| Author | Affiliation |
|---|---|
| Heather Groth, MD | University of Virginia, Department of Emergency Medicine, Charlottesville, Virginia |
| Hans House, MD | University of Iowa, Department of Emergency Medicine, Iowa City, Iowa |
| Rachel Overton, MD | La Crosse-Mayo Clinic, Department of Family Medicine, La Crosse, Wisconsin |
| Eric DeRoo, MD | University of Indiana, Department of Urology, Indianapolis, Indiana |
ABSTRACT
Introduction:
The American College of Emergency Physicians (ACEP) endorses emergency medicine (EM) residency training as the only legitimate pathway to practicing EM, yet the economic reality of Iowa’s rural population will continue to require the hiring of non-EM trained physicians. The objective of our study is to better understand the current staffing practices of Iowa emergency departments (EDs). Specifically, we seek to determine the Iowa community size required to support hiring an emergency physician (EP), identify the number of EDs staffed by advanced practice providers (APPs) in solo coverage in EDs, determine the changes in staffing over a 4-year period, and understand the market forces that contribute to staffing decisions.
Methods:
Researchers surveyed all 119 hospitals throughout the state of Iowa regarding their ED hiring practices, both in 2008 and 2012. From these data, we determined the mean population that supports hiring EPs and performed a qualitative examination of the reasons given for hiring preferences.
Results:
We found that a mean population of approximately 85,000 is needed to support EP-only staffing practices. In 2012, only 14 (11.8%) of Iowa’s EDs were staffed exclusively with EPs. Seventy-two (60.5%) staff with a combination of EPs and FPs, 33 (27.7%) staff with FPs alone, and 72 (60.5%) have physician assistants or nurse practitioners working in solo coverage for at least part of the week. Comparing the data from 2008 and 2012, there is no statistical change in the hiring of EPs versus FPs over the 4 years (Chi-square 0.68, p=0.7118), although there is a significant increase in the number of APPs in solo practice (Chi-square 11.36, p= 0.0008). Administrators at hospitals cited several factors for preferring to hire EPs: quality of care provided by EPs, availability of EPs, high patient acuity, and high patient volume.
Conclusion:
Many EDs in Iowa remain staffed by family medicine-trained physicians and are being increasingly staffed by APPs. Without the contribution of family physicians, large areas of the state would be unable to provide adequate emergency care. Board-certified emergency physicians remain concentrated in urban areas of the state, where patient volumes and acuity support their hiring.
BACKGROUND
The availability of emergency medical care is a worldwide necessity and the United States is no exception. As of 2008, there were 4,613 emergency departments (EDs) throughout the country, with over 36,000 physicians staffing these departments.1 Only a fraction of these EDs are staffed with board-certified emergency physicians (BC-EPs).2 Many hospitals hire family practice physicians (FPs) to help fill the staffing needs of their EDs. In fact, without the contribution of family physicians, large areas of the country would be unable to provide adequate emergency care. It is estimated that almost one third of emergency care is provided by family physicians and that 65% of family practitioners practice some type of emergency care.3 This is especially true in rural communities, where hospitals have smaller and less predictable patient volumes. Rural hospitals, where 42% of national EDs are located, are less likely to staff with an EP and more likely to staff their EDs with available family physicians.4
Likewise, nurse practitioners (NPs) and physician assistants (PAs) have been increasingly utilized in EDs. With the number of annual ED visits rapidly increasing, advanced practice providers (APP) have a larger role in the emergency medicine (EM) workforce. In one study, ED visits staffed by APPs increased from 4% of visits in 1993 to 12.9% of visits in 2005.5 Many of these visits are never staffed with a physician. In a different study, only 54.9% of APP cases were also seen by staff physicians.6Furthermore, many EDs have begun to staff with APPs in solo coverage for at least part of the week, particularly in rural areas.
EDs in Iowa have seen similar staffing trends. Being a predominantly rural state, Iowa has traditionally staffed its EDs with family medicine-trained physicians and has seen an increase in APP ED coverage. However, hospitals have been hiring more EPs over the past decade. The number of EPs increased with the founding of the state’s only emergency medicine residency program at The University of Iowa Hospitals and Clinics in 2003. Even with this recent increase, smaller communities continue to hire non-EPs to staff their EDs. In the most recent job bulletin distributed by the University of Iowa Carver College of Medicine, 32 communities were currently recruiting physicians for their EDs. Of these, only 6 specified that these opportunities were for EPs only.7Additionally, in a survey of hospital administrators throughout the country, the majority of urban administrators indicated that their hospital could attract and retain EPs, whereas the majority of rural administrators were certain their hospital could not retain such physicians.8 Concordantly, a survey of recent EM graduates suggested that factors which cause an EP to practice in a rural community are difficult to change (lifestyle factors, family connection, and access to specialists).9
While Iowa lacks current data concerning the penetration of EPs, other states have published this information. A study performed by The University of Nebraska Medical Center reported that 50.6% of physicians working in EDs in Nebraska, North Dakota, and South Dakota were EPs. The rural nature of the ED affected the proportion of EPs. Specifically, it was reported that 65.2% of urban hospitals were staffed with EPs, while only 30.8% of hospitals serving populations of less than 10,000 were so staffed.8 Similar statistics were reported in the states of New Mexico and West Virginia, where researchers found 35% and 12% of EDs staffed with EPs, respectively.10, 11 The study with a design most similar to ours was performed in the state of Washington in 1992. This study examined the staffing practices of rural hospitals, categorizing each hospital as staffing their EDs with local family physicians only (27%), visiting BC-EPs only (27%), and a variety of ED staffing combinations (46%).12
Staffing decisions for EDs are not based exclusively on population. The costs of running a small rural ED are significant, especially with low patient loads.12 These costs can lead to preferential hiring of FPs. However, studies have shown that in some EDs the switch to all EPs did not increase the cost of care, and further, that the number of tests ordered for each patient was actually reduced.13Malpractice is another issue that is very pertinent to ED staffing ,and one study of closed malpractice claims from a single insurer showed that the cost per physician per year of malpractice coverage was twice as high for non-EPs as compared to EPs.14 Moreover, hospitals with low patient acuity rates may choose to hire FPs instead of EPs.15
This previous research was performed in states other than Iowa. Thus, the purpose of this study was to describe the demographics of EM providers in Iowa and to identify the market forces influencing the hiring of FPs, EPs, NPs, and PAs. Specifically, we sought to determine the population necessary to support the employment of an EP in Iowa, identify the percentage of EDs staffed by APPs in solo coverage in EDs, and understand the rationale for hiring each type of ED provider.
METHODS
A telephone survey (Table 1) was given to administrators from all 119 hospitals with EDs in Iowa. This was performed once in 2008 and then repeated in 2012. The list of hospitals was obtained from the state medical society. Key measures included the preference in hiring within the specialty of EM and the factors that influence the tendency to hire EPs, FPs, and NPs and PAs. We stratified responses by hospital hiring profile: EP only, combination of EPs and FPs, and FP only. Using a chi-square test, we compared physician hiring practices (EP only, FP only, or both EP and FP) between 2008 and 2012. Similarly, we used a Pearson chi-square to compare the number of EDs hiring APPs in solo coverage between the 2 surveys. We determined the population of the area of care from the population as determined by the 2010 U.S. Census, and we determined a mean population to support hiring EPs only and both FPs and EPs from the data. Additionally, we conducted a qualitative analysis for each practitioner type, with the researchers asking questions regarding the market forces that influence hiring decisions, including quality of care provided, malpractice insurance rates, efficiency, salary, level of patient acuity, patient load, competition with other EDs, ability of physicians to generate higher billing, and availability of qualified applicants.
RESULTS
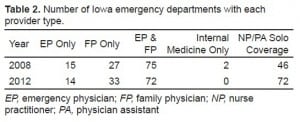
We received responses from all 119 hospitals in the state (100% response rate) in both 2008 and 2012. In 2012, only 14 (11.8%) of Iowa’s EDs exclusively staffed with EPs. Seventy-two (60.5%) hospitals staffed with a combination of EP and FP, while 33 (27.7%) of Iowa hospitals staffed with FP alone. We also found that 72 (60.5%) of Iowa’s EDs staffed with physician assistants or nurse practitioners as solo coverage during at least part of the work week. In 2008, 15 (12.6%) EDs were staffed with EPs only, 27 (22.7%) with FPs only, 75 (63.0%) with EPs and FPs, and 2 (1.7%) with internal medicine (IM) physicians only. Forty-six (38.7%) of the EDs were staffed with NPs or PAs in solo coverage in 2008 (Table 2). Using a Chi-Square test, we compared physician staffing practices (FP-only, EP-only, and both FP and EP) between 2008 and 2012. There is no significant difference between the two surveys, with a chi-square of 0.68 (P = 0.71). However, there is a significant increase in the number of PAs and NPs practicing in solo coverage in Iowa EDs (Chi-square 11.36, P = 0.0008).
Using the data from the 2012 survey, the mean population of communities supporting exclusive EP coverage was 84,787. The minimum population of a town supporting an EP-only ED was 2,968. The mean population that supports a combination of both EPs and FPs was 25,201. The minimum population of a town supporting both EPs and FPs was 1,691.
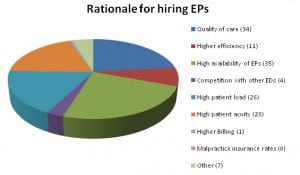
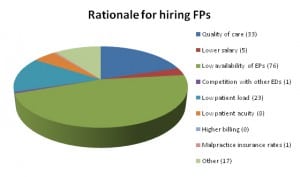
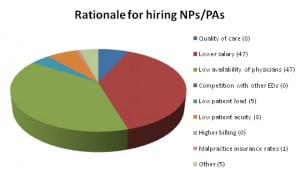
The most common reasons cited for staffing with FPs included the low availability of EPs,a low patient census that did not warrant EP specialty training, and hospital satisfaction with the quality of care provided by the local FPs (Figure 1). EDs that hired EPs cited factors that included the quality of care provided by EPs, the high availability of EPs, and a high patient and high patient census best supported by EPs (Figure 2). The most common reasons for hiring NPs and PAs in solo coverage were lower salaries and low availability of physicians (Figure 3).
DISCUSSION
We found that that in Iowa a mean population of approximately 85,000 is needed to support an EP-only ED. The minimum population was 2,968, representing the town of West Union, located in Northeast Iowa. A much lower mean population of approximately 25,000 was sufficient to support a combination of EPs and FPs. The minimum population required to support combined EPs and FPs was 1,691. We speculate that this relatively low population supported hiring EPs was because of the availability of staffing services.
Our research indicates that many EDs throughout Iowa rely on staffing services to supply physicians to provide care in their ED. At least 42 EDs use staffing services, and these services usually provide both EPs and FPs. Additionally, some staffing services hire other physician types and may hire APPs as well. The benefit of using these services is that they provide local physicians with much needed time off from ER call, and many hospitals stated that they used this fact as a recruiting tool.
Overall, there was no significant change in physician staffing of EDs in the state between 2008 and 2012. However, there was a large significant increase in the number of APPs. The number of EDs using NP/PAs in solo coverage increased by 56.5% between 2008 and 2012.
This study is limited in that it is a survey and relies on the accuracy of those responding to a research team. There was a great deal of heterogeneity in who responded to the survey. It was usually a non-physician hospital administrator, but the research team also heard from physician ED medical directors and the hospital directors of physician recruitment. The initial survey (2008) was conducted 4 years after the establishment of the EM residency at the University of Iowa and 1 year following the inaugural graduating class. Although the residency would not be expected to have a significant impact with only 12 total graduates, it would have been preferable to have a baseline survey in 2003 to measure the impact of attitudes toward EM as a specialty.
Certification by the American Board of Emergency Medicine (ABEM) has been the accepted standard to practice EM in the U.S.16 Since there are indications that the residency training site correlates with the choice of practice location, the addition of the state’s sole EM residency training program in 2003 may increase the hiring of EPs in rural Iowa.17 However, with the lack of change in EP hiring over the past 4 years, it seems likely that many EDs in this scarcely populated state will remain staffed by FM-trained physicians. In fact, without the contribution of family physicians, large areas of the state would be unable to provide adequate emergency care. Board-certified emergency physicians remain concentrated in more densely populated areas of the state, where patient volumes and acuity support their hiring.
Footnotes
Supervising Section Editor: Erik D. Barton, MD, MS, MBA
Submission history: Submitted June 8, 2012; Accepted August 30, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.8.12783
Address for Correspondence: Hans House, MD. University of Iowa, Department of Emergency Medicine, 200 Hawkins Drive, RCP 1008, Iowa City, IA 52242. Email: hans-house@uiowa.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hsia RY, Kellermann AL, Shen Y. Factors associated with closures of emergency departments in the united states. JAMA. 2011;305(19):1978–1985. [PubMed]
2. Williams AL, Blomkals AL, Gibler WB. Residency training in emergency medicine: the challenges of the 21st century. Keio J Med. 2004;53(4):203–209. [PubMed]
3. Bullock KA, Pugno PA, Gerard A. The role of family physicians in delivering emergency medical care. Am Fam Physician. 2008;77(2):148–149. [PubMed]
4. Wadman MC, Hoffman LF, Erickson T, et al. The impact of a rural emergency department rotation on applicant ranking of a US emergency medicine residency program. J Rural Remote Health.2007;7(4):686. [PubMed]
5. Ginde AA, Espinola JA, Sullivan AF, et al. Use of midlevel providers in US EDs, 1993–2005: implications for the workforce. Am J Emerg Med. 2010;28(1):90–94. [PubMed]
6. Menchine MD, Wiechmann W, Rudkin S. Trends in midlevel provider utilization in emergency departments from 1997 to 2006. Acad Emerg Med. 2009;16(10):963–969. [PubMed]
7. Office of Statewide Clinical Education, UI Carver College of Medicine, September 2011.
8. Wadman MC, Muelleman RL, Hall D, et al. Qualification discrepancies between urban and rural emergency department physicians. J Emerg Med. 2005;28(3):273–276. [PubMed]
9. Helland LC, Westfall JM, Carmargo CA, Jr, et al. Motivations and barriers for recruitment of new emergency medicine residency graduates to rural emergency departments. Ann Emerg Med.2010;56(6):668–673. [PubMed]
10. McGirr J, Williams JM, Prescott JE. Physicians staffing rural West Virginia emergency departments: residency training and board certification status. Acad Emerg Med. 1998;5:333–336.[PubMed]
11. Sklar D, Spencer D, Alcock J, et al. Demographic analysis and needs assessment of rural emergency departments in New Mexico (DANARED-NM) Ann Emerg Med. 2002;39:456–457.[PubMed]
12. Williamson HA, Rosenblatt RA, Hart LG. Physicians staffing of small rural hospital emergency departments: rapid change and escalating cost. J Rural Health. 1992 Summer;8(3):171–177.[PubMed]
13. McNamara RM, Kelly JJ. Cost of care in the emergency department: impact of an emergency medicine residency program. Ann Emerg Med. 1992;21(8):956–962. [PubMed]
14. Branney SW, Pons PT, Markovchick VJ, et al. Malpractice occurrence in emergency medicine: does residency training make a difference? J Emerg Med. 2000;19(2):99–105. [PubMed]
15. Wadman MC, Muelleman RL, Hall D, et al. Qualification discrepancies between urban and rural emergency deparment physicians. J Emerg Med. 2005;28(3):273–276. [PubMed]
16. Wadman MC, Hoffman LH, Erickson T, et al. The impact of a rural emergency medicine department rotation on applicant ranking of a US emergency medicine residency program. Rural Remote Health. 2007;7(4):686. [PubMed]
17. Stratton TD, Geller JM, Ludtke RL, et al. Effects of an expanded medical curriculum on the number of graduates practicing in a rural state. J Acad Med. 1991;66(2):101–105. [PubMed]