| Author | Affiliation |
|---|---|
| Ali Pourmand, MD, MPH | George Washington University, Department of Emergency Medicine, Washington, DC |
| Raymond Lucas, MD | George Washington University, Department of Emergency Medicine, Washington, DC |
| Jesse M. Pines, MD, MBA | George Washington University, Department of Emergency Medicine, Washington, DC George Washington University, Department of Health Policy, Washington, DC |
| Hamid Shokoohi, MD, MPH | George Washington University, Department of Emergency Medicine, Washington, DC |
| Kabir Yadav, MDCM, MS | George Washington University, Department of Emergency Medicine, Washington, DC |
ABSTRACT
Introduction:
We tested the effect of a brief disposition process intervention on residents’ time to disposition and emergency department (ED) length of stay (LOS) in high acuity ED patients.
Methods:
This was a quasi-experimental study design in a single teaching hospital where ED residents are responsible for administrative bed requests for patients. Enrollment was performed for intervention and control groups on an even-odd day schedule. Inclusion criteria were ED patients triaged as Emergency Severity Index (ESI) 1 and 2. In the intervention group, the attending physician prompted the resident to make the disposition immediately after the evaluation of resuscitation patients. In the control group, the attending physicians did not intervene in the disposition process unless more than 2 hours passed without a disposition. Main outcomes were time to disposition and total ED LOS.
Results:
A total of 104 patients were enrolled; 53 (51%) in the intervention group and 51 (49%) in the control group. After controlling for ESI and resident training year, mean disposition time was significantly shorter in the intervention group by 41.4 minutes (95% CI: 32.6–50.1). LOS was also shorter in the intervention group by 93.3 minutes (95% CI: 41.9–144.6).
Conclusion:
Prompting residents to enter administrative disposition orders in high acuity patients is associated with significant reduction in both time to disposition and ED LOS.
INTRODUCTION
Background
Prolonged length of stay in critically ill patients in the emergency department (ED) is associated with higher complication rates and higher mortality rates.1,2 This is because often the focus of emergency care is on the initial management of patients (such as immediate resuscitation). Longer term management, such as managing ventilator settings and titrating medications, is sometimes deprioritized because of competing demands and expectation that those tasks will occur in the inpatient setting. Therefore, reducing length of stay (LOS) for this high-risk patient group is important because it may not only reduce overall ED crowding but also improve patient outcomes.3A recent American College of Emergency Physicians policy statement on the boarding of intensive care unit patients stated that hospitals have the responsibility to ensure, “…the prompt transfer of patients admitted to inpatient units as soon as the treating emergency physician makes such a decision.”4
Importance
For emergency medicine training programs, teaching ways to reduce LOS to ED residents is consistent with the Accreditation Council for Graduate Medical Education (ACGME) core competency requirement for training in systems-based practice. One of the key steps in ED care is the placement of an administrative bed request, which prompts hospital staff to search for available inpatient beds. The timing of the placement of the bed request should ideally come when the decision is made to admit; however, there is provider variation in when the bed requests are entered. Some providers place bed requests early, while others wait for extensive clinical data to justify the admission to the admitting physician or consultant. There is a paucity of research on variation in disposition practices in the ED and how teaching residents to focus early on the disposition might influence actual time to disposition or overall ED LOS.
Goals of this investigation
We tested the impact of a real-time disposition process intervention to prompt ED residents to focus early on the administrative bed request on time to disposition and overall ED LOS. We hypothesized that actively prompting the disposition would be associated with shorter ED LOS.
METHODS
Study Design and Setting
This was a quasi-experimental study design, approved by the institutional review board (IRB) to assess the impact of a brief process intervention on time to administrative bed request and overall ED LOS in high acuity ED patients. The study population was residents in a 4-year ED residency program caring for high-acuity patients – emergency severity index (ESI) 1 or 2 – at an urban community hospital affiliated with their program. Patients were enrolled from August 2009 to March 2010. Eight attending physicians enrolled patients in this study and patients were only enrolled when those attendings were working clinically in the ED. Attending physicians enrolled both intervention and control patients.
Enrollment, Interventions, and Data Processing
Patients were assigned to either the intervention or control arms of the study on alternating odd-even days. This was done because of ED residents overlapped with multiple attendings per day and we did not want to enroll the same resident in the intervention and control arms on the same day. The ED residents and the patients were blinded to the study. In the intervention group, when the ED resident presented the case to the attending physician, the attending delivered bedside teaching in the usual fashion but also deliberately prompted the residents about patient disposition. The attending physicians were trained through a 45-minute lecture reviewing the literature on ED LOS, crowding and the impact on residency training. In the control group, after case presentation, the ED resident was not prompted about disposition status until the resident had not submitted admitting papers for more than 120 minutes. At such time, the attending physician would submit admitting papers for the patient without informing the EM resident to avoid any study-related delays of time to disposition. The resident was still expected to submit the admitting papers.
Data were collected on the resident’s post-graduate year (PGY) level, the patient’s ESI level, the disposition time, and total length of stay for each encounter. We defined disposition time as the time interval between patient arrival (the earliest administrative time-stamp in the patient’s record) and the resident submission of admission papers (which was also time-stamped). ED LOS was defined as time between patient arrival and the time that patient physically left the ED. The data were collected from admission tickets and then entered in a spreadsheet.
Data Analysis
We used appropriate descriptive statistical methods and group comparison tests to compare the outcomes of interest (disposition time, LOS) and the covariates (ESI, PGY level). Controlling for covariates, we constructed separate multivariate linear regression models for both outcomes of interest. Regression diagnostics were performed to confirm good model specification with normal distribution of residuals and without implausible overly influential outlier observations. No formal power calculation was conducted for this study. We performed statistical analysis using Stata version 11.1 (StataCorp, College Station, Texas).
RESULTS
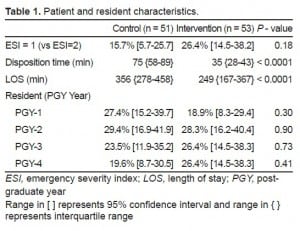
There were 104 encounters available for analysis, 53 (51%) in the intervention group and 51 (49%) in the control group. As disposition time and LOS was not normally distributed, we performed non-parametric tests for group comparisons. Patient and resident characteristics were not significantly different between the two groups (Table 1).
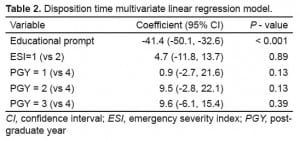
Median disposition time was significantly different between the intervention and control groups (P < 0.001), 35 minutes (interquartile range [IQR]: 28–43) and 75 minutes (IQR: 58–89) respectively (Table 1). In multivariate linear regression modeling controlling for residents’ level of training and patient ESI level, only the disposition process intervention was significantly associated with patient’s disposition time, accounting for a 41.4 minutes reduction (95% CI: 32.6–50.1) (Table 2). Regression diagnostics confirmed good model specification with normal distribution of residuals and without implausible overly influential outlier observations.
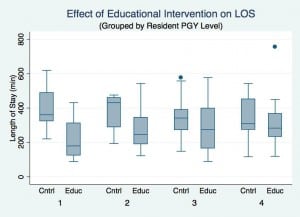
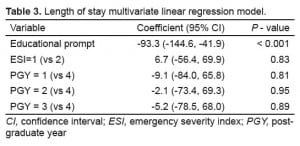
Median LOS was also significantly different between the intervention and control groups (P < 0.001), 249 minutes (IQR: 167–367) and 356 minutes (IQR: 278–458) respectively (Table 1). Although intervention effect on LOS also appeared to vary by residents’ level of training (Figure 1), in multivariate linear regression modeling controlling for residents’ level of training and patient ESI level, the process intervention was significantly associated with patient LOS, accounting for a 93.3 minute reduction (95% CI: 41.9–144.6) (Table 3). Regression diagnostics confirmed good model specification.
LIMITATIONS
There are limitations to our study. First, this was a small study of 104 cases, based in one urban academic hospital center and there were only a handful of attending physicians who enrolled patients. It is unclear whether this improvement could be extrapolated into other clinical settings with other physicians. In addition, all attending physicians were instructed on a standardized delivery of the intervention; however, it is unknown whether it was delivered in a uniform manner.
In our study we did not randomize patients; instead, we used an odd-even day enrollment scheme. It is possible that this could have created some selection bias; however, we think that this would likely be non-differential. In addition to administrative bed request times, ED LOS can be influenced by several factors, including the concurrent hospital occupancy that were not controlled for in our study.
Finally, our evaluation only included patients with ESI 1–2 complaints who would clearly be admitted to an inpatient setting based on the acuity of their illness. The study did not include other patients whose disposition may have depended on the results of lab tests, imaging studies, or consultant evaluations. Further work with a brief disposition process intervention spanning all patient acuity levels would be appropriate.
DISCUSSION
Many important tasks are required for ED physicians to deliver optimal patient care.5 Timely consultation and disposition is one of them and involves navigating the complexities of the inpatient and outpatient system. We found that a disposition process intervention where attending physicians prompt early bed request decision-making by residents was effective in reducing not only time to disposition but also overall ED LOS. Because prolonged ED LOS in critically-ill patients is associated with poorer outcomes, this simple intervention to hasten the admission process may improve quality of care.
The ED literature highlights the importance of timely consultation and disposition yet provides few practical bedside examples about how to teach trainees how to optimize patient flow.6–9 One study incorporated teaching timely disposition and consultation as one of several systems-based practice criteria in an ED simulation curriculum.6 Educators in other specialties have described approaches, including dedicated systems-based practice conferences, web-based or electronic learning modules, and required resident scholarly projects around systems-based practice.10–17 Our study demonstrated that a deliberate inclusion of early disposition into bedside teaching was not only a feasible approach that influenced resident behavior, but also positively impacted a clinically relevant outcome measure: ED LOS for high-acuity patients.
Adding additional tasks in bedside teaching may not be attractive to some educators in an already crowded ED environment. Faculty-resident interaction time already may occupy as little as 20% of available time in the ED and resident surveys suggest crowding negatively affects training.18,19Nevertheless, other studies suggest that effective teaching can still occur in crowded EDs. One study found no relationship between the workload of attending physicians and their student teaching evaluations.20 Other studies have found that attending workload and overall crowding have no influence on resident perception of their teaching and that individual attending teaching skills and attributes were more important.21,22
CONCLUSION
A brief process intervention to prompt residents to enter bed requests earlier was associated with shorter time to disposition and shorter LOS in high-acuity patients. Additional studies are needed to validate this approach for lower-acuity patients and in other ED settings.
Footnotes
Supervising Section Editor: Erik D. Barton, MD, MS, MBA
Submission history: Submitted March 28, 2012; Revision received July 29, 2012; Accepted October 19, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.10.12243
Address for Correspondence: Ali Pourmand, MD, MPH, Department of Emergency Medicine, The George Washington University 2150 Pennsylvania Ave. NW, Suite 2B Washington, DC 20037. Email: apourmand@mfa.gwu.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. [PubMed]
2. Carr B, Kaye A, Wiebe D, et al. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma. 2007 Jul;63(1):9–12. [PubMed]
3. Hoot N, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerge Med. 2008;52:126–136. [PubMed]
4. Boarding of Admitted and Intensive Care Patients in the Emergency Department. Ann Emerg Med.2011;58:110. [PubMed]
5. Model of the Clinical Practice of Emergency Medicine 2009. Retrieved June 15, 2011. Available at:http://www.acep.org/WorkArea/DownloadAsset.aspx?id=47823.
6. Reisdorff E, Hayes O, Walker G, et al. Evaluating systems-based practice in emergency medicine.Acad Emerg Med. 2002;9:1350–1354. [PubMed]
7. Dyne P, Strauss R, Rinnert S. Systems Based Practice: The Sixth Core Competency,” Academic Emergency Medicine. 2002;9:1270–1277. [PubMed]
8. Hobgood C, Promes S, Wang E, et al. Outcome assessment in emergency medicine-a beginning: results of the council of emergency medicine residency directors emergency medicine consensus workgroup on outcome assessment. Acad Emerg Med. 2008;15:267–277. [PubMed]
9. Wang EE, Vozenilek JA. Addressing the Systems-based Practice Core Competency: A Simulation-based Curriculum. Academic Emergency Medicine. 2005;12(12):1191–1194. [PubMed]
10. Sultana CJ, Baxter JK. Improving patient safety and quality of care is part of systems-based practice and practice-based learning. Obstet Gynecol. 2011 Feb;117(2 Pt 1):377–382. [PubMed]
11. Nagler A, Andolsek K, Dossary K, et al. Addressing the systems-based practice requirement with health policy content and educational technology. Med Teach. 2010;32(12):e559–565. [PubMed]
12. Eskildsen MA. Review of Web-Based Module to Train and Assess Competency in Systems-Based Practice. J Am Geriatr Soc. 2010 Dec;58(12):2412–2413. [PubMed]
13. Kerfoot BP. Learning benefits of on-line spaced education persist for 2 years. J Urol. 2009 Jun;181(6):2671–2673. [PubMed]
14. Buchman RF, Deloney LA, Donepudi SK, et al. Development and implementation of a systems based practice project requirement for radiology residents. Acad Radiol. 2008 Aug;15(8):1040–1045. [PubMed]
15. Delphin E, Davidson M. Teaching and evaluating group competency in systems-based practice in anesthesiology. Anesth Analg. 2008 Jun;106(6):1837–40183. [PubMed]
16. Zerzan AE, Choo J, Shenson D, et al. Teaching systems-based practice to residents by using independent study projects. Acad Med. 2005 Feb;80(2):125–128. [PubMed]
17. Doezema D, McLaughlin S, Sklar DP. An approach to fulfilling the systems-based practice competency requirement. Acad Emerg Med. 2002 Nov;9(11):1355–1359. [PubMed]
18. Chisholm CD, Whenmouth LF, Daly EA, et al. An evaluation of emergency medicine resident interaction time with faculty in different teaching venues. Acad Emerg Med. 2004 Feb;11(2):149–155. [PubMed]
19. Sabbah S. The impact of hospital overcrowding on postgraduate education: an emergency medicine resident’s perspective through the lens of CanMEDS. CJEM. 2009;11(3):247–249.[PubMed]
20. Berger TJ, Ander DS, Terrell ML, et al. The impact of the demand for clinical productivity on student teaching in academic emergency departments. Acad Emerg Med. 2004 Dec;11(12):1364–1367. [PubMed]
21. Kelly SP, Shapiro N, Woodruff M, et al. The effects of clinical workload on teaching in the emergency department. Acad Emerg Med. 2007 Jun;14(6):526–531. [PubMed]
22. Pines J, Prabhu A, McCusker CM, et al. The effect of ED crowding on education. Am J Emerg Med.2010 Feb;28(2):217–220. [PubMed]