---|
| Melissa Givens, MD, MPH | Carl R. Darnall Army Medical Center |
| Kristine Kalbfleisch, MD, MS | Carl R. Darnall Army Medical Center |
| Scott Bryson, MD | Carl R. Darnall Army Medical Center |
ABSTRACT
Introduction:
Methanol poisoning by ingestion is well represented in current emergency medicine literature. Much less described, however, is poisoning via intentional inhalation of methanol-containing products such as carburetor cleaner. This study intends to explore the exposure routes and treatment patterns of methanol cases reported to Texas Poison Centers.
Methods:
All cases of methanol exposures from January 2003 to May 2005 were collected from the Texas Poison Center Network database “Toxicall.” Inclusion criteria were 1) methanol as primary exposure, and 2) documented route of exposure. Exclusion criteria were unknown, dermal, and eye exposures. Data was extracted from documented calls to Texas Poison Centers and analyzed using descriptive statistics.
Results:
A total of 203 cases were collected from 6 regional Poison Centers. Eighty seven cases had inhalation as the route of exposure, while 81 were methanol ingestions. Carburetor cleaner was responsible for nearly all the inhalational cases (79/87) while ingestions involved mostly windshield washer fluid (39/81) and carburetor cleaner (20/81). Seventy-eight percent of the inhalational exposures were intentional while most of the ingestions were accidental (49/75) and suicidal (18/75). An anion gap was documented in 31 of the inhalational cases and in 10 of the ingestions. Dialysis, use of fomepizole, and vision loss were documented for both types of exposure. Fifty-six percent of the inhalational group was admitted compared to 46% of the ingestion group.
Conclusion:
We propose that the results obtained from our review show inhalational exposure involving methanol (e.g., “huffing”) represents a significant source of toxicity in the studied population. This is in contrast to previous literature that proposed inhalational toxicity was rare and aggressive treatment usually not necessary in cases of inhalation of methanol-containing carburetor cleaners.
INTRODUCTION
When speaking of methanol exposures, most emergency physicians have experience with ingestions of methanol-containing products. However, inhalational abuse of carburetor cleaner and other volatile products containing methanol represents a non-trivial source of methanol exposure not commonly described in emergency medicine textbooks. Methanol is a colorless, volatile alcohol commonly used commercially in industrial solvents and products such as windshield washer fluid, glass cleaners, antifreeze, carburetor cleaners, canned solid fuels (e.g., Sterno®), and small engine fuels. It is a common source of both intentional and accidental poisoning because of its widespread availability. Methanol is oxidized to formaldehyde by alcohol dehydrogenase (ADH) and then to formic acid by aldehyde dehydrogenase. Formic acid is primarily responsible for most of the serious sequelae observed in methanol toxicity, including metabolic acidosis and visual disturbances.1,2 Methanol poisoning by ingestion commonly presents with gastrointestinal complaints due to mucosal irritation including nausea, vomiting, and abdominal pain. All exposure routes lead to central nervous system (CNS) depression, confusion and ataxia. The syndrome can progress to development of an uncompensated anion gap metabolic acidosis, brain lesions, and visual impairment, which can range from blurred vision to visual field deficits to total blindness.
Importance of the Topic
Epidemic poisonings from methanol exposure are sporadic. In 2005, of the 807 cases of methanol poisoning reported to American poison centers, 80% were unintentional, 4% had major complications and six resulted in fatalities.3 Treatment delay is associated with increased morbidity, making early recognition of clinical and laboratory clues crucial. Intentional inhalation of volatiles, including methanol-containing products, is increasing in prevalence, especially among adolescents.4–7 Long-term inhalant abuse is associated with violence, major depression, polysubstance abuse, and suicidality.8,9 This has far-reaching implications to society in general and to the emergency department (ED) as we treat significant toxicity in this growing demographic.
Goals of the Investigation
Poisoning by ingestion of methanol-containing products is well represented in the current body of medical literature; however, there is a paucity of literature dealing with their inhalation. Information is limited to a handful of small studies and case reports with mixed conclusions. Some report that methanol toxicity by inhalation or ingestion is equally dangerous, while others assert that inhalation does not result in serious toxicity.10–14 The goals of this investigation are to contribute evidence that toxicity from inhalation of methanol-containing products is both more common and more dangerous than previously thought and to explore the exposure routes and treatment patterns of methanol cases reported to Texas Poison Centers.
METHODS
A retrospective chart review was performed using the Texas Poison Control Center Network database, “Toxcall”®. All cases of methanol exposures from January 2003 to May 2005 were collected. Inclusion criteria were 1) methanol exposures, and 2) documented route of exposure. Exclusion criteria were unknown, dermal, and eye exposures. Data were extracted using a standardized data collection instrument by two independent investigators and reviewed for discrepancies. If a discrepancy occurred, the original chart was reviewed by both investigators to correct the discrepancy. Data were extracted from documented calls to Texas Poison Centers and analyzed using descriptive statistics. Database was managed and analyzed using Microsoft Office Excel® 2007.
Important endpoints included the type of product/exposure source (e.g., carburetor cleaner vs. windshield wiper fluid), categorization of route of exposure (e.g., inhalation vs. ingestion), age of the exposed, and whether the exposure was intentional abuse (e.g., abused for intoxication purposes), accidental, or for a suicidal intent. The endpoints of toxicity included methanol level (if measured), the presence of an anion-gap acidosis (anion gap >12mEq/L), visual disturbances (to include any change in vision documented in the chart), the need for ethanol, fomepizole treatment and/or hemodialysis, and final ED disposition (e.g. need for admission). If endpoints were not documented in the chart then data were reported as “unknown.”
RESULTS
A total of 203 cases were collected from six regional poison centers. Eight unknown exposures, five dermal, and 22 eye exposures were excluded. Eighty-seven of the remaining cases were inhalational and 81 were ingestions. Carburetor cleaner was responsible for nearly all the inhalational cases (79/87). The remaining inhalational cases were unknown products (6) or windshield washer fluid (2). Ingestions involved mostly windshield washer fluid (39/81) and carburetor cleaner (20/81), with 11 remaining cases from miscellaneous sources such as Sterno® and brake fluid and 11 cases from unknown products.
The mean age of the ingestion group was 19 (range <1 to 70 years, with 12 patients under the age of six), while the mean age of the inhalation group was 28 (range 2–62 years with one patient under the age of six). Seventy-one percent (62/87) of the inhalational group was male, and 88% (71/81) of the ingestion group was male. Eighty percent of known cases (66/83) of the inhalational exposures were intentional abuse cases, while 8 were suicidal, 9 accidental, and 4 unknown. Most of the known cases of ingestions were accidental (49/75) and suicidal (18/75) with the remaining attributable to intentional abuse (8) and unknown (6).
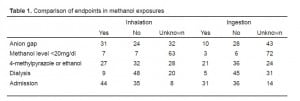
The mean pH for the inhalation group was 7.24 (95% CI 7.19 – 7.29) and for the ingestion group was 7.33 (95% CI 7.27–7.37). Arterial or venous source of pH was not explicitly queried. Six patients in the inhalational group suffered visual loss and two in the ingestion group. Other endpoints are described in Table 1.
DISCUSSION
Although awareness of acute toxicity from methanol ingestion has been highlighted for years in Emergency Medicine literature, this is one of the few studies looking at inhalational exposures. In 2002 Barceloux et al.1 reported that “almost all cases of acute methanol toxicity result from ingestion, though rarely cases of poisoning have followed inhalation or dermal absorption.” The results obtained from our retrospective chart review demonstrate an increased trend of inhalational exposure involving methanol (i.e., “huffing”), and the critical clinical manifestations of methanol toxicity and evidence of poisonings from an inhalation-exposure route.
A case report published in Annals of Emergency Medicine in 1990 described the “unusual presentation of solvent abuse” in a 17-year-old male who appeared intoxicated after inhaling a rag soaked with carburetor cleaner containing methanol, toluene and methylene chloride.14 Additionally, in 1993 Frenia and Schauben10 reported in Annals of Emergency Medicine of seven cases of intentional inhalation abuse of carburetor cleaner, containing methanol, toluene, methylene chloride and propane. These cases experienced CNS depression, visual disturbance (one case), death (one case), and acidosis requiring treatment with leucovorin and/or folate, ethanol infusions, reversal of acidosis and even hemodialysis (three cases). The results of our retrospective chart review build upon these reports to provide an even larger number of patient study subjects inhaling methanol (87) with 80% of those cases defined as “intentional abuse” exposures. These cases were compared to ingestion exposure subjects (81) defined as accidental (60%) or suicidal (22%). Our study too showed that the most popular methanol-containing product involved in inhalational cases was carburetor cleaner (97%).
Carburetor cleaner contains other compounds that may contribute to toxicity. Common ingredients that often comprise more than 50% of the listed ingredients in carburetor cleaners include toluene, xylene, acetone, and naphtha; however, this list is not all-inclusive. Mixtures of various hydrocarbons make up smaller percentages of ingredients. Methanol content varies based on manufacturer. The hydrocarbon component of carburetor cleaners can be expected to contribute to toxicity. Inhalation of hydrocarbons may cause pulmonary toxicity, CNS symptoms (sedation, agitation, seizures, ataxia) and cardiac dysrythmias. Toluene deserves specific mention as it can cause renal tubular acidosis with chronic exposure. Toluene may also contribute a small amount to an anion gap metabolic acidosis since it is metabolized to hippuric acid.
A recent retrospective poison center chart review summarized 22 cases and reported that “significant toxicity following inhalation of methanol containing carburetor cleaners was rare with symptoms improving without aggressive care (e.g., dialysis, ADH blockade).”12A more recent prospective observational study on seven patients after inhalant abuse of methanol-containing hydrocarbon products preliminarily concluded that “inhalant abusers of methanol products may have significantly elevated methanol and formic acid levels, but are at low risk for methanol induced complications of visual dysfunction and refractory acidosis.”13
Our data appear to refute these conclusions. Many of our inhalation exposure patients developed an anion gap metabolic acidosis, needed dialysis or treatment with ethanol or fomepizole, developed visual loss and required admission to the hospital. The trends observed in our study should remind us to maintain our awareness and aggressiveness of treatment of the acutely intoxicated patient to prevent the potential significant toxic sequelae that can result from the inhalation of methanol-containing products.
LIMITATIONS
Several limitations exist in our study. It is performed on only the patient population reported through the poison control system and thus is vulnerable to the inherent limitations of poison center data. Data are collected by specialists in poison information (SPI) by phone calls from the facility where the patient is receiving care. Data may be collected from nurses or physicians and are dependent on the information offered by those involved in the care of the patients and the thoroughness of the query by the SPIs. Due to the limitations of data collection in these patients, we did not do any further statistical testing other than descriptive statistics. Poison center cases are limited to those voluntarily reported by the individual or health care facilities. There could be cases that are never diagnosed or reported, which could contribute to the underestimation of this exposure. In addition, the ingestion route of exposure may be overestimated from the large number of accidental cases reported and are a result of small amounts ingested, and therefore nontoxic. One major limitation of the study that may overestimate the toxicity of the inhalational exposures is the fact that the source products contain several co-ingestants/chemicals (e.g., methylene chloride, toluene, etc.) which may be contributing to the endpoints of toxicity.
CONCLUSION
Our results indicate that inhalational exposure involving methanol represents a significant source of toxicity in the studied population. These results contrast with previous literature that proposed inhalational methanol toxicity was rare and aggressive treatment usually not necessary in cases of inhalation of methanol containing carburetor cleaners.
Footnotes
Supervising Section Editor: Jeffrey R. Suchard, MD
Submission history: Submitted February 20, 2008; Revision Received April 4, 2008; Accepted April 7, 2008.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Melissa Givens, MD MPH, Department of Emergency Medicine, 36000 Darnal Loop, C.R. Darnall Army Medical Center, Fort Hood TX 76548
Email: Melissa.givens@us.army.mil
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA. American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol. 2002;40(4):415–46. [PubMed]
2. Hantson PE. Acute methanol intoxication: physiopathology, prognosis and treatment.Bull Mem Acad R Med Belg. 2005;160(5–6):294–300. [PubMed]
3. Lai M, Klein-Schwartz, Rodgers G, et al. 2005 Annual report of The American Academy of Poison Control Centers national poisoning and exposure database. Clin Toxicol.2006;44(6–7):803–892.
4. Kavet R, Nauss KM. The toxicity of inhaled methanol vapors. Crit Rev Toxicol.1990;21(1):21–50. [PubMed]
5. Wu LT, Ringwalt CL. Inhalant use and disorders among adults in the United States.Drug Alcohol Depend. 2006 Oct 15;85(1):1–11. Epub 2006 Apr 3. [PMC free article][PubMed]
6. Chepesiuk R. Resurgence of teen inhalant use. Environ Health Perspect. 2005 Dec;113(12):A808.
7. Neumark YD. The epidemiology of adolescent inhalant drug involvement. Arch Pediatr Adolesc Med. 1998 August 1;152(8):781–6. [PubMed]
8. Fleschler MA, Tortolero SR, Baumler ER, Vernon SW, Weller NF. Lifetime inhalant use among alternative high school students in Texas: prevalence and characteristics of users.Am J Drug Alcohol Abuse. 2002;28(3):477–95. [PubMed]
9. Sakai JT, Hall SK, Mikulich-Gilbertson SK, Crowley TJ. Inhalant use, abuse, and dependence among adolescent patients: commonly comorbid problems. J Am Acad Child Adolesc Psychiatry. 2004 Sep;43(9):1080–8. [PubMed]
10. Frenia ML, Schauben JL. Methanol inhalation toxicity. Ann Emerg Med. 1993 Dec;22(12):1919–23. [PubMed]
11. Winnik L, Radomska M, Wos M, Pach D. The CNS damage due to methanol poisoning in the case of 23. year-old male patient addicted to organic solvents. Przegl Leki.2005;62(6):511–3.
12. LoVecchio F, Sawyers B, Thole D, Beuler MC, Winchell J, Curry SC. Outcomes following abuse of methanol-containing carburetor cleaners. Hum Exp Toxicol. 2004 Oct;23(10):473–5. [PubMed]
13. Bebarta VS, Heard K, Dart RC. Inhalational abuse of methanol products: elevated methanol and formate levels without vision loss. Am J Emerg Med. 2006 Oct;24(6):725–8. [PubMed]
14. McCormick MJ, Mogabgab E, Adams SL. Methanol poisoning as a result of inhalational solvent abuse. Annals of Emergency Medicine. 1990 Jun;19(6):639–42. [PubMed]