| Author | Affiliation |
|---|---|
| Taher Vohra, MD | Henry Ford Hospital, Department of Emergency Medicine, Detroit, Michigan |
| James Paxton, MD, MBA | Henry Ford Hospital, Department of Emergency Medicine, Detroit, Michigan |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: Arterial blood gas and serum lactate (ABG / SL) values have been shown to be markers for occult shock and poor outcome following blunt trauma. However, the utility of ABG / SL in blunt trauma patients who also receive computed tomographies (CT) of the chest, abdomen, and pelvis (CT C&A) remains unknown.
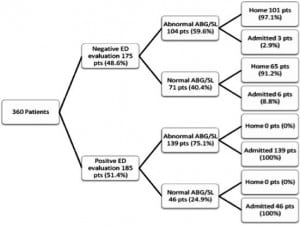
Methods: A chart review was performed of all adult blunt trauma patients who received both CT C&A and ABG / SL upon presentation to our emergency department (ED) between January 1, 2007 and December 31, 2007. These patients (n=360) were identified from our institutional trauma registry database. Patients were divided into subgroups based upon whether they had a positive or negative ED evaluation for traumatic injury requiring hospitalization or immediate operative management. The expected course for patients with negative ED evaluations regardless of ABG / SL was discharge home. The primary outcome measure was the proportion of patients with a negative ED evaluation and an abnormal ABG or SL that were admitted to the hospital.
Results: 2.9% of patients with a negative ED evaluation and abnormal ABG or SL were admitted. Of these, none were found to have any post-traumatic sequalae.
Conclusion: We found that abnormal ABG / SL results do not change management or discharge disposition in patients without clinical or radiographic evidence of traumatic injury on CT C&A. Among patients who receive CT C&A, the routine measurement of arterial blood gas and lactate may be an unnecessary source of additional cost, patient discomfort, and delay in care.
INTRODUCTION
Arterial blood gas (ABG) and serum lactate (SL) abnormalities have both been identified as markers for occult malperfusion and poor outcome following blunt traumatic injury.1–5 This has led some authors to advocate the use of arterial blood gas with serum lactate (ABG / SL) as a screening tool for occult injury in all patients sustaining blunt trauma.4 Our institutional protocol requires that ABG / SL be obtained on all Level I or Level II blunt trauma patients presenting to the resuscitation bay. However, cross-sectional computed tomography (CT) of the chest, abdomen and pelvis (CT C&A) is also obtained on many of these patients. It remains unclear whether or not ABG / SL adds any predictive or prognostic value in the detection of clinically-significant occult injury when early CT C&A is also obtained.
Routine laboratory testing in blunt trauma patients has been dramatically reduced over the past decade.6 Studies have shown that the routine use of chemistry panels, amylase, and coagulation studies are of limited clinical value in the evaluation of blunt trauma patients, and merely add to overall hospital resource use.6 Among those blunt trauma patients who also receive CT C&A imaging, routine ABG / SL testing may also be an unnecessary source of additional cost, patient discomfort, and delay in care. This study sought to determine whether abnormal ABG / SL values change the emergency department (ED) disposition of patients who also receive an early CT of the chest, abdomen and pelvis.
METHODS
All Level I or Level II adult blunt trauma patients presenting to the ED resuscitation bay between January 1, 2007, and December 31, 2007, were identified from the institutional trauma registry. We considered patients ≥ 16 years of age adults for the purposes of this study. Exclusion criteria included the absence of an ABG or serum lactate level, the absence of complete CT C&A imaging while in the ED, concomitant penetrating trauma, transfer to or from another institution prior to hospital admission, or patients who left prior to completion of service.
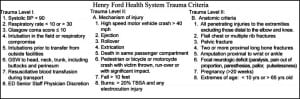
The criteria for Level I and Level II trauma triage at our institution are shown in Figure 1. There is some discretion with regards to Level II triage criteria and some of these patients, as well as Level 3 trauma patients, are not seen in the resuscitation bay. Patients who are not seen in the resuscitation bay do not receive the same routine laboratory studies and therefore were not included in this study.
We developed a data abstraction tool to collect information, and instructed a research assistant on using the tool. All data were collected by the study authors and a single research assistant. This tool collected demographic data (age and gender), initial ABG and lactate values, results of all CT studies, mechanism and types of traumatic injuries, ED complications, and final disposition from the ED for all patients. Patients who were admitted to the clinical decision unit (CDU) for observation ≤ 23 hrs were considered to be hospital admissions for the purposes of this study, as they were not discharged home.
An abnormal ABG was defined as a pH of less than 7.35 or greater than 7.45, or a base deficit (BD) of ≤ –6. An abnormal lactate was defined as a serum lactate level > 1.8 mmol/L, which is the upper limit of normal at our institution.
We analyzed 2 patient subgroups. The first subgroup consisted of those patients with a negative ED evaluation for traumatic injury. By definition, these patients all had a CT C&A demonstrating no acute traumatic injuries, normal CT Head or Glasgow Coma Scale (GCS) of 15 and no clinical concern for head injury, and no radiographic or clinical evidence for any major traumatic injury requiring emergent operative intervention or hospital admission. In short, these patients had no traumatic sequelae identified that would have required hospital admission or emergent operative intervention.
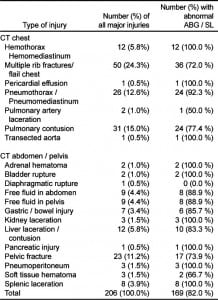
The second subgroup consisted of those patients with a positive ED evaluation for traumatic injury. Patients in this group had either a CT C&A demonstrating significant acute traumatic injuries, or some other radiographic or clinical evidence of blunt traumatic injury requiring immediate operative intervention or hospital admission. In short, these patients would have required admission to the hospital for traumatic injuries regardless of ABG / SL results. For the purposes of this study, major injury was defined as blunt traumatic injury requiring immediate operative intervention or hospital admission.
The expected course for patients with a negative ED evaluation in the absence of the information provided by an ABG or serum lactate level would be discharge to home. Patient charts were reviewed looking for evidence of a change in expected management in both of these groups. The primary outcome measure was the proportion of patients with a negative ED evaluation and an abnormal arterial blood gas and/or lactate that were subsequently admitted to the hospital.
Secondary outcomes included the proportion of overall abnormal ABG / serum lactate results, and the proportion of patients with an abnormal ABG or serum lactate and a negative ED evaluation that subsequently sustained an ED complication. ED complications were defined as ED mortality, ED cardiac or respiratory arrest with successful resuscitation, or significant hypotension requiring the transfusion of blood products after the patient’s initial resuscitation was completed.
RESULTS
We identified 464 adult blunt trauma patients from our institutional trauma registry who presented to the ED resuscitation bay between January 1, 2007, and December 31, 2007, . We excluded 104 patients from the study due to absence of CT C&A imaging (63 patients), transfer from or to another institution (28 patients), absence of either ABG or serum lactate value (6 patients), inaccurate patient identifier information (6 patients), or patient leaving prior to completion of service (1 patient).
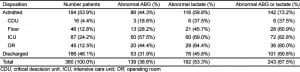
Three hundred sixty adult blunt trauma resuscitation patients met inclusion criteria. We found significant differences in mean pH (p<0.001), mean partial pressure of carbon dioxide (p=0.04), mean serum lactate level (p<0.001), and mean base deficit (p<0.001) between groups. We found no significant differences between groups in regards to mean partial pressure of oxygen (p=0.28) or mean oxygen saturation (p=0.88). Patients with a negative ED evaluation were generally younger than patients with a positive ED evaluation (mean age 38.8 years vs. 42.5 years, p<0.001). This data is presented in Table 1.
![Table 1. Patient characteristics (positive vs. negative emergency department [ED] evaluation) Table 1. Patient characteristics (positive vs. negative emergency department [ED] evaluation)](https://westjem.com/wp-content/uploads/2013/06/i1936-900X-14-3-212-t01-300x202.jpg)
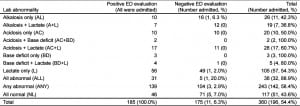

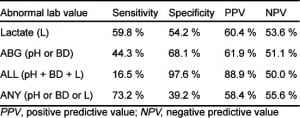
The sensitivity of an abnormal ABG or lactate level for blunt traumatic injury identified on CT of the chest, abdomen, and pelvis was 69.2%, with specificity of 43.5%. The positive predictive value (PPV) was 34.1%, with negative predictive value (NPV) of 76.9%. In identifying major blunt trauma injury, abnormal ABG (base deficit or pH < 7.35 or > 7.45) alone was found to have a sensitivity of 40.2%, and specificity of 79.8% (PPV 45.7%, NPV 75.9%). Abnormal serum lactate alone was associated with a sensitivity of 62.6%, and specificity of 50.6% (PPV 34.9%, NPV 76.2%) for major injury identified on CT.
The sensitivity of an abnormal ABG or lactate level for blunt traumatic injury requiring hospital admission was 73.2%, with specificity of 39.2%. The PPV was 58.4%, NPV of 55.6%. In predicting hospital admission, abnormal ABG (abnormal base deficit or pH) alone was found to have a sensitivity of 44.3%, and specificity of 68.1% (PPV 61.9%, NPV 51.1%). Abnormal serum lactate alone was associated with a sensitivity of 59.8%, and specificity of 54.2% (PPV 60.4%, NPV 53.6%). These results are presented in Table 6, including descriptive statistics for various combinations of abnormal lab values.
We found only 3 cases among the 360 patients included in our analysis that appeared to have a change in disposition from the ED due to abnormal ABG / SL values. The first of these patients was a 51-year-old male involved in a motor vehicle collision (MVC) who was admitted to the inpatient medical floor for known Atrial Fibrillation with Rapid Ventricular Response with an arterial pH 7.52 but otherwise normal ABG / SL. The second patient was a 33-year-old female involved in an MVC who was admitted for observation in the Clinical Decision Unit (CDU) for persistent abdominal pain with a lactate 2.4 mmol/L and discharged the following morning. The third patient was a 16-year-old male involved in an assault who was admitted to the CDU for an unexplained elevated lactate level (12.5 mmol/L) and base deficit of 9. He was also discharged home the following morning. All 3 patients had negative laboratory and radiographic evaluations in the ED with the exception of the ABG / SL. None of these 3 patients were found to have any post-traumatic sequelae during the time that they were monitored in the hospital.
Of the 175 patients with negative ED evaluations, 6 were admitted to the hospital despite normal ABG / SL values. One of these patients was admitted to the intensive care unit for a new diagnosis of atrial fibrillation, and 5 were admitted to the CDU for observation. Three of the 5 CDU patients were admitted for pain control, one was admitted for an elevated amylase level that normalized the following day, and 1 patient was observed for < 23 hours following infiltration of CT intravenous contrast. There were no ED complications identified in patients with a negative ED evaluation.
DISCUSSION
Arterial blood gases and serum lactate levels have been shown to be appropriate laboratory studies in the evaluation of select blunt trauma patients, especially those patients who have sustained significant traumatic injury. The utility of serial blood gases and lactate levels in assessing the adequacy of fluid resuscitation in blunt trauma patients has been well studied and is strongly supported by the current trauma and critical care literature.7–8 Table 4 also demonstrates that patients in this study with major injury identified on CT generally have statistically-higher mean lactate levels and mean base deficits than patients in this study without major injury. However, in this study, the mean base deficit for patients with major injury identified on CT was still within normal limits for healthy individuals, and the mean serum lactate for uninjured patients was elevated above normal limits at our institution. This data suggests that ABG / SL levels are of limited value in detecting clinically-significant occult injury among patients with a normal CT evaluation of the chest, abdomen, and pelvis following blunt trauma.
CT has been shown to reliably identify major traumatic injury following blunt trauma.9–10 ABG / SL levels can also play an important role in defining fluid resuscitation endpoints and evaluating the degree of post-traumatic malperfusion when followed over time. However, our data suggests that abnormal ABG / SL results do not alter discharge disposition or identify ED complications in those blunt trauma patients who also receive extensive CT early in their resuscitation. In this patient population, a thorough physical examination, appropriate CT, and other radiographic studies were adequate to identify injuries ultimately requiring immediate management or hospital admission. Based on these results, routine ABG / SL measurements should not be used as screening tests to identify occult injury in adult blunt trauma patients who undergo CT C&A.
Routine ABG / SL testing may not add any diagnostic value to a patient’s ED evaluation, but is associated with additional costs to the patient, potential complications, and the misappropriation of already limited ED resources. The laboratory cost of an ABG / SL level at our institution is $216, which represents a cumulative cost of $77,760 for all 360 patients included in this analysis. Besides this additional cost, cannulation of the radial artery for sampling also carries the risk of certain complications, including bleeding, median nerve injury, pseudoaneurysm formation, and radial artery thrombosis.11
Based upon these results, we hope to defer ABG / SL testing on all patients who will be receiving early CT C&A at our institution until CT results are known, unless the patient is deemed clinically unstable or is expected to require hospital admission independent of CT findings. We believe that these changes to our institutional blunt trauma protocol will save our patients this unnecessary expense, while improving their risk profile without compromising the quality of the care provided in the ED.
LIMITATIONS
We faced the standard limitations of a retrospective study. However, these were mitigated by the fact that the trauma registry data is collected prospectively and the data points are readily found in the registry. The main limitation in this analysis was the inability to eliminate practice variation due to the retrospective nature of the study. The institutional trauma protocol requires that ABG / SL levels be obtained on all blunt trauma patients presenting to the resuscitation room. In reality, there was some variability in the frequency of ABG and lactate collection and this may have affected the results. We also did not evaluate how ABG / SL results may have affected intravenous fluid administration or other treatments provided in the ED. Lastly, the lack of complete follow up of discharged patients is a limitation of their true final outcome.
CONCLUSION
Abnormal arterial blood gas or serum lactate levels do not change the ED disposition of adult blunt trauma patients who also receive an early CT of the chest, abdomen and pelvis. The routine use of ABG / SL on these patients is not warranted.
Footnotes
Supervising Section Editor: Ali S. Raja, MD
Submission history: Submitted October 4, 2011; Revision received Feburary 9, 2012; Accepted March 26, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.6905
REFERENCES
1. Davis JW, Kaups KL. Base deficit in the elderly: a marker of severe injury and death. J Trauma.1998;45(5):873–877. [PubMed]
2. Davis JW, Parks SN, Kaups KL. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996;41(5):769–774. et al. [PubMed]
3. Rutherford EJ, Morris JA, Jr, Reed GW. Base deficit stratifies mortality and determines therapy. J Trauma. 1992;33(3):417–423. et al. [PubMed]
4. Barquist E, Pizzutiello M, Burke M. Arterial blood gas analysis in the initial evaluation of the nonintubated adult blunt trauma patient. J Trauma. 2002;52(3):601–602. et al. [PubMed]
5. Manikis P, Jankowski S, Zhang H. Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am J Emerg Med. 1995;13(6):619–622. et al. [PubMed]
6. Namias N, McKenney MG, Martin LC. Utility of admission chemistry and coagulation profiles in trauma patients: a reappraisal of traditional practice. J Trauma. 1996;41(1):21–25. [PubMed]
7. Callaway DW, Shapiro NI, Donnino MW. Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma. 2009;66(4):1040–1044. et al. [PubMed]
8. Schulman AM, Claridge JA, Carr G. Predictors of patients who will develop prolonged occult hypoperfusion following blunt trauma. J Trauma. 2004;57(4):795–800. et al. [PubMed]
9. Freshman SP, Wisner DH, Battistella FD. Secondary survey following blunt trauma: a new role for abdominal CT scan. J Trauma. 1993;34(3):337–340. et al. [PubMed]
10. Livingston DH, Lavery RF, Passannante MR. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma. 1998;44(2):273–280. et al. [PubMed]
11. Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care.2002;6(3):199–204. [PMC free article] [PubMed]


