| Author | Affiliation |
|---|---|
| Karl A. Sporer, MD | University of California, San Francisco, Department of Emergency Medicine, San Francisco General Hospital |
| Nicholas J. Johnson, BS | University of California, San Francisco, School of Medicine |
ABSTRACT
Introduction:
Medical Priority Dispatch System (MPDS) is a type of Emergency Medical Dispatch (EMD) system used to prioritize 9-1-1 calls and optimize resource allocation. Dispatchers use a series of scripted questions to assign determinants to calls based on chief complaint and acuity. We analyzed the prehospital interventions performed on patients with MPDS determinants for breathing problems, chest pain, unknown problem (man down), seizures, fainting (unconscious) and falls for transport status and interventions.
Methods:
We matched all prehospital patients in complaint-based categories for breathing problems, chest pain, unknown problem (man down), seizures, fainting (unconscious) and falls from January 1, 2004, to December 31, 2006, with their prehospital record. Calls were queried for the following prehospital interventions: Basic Life Support care only, intravenous line placement only, medication given, procedures or non-transport. We defined Advanced Life Support (ALS) interventions as the administration of a medication or a procedure.
Results:
Of the 77,394 MPDS calls during this period, 31,318 (40%) patients met inclusion criteria. Breathing problems made up 12.2%, chest pain 6%, unknown problem 1.4%, seizures 3%, falls 9% and unconscious/fainting 9% of the total number of MPDS calls. Patients with breathing problem had a low rate of procedures (0.7%) and cardiac arrest medications (1.6%) with 38% receiving some medication. Chest pain patients had a similar distribution; procedures (0.5%), cardiac arrest medication (1.5%) and any medication (64%). Unknown problem: procedures (1%), cardiac arrest medication (1.3%), any medication (18%). Patients with Seizures had a low rate of procedures (1.1%) and cardiac arrest medications (0.6%) with 20% receiving some medication. Fall patients had a lower rate of severe illness with more medication, mostly morphine: procedures (0.2%), cardiac arrest medication (0.2%), all medications (28%). Unconscious/fainting patients received the following interventions: procedures (0.3%), cardiac arrest medication (1.9%), all medications (32%). Few stepwise increases in the rate of procedures or medications were seen as determinants increased in acuity.
Conclusion:
Among these common MPDS complaint-based categories, the rates of advanced procedures and cardiac arrest medications were low. ALS medications were common in all categories and most determinants. Multiple determinants were rarely used and did not show higher rates of interventions with increasing acuity. Many MPDS determinants are of modest use to predict ALS intervention.
INTRODUCTION
Emergency Medical Dispatch (EMD) is a system of categorizing and prioritizing emergency calls in order to send an appropriate ambulance response. A variety of studies in differing systems with both health and non-health trained dispatchers have been published using a variety of different clinical measures to gauge success.1–12 The Medical Priority Dispatch System (MPDS) is a complex computer-based EMD system that uses callers’ responses to scripted questions to categorize cases into numerical complaint-based categories, which are further assigned a priority (Alpha, Bravo, Charlie, Delta, or Echo) based on their perceived acuity. Alpha and Bravo represent the lowest acuity calls, with Charlie, Delta and Echo representing higher acuity calls that may require advanced assessment and/or intervention. Calls may be further assigned a numerical subgroup and a modifier, which provide responders with more specific details about the call. Together, the complaint-based numerical category, priority (Alpha through Echo), subgroup and modifier (when present) make up the MPDS determinant. For instance, a call may be assigned to the MPDS determinant 6D2A. The number six is the complaint-based category for breathing problems, “D” (or Delta) represents priority. Two is a subcategory that informs providers that the patient is not alert, and “A” is a modifier that indicates the patient has a history of asthma.
Several studies have examined the predictive accuracy of MPDS and other EMD systems for a variety of outcomes, including paramedic-assigned acuity score, physician diagnosis of an acute illness, cardiac arrest, “Code 3” or “lights and sirens” return, and the need for Advanced Life Support (ALS) intervention.9, 10, 13–18 Most research has demonstrated that MPDS and other EMD systems identify most but not all urgent calls with a considerable degree of overtriage.7–10, 12, 14, 16, 19–21
Patients with breathing problems make up approximately 11–15% of all Emergency Medical Services (EMS) calls.9, 15 Because there are no low priority determinants related to respiratory distress, it has a sensitivity of 100% to predict ALS intervention, and the positive predictive value has ranged from 44–84%.9, 11 Previous studies have demonstrated little difference in medication administration rates (range of 40 to 65%) and airway procedure rate (1%) between the various subgroups of patients with breathing problems.11, 12 A recent study demonstrated increasing rates of cardiac arrest (0.1% to 17%) with increasing category severity.15
Patients with chest pain make up approximately 10% of EMS calls.9 One study examined the differences between chest pain determinants and demonstrated that they all had relatively high rates of medication administrations (40% to 65%), usually aspirin or nitroglycerin.11 Fewer than 1% of each determinant required advanced airway maneuvers, cardiac arrest medications or defibrillation.12
Because few (1%) of the chest pain calls were classified as Basic Life Support (BLS), the sensitivity of EMD was excellent (99–100%) to predict ALS interventions but with very poor specificity (0–2%).9,11 Another study of the London EMS system also demonstrated infrequent use of the alpha priority among chest pain patients and a consistently low rate of cardiac arrest among all determinant (<1%).16 The Alpha priority had a lower rate of “lights and sirens” return (3%) as compared to Charlie and Delta priorities (both 12%).
Patients with an unknown problem (man down) make up approximately 3% of all EMS calls.9 In a previous study in our system, this category had a sensitivity of 36% with a specificity 85% for ALS interventions.22 One study of 696 patients classified as an unknown problem had an advanced procedure rate of 1% and medications were administered to 22%.15 A more in-depth analysis of the unknown problem complaint-based category revealed that the rate of cardiac arrest among those with a bravo priority were all less than 1% and modestly higher (1.5%) rate of those with Delta (life status questionable).15
Patients with a seizure make up approximately 4% of all EMS calls.9, 15 The MPDS determinants for seizure have been demonstrated to have a reasonable sensitivity (83%) and poor specificity (20%) to predict the need for ALS.11 Another study from Toronto demonstrated that determinants for seizure had 66% sensitivity and a 46% specificity for Canadian Triage and Acuity Scale (CTAS) score.9
It has been described that approximately 3% of cardiac arrest calls are initially categorized as a seizure.9, 14, 23, 24 The 12D1 determinant (seizing not breathing) was infrequently used in one study but had an extraordinarily high rate of cardiac arrest (26%).14 Those patients with a known history of seizure had a clinically insignificant rate of cardiac arrest.
Patients with a history of falls make up 11% of all EMS calls.9 One study examined 103 calls from the falls complaint-based category and demonstrated that 26% of these were found to have important clinical field findings and that these had a modest correlation with age.25 The rates of ALS interventions given to fall patients in the lowest priority (Alpha) determinants ranged from 7–10% in one system and 46% in another.3, 5, 6 The rate of ALS interventions for all Fall patients in another study was 27%.26 That same Toronto study demonstrated that the fall category had a 20% sensitivity and a 93% specificity for CTAS score.9
Patients in the fainting/unconscious category make up 9% of all EMS calls.9 The MPDS determinants for fainting/unconscious have been demonstrated to have good sensitivity (92%) and very poor specificity (2%) to predict the need for ALS.11 The Toronto study demonstrated that the fainting/unconscious category had a 98% sensitivity and a 9% specificity for CTAS score.9
This descriptive analysis of an individual EMS system is the first to provide a comprehensive evaluation of interventions performed in the specific MPDS determinants for these common problems for both transported and non-transported patients. This study asks the following question: do the multiple determinants, subgroups, and modifiers in the breathing problems, chest pain, unknown problem (commonly known as “man down”), seizure, falls and fainting/unconscious categories aid in predicting prehospital interventions?
METHODS
San Mateo County is an urban/suburban county of 552 square miles with a population of 700,000. It receives approximately 40,000 calls for emergency medical assistance annually. All calls receive an ALS response under a tiered system, consisting of a fire department single paramedic first response team and a private ambulance staffed with at least one paramedic. An electronic prehospital care record is established for each patient, which includes patient demographics, medical history, signs and symptoms, and clinical interventions.
Nine-one-one callers are asked a series of scripted questions that include the patient’s level of consciousness, age, chief complaint and other complaint-specific questions. A computer-aided dispatch system records general information regarding each call, including date, time, location of call, dispatch time, dispatch code and disposition. We used MPDS (Versions 11.2 and 11.3 (May 2006), NAEMD, Salt Lake City, UT) to categorize cases into standardized, complaint-based categories, which were further classified as Alpha or Bravo for no “lights and sirens” response, and Charlie, Delta, or Echo for “lights and sirens” response. In some cases, a subgroup or modifier was added to alert providers to further details about the call.
All EMS patients from January 1, 2004, to December 1, 2006, were identified from the Computer Aided Dispatch system and linked automatically by call number to an electronic prehospital care record. We electronically imported data into a Excel spreadsheet (Microsoft Corporation, Redmond, WA). In this study we included all patients assigned a priority by MPDS in the categories of breathing problems, chest pain, unknown problem (commonly known as “man down”), seizure, falls and fainting/unconscious. The investigators chose these complaint-based categories a priori, as they make up a significant portion of EMS calls and encompass a large number of prehospital interventions. Furthermore, several of these categories have had mixed results or inconclusive results about their predictive abilities for prehospital interventions in prior studies. The University of California, San Francisco Committee on Human Research approved this study.
ALS level of care was defined as those patients who received a procedure, a medication or an intravenous (IV) fluid infusion. Medications available in the San Mateo County EMS system included nitroglycerin, aspirin, adenosine, albuterol, atropine, epinephrine, dopamine, diphenhydramine, lidocaine, naloxone, glucagon, midazolam, sodium bicarbonate, dextrose 50%, morphine, activated charcoal, oral glucose, glucose cola and intravenous fluid. Oxygen was not included as a medication. Intravenous fluid was defined either as an infusion of a volume greater than 100cc or as a chart in which the phrases “wide open” or “infusion” were noted. Procedures included endotracheal intubation, Combitube placement, defibrillation, transcutaneous pacing, cardioversion, needle cricothyrotomy or needle thoracotomy. Blood glucose measurement, wound care, splinting, cervical spine immobilization and pulse oximetry were not included as procedures, as these are considered BLS skills in our system. We also excluded IV catheter placement without fluid infusion, as prior studies in our system demonstrated a high rate of intravenous line insertion in low acuity patients.6 Patients who did not receive a medication or a procedure were considered to have received BLS level of care. Patients not transported to the hospital were placed in a non-transport category.
We analyzed calls in the complaint-based categories for breathing problems, chest pain, unknown problem (man down) seizures, fainting (unconscious) and falls for transport status and ALS interventions. They were queried for the following prehospital interventions: BLS care only, intravenous line placement only, medication given, procedures or non-transport. We tabulated the numbers and percentages of each of these interventions tabulated for each determinant. We directly compared percentages of prehospital interventions in each category, and assessed statistical significance via a two-tailed paired t-test using Statistics Calculator (StatPac Inc., Bloomington, MN).
RESULTS
A total of 77,394 calls underwent the EMD process during the study period. The number and percentage of the total patients in each category are as follows: breathing problems 9,435 (12.2%), chest pain 4,679, (6.0%), unknown problem 1,094 (1.4%), seizure 2,606 (3.4%), falls 6,741 (8.7%), and fainting/unconscious 6,763 (8.7 %).
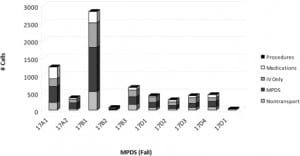
Among those patients with breathing problems, the far majority of the patients were classified as 6D1, severe respiratory distress (Figure 1). There was no significant difference in the rate of advanced procedures between those with 6D1 (1.2%) and 6D1A (with asthma) [0.9% p=0.33]. There was a small but statistically significant difference in the advanced procedure rate of 6C determinants (0%), as compared to 6D (1.1% p<0.01) [Table 1]. Less than 1% of all patients with breathing problems received a procedure. Of the 88 patients with breathing problems who received a procedure, most received an advanced airway.
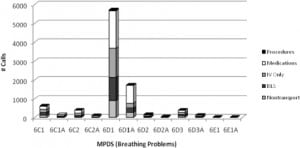
Albuterol and nitroglycerin were the most common medications among those patients with a breathing problem with 38% of all these patients receiving some medication. One hundred forty-nine of these patients (1.6%) received cardiac arrest drugs (Table 2).

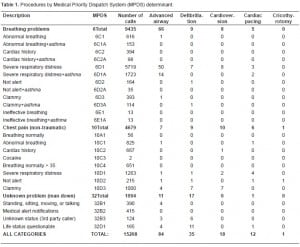
For those patients with chest pain there was a wide distribution of interventions among determinants, except for the rarely used 10A1 determiant (Figure 2). There was a small stepwise increase in the rate of procedures or medications seen in this category, with 53% of calls in the 10C determinant receiving procedures or medications compared with 49% in 10D. (p=0.02) [Tables 1and and2].2]. Only 23 (0.5%) of the patients with chest pain received a procedure, with some of these patients receiving multiple procedures (Table 1). The procedures in this category were distributed between advanced airways (7), defibrillation (9), cardioversion, (10) transcutaneous pacing (6) and cricothyrotomy (1). Most of these procedures occurred in the Delta and Echo priorities. Of the 4,679 patients with chest pain, 79% received nitroglycerin and 39% received aspirin (Table 2). Seventy-two (1.5%) patients with chest pain received cardiac arrest drugs.
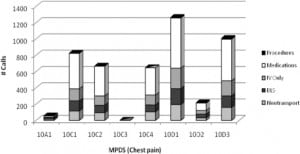
For those patients in the unknown problem (man down) category, there was no increase in medication or procedure rates for higher priority calls (Figure 3). The incidence of procedure and medication use for 32B determinants was 19% compared with 17% in 32D (p=0.56). Among patients with an unknown problem, 1% received a procedure, mostly accounted for by airway and defibrillation (Table 2). Approximately 18% of patients received a medication and 1.3% received cardiac arrest medications in this category (Table 2).
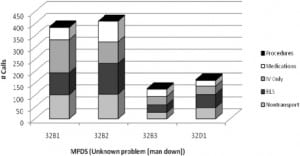
The majority (84%) of the seizure calls fell into three determinants: 12A1, 12D2, or 12D3 (Figure 4). Fifteen (0.6%) patients among the seizure calls received cardiac arrest medications with no discernable pattern among determinants (Table 3). One determinant (12D1, seizure and not breathing) had two out of seven (29%) cases requiring cardiac arrest medications, which was markedly higher than others in this category.

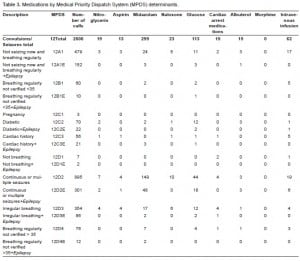

An examination of the rate of procedures among seizure patients produced no discernible pattern (Figure 4 and Table 4). The most commonly administered medications were midazolam and glucose (Table 3). The rate of midazolam administration demonstrated a higher rate among the Delta subcategories (Alpha 4%, Bravo 3%, Charlie 3%, Delta 13%, p<0.02). The subcategory of 12A1 (seizing stopped and breathing regularly) had a 5% rate of midazolam administration. Those patients with continuous or multiple seizures (12D2, 12D2E) had a 17% rate of midazolam administration with a known history of epilepsy making no significant difference.

For those patients with the complaint of falls, there was a wide distribution of interventions among determinants (Figure 5). The rate of advanced airway and cardiac arrest medication among the fall group was very low (0.2%) [Table 3]. Morphine, the most common medication received by fall patients, was administered to 24% of the total. There was no obvious pattern to the rate of morphine administration among the subgroups. The Omega subcategory (17O1 public assist with no injuries or priority symptoms) was rarely used but had no procedures or morphine administration.
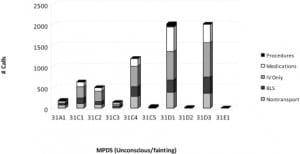
Among those patients in the fainting/unconscious category, there was an increasing rate of medication administration with higher priority (Alpha 15%, Charlie, 25%, Delta 36%, p-value for trend <0.01) [Table 3]. There was no consistent pattern in the types of medications given to these patients (Table 3). The rate of cardiac arrest medication administration increased with higher priority (Alpha 0%, Charlie, 1%, Delta 2.6%, p-value comparing Charlie to Delta <0.01). The rates of advanced airway intervention among the Fainting/Unconscious determinants were all well below 1%, except for the still unconscious (31D1) determinant (3.7%).
DISCUSSION
The MPDSand other EMD systems are designed to aid in the decision to send which prehospital resource and at what level of urgency. The use of multiple determinants and subgroups in each complaint category should aid in these decisions by having demonstrably increasing rates of ALS procedures and medication administration with higher priority.
These six MPDS complaint-based categories collectively accounted for 40% of calls that underwent the EMD process. The procedure rate was low (<1%) in four categories (breathing problem, chest pain, unknown problem and falls) and was only slighter higher in two others (seizure 1.1%, and fainting/unconscious 2.9%).
The rate of administration of cardiac arrest drugs was low (<1%) for most of the categories with the exception of ineffective breathing (31% cardiac arrest), chest pain clammy (3%), man down life status questionable (3%), seizure not breathing (28%) and unconscious with severe respiratory distress (5%). The rate of cardiac arrests among the seizure patients (0.6%) was similar to other studies.17The high rate of cardiac arrest among those seizure patients classified as 12D1 (seizure and not breathing, 29%) was similar to a prior study, although with small numbers in both studies.14
The overall medication rate for each category was seizure 20%, falls 28% and fainting/unconscious 32%. Those patients from the seizure category were most often treated with a benzodiazepine and glucose. Among fall patients, morphine was the most common medication given but accounted for only 24% of the total. Fainting/unconsciousness patients were treated with a broad range of medications.
Prior studies have demonstrated that the addition of ALS resources to a prehospital system causes a modest decrease in mortality among patients with breathing problems or chest pain.27, 28 It is likely that some of these prehospital treatments are time dependent, but it is not known whether a “lights and sirens” response is required to achieve these improvements.
Among those patients with breathing problems, the far majority were classified as severe respiratory distress (6D1), similar to an earlier study.15 We saw little difference in the treatment rates of those with and without asthma. This study demonstrates that most subgroups of breathing problem were rarely used and there is little difference in the rate of medications or procedure rate.10 Due to the relatively high rate of medication administration, all patient who are assigned into breathing problem determinants in a tiered prehospital system should be sent with an ALS response. It is less clear whether lights and sirens are required in all categories.
Among patients with chest pain, very few were placed in the 10A1 determinant. Those infrequent chest pain patients who received a procedure or cardiac arrest medications were found in almost all subgroups. The administration of other medications was common in all determinants (most commonly aspirin and nitroglycerin) making these distinctions to be of questionable use in refining an EMS response. Again, due to the relatively high rate of medication administration, patients who are placed in the chest pain category in a tiered prehospital system should be sent with an ALS response unless BLS providers are capable of administering medications such as aspirin and nitroglycerin.
In our study there are numerous determinants that are rarely used, particularly in the seizure category. The medication rate was less than 5% in the lower acuity seizure determinants and 13% among the Delta priorities. The need for infrequent medication must be balanced against the over triage rate.
Patients in the fall category had a consistently small rate of cardiac arrest and procedures but a high rate of medication use. The types of medications administered are less time dependent (i.e. pain medications) and may allow for a lower priority response for most of these determinants.
Those patients in the fainting/unconscious category had an increasing rate of cardiac arrest medication with higher priority. These were 1% or lower in the Alpha and Charlie priorities and 2.6% in the Delta group. This category worked reasonably well at differentiating those patients who required a rapid EMS response.
Those patients in the unknown problem (man down) determinants had a similar rate of procedures (1%) and cardiac arrest medication administration (1.4%). The medication list for this category was more varied with no discernable pattern. The appropriate response for this category is less clear.
This study used process measures (procedures and medication administration) as proxies for requiring ALS intervention. This determination of the appropriate threshold of ALS dispatch must take into account the local tolerance for the rate of missed ALS calls and the cost and system implications of overtriage. An accepted hierarchy of time dependent interventions and thresholds for under-triage are necessary for the judicious analysis and optimal design of a tiered EMS system.22 This study also is indicative of the inherent difficulty in getting adequate information from 9-1-1 callers that will allow us to make subtle clinical distinctions.
The MPDS has multiple advantages, including its computerization, the consistency of the education and usage, as well as its quality improvement process. Prior studies have demonstrated its ability to improve the diagnosis of cardiac arrest.2 This study demonstrates that the multiple determinants in the categories of breathing problem, chest pain and unknown problem were of modest use in defining need for ALS procedures or medications. The categories of seizure, falls and fainting/unconscious had consistently low rates of cardiac arrest and medical procedures.
LIMITATIONS
This study is limited by the fact that all of its data comes from one community. Another major limitation is the fact that all of our calls receive an ALS response, which may lead to higher delivery of ALS measures. The findings in our single-tiered EMS system may thus differ from those derived in multi-tiered EMS systems. This study was unable to measure protocol compliance with the use of ALS interventions or outcomes and this may not necessarily imply the need for these interventions.
Approximately 12% of EMD and transported calls were unmatched and excluded, potentially introducing a selection bias. This commonly occurred because of a mismatch between the dispatch-generated run number and the number entered by the paramedic. A large percentage of our calls (28%) were not subject to the EMD process and this also may have had an effect on data analysis. Most of these were calls for assistance by law enforcement and fire personnel and have similar rates of interventions. Two versions of the MPDS (Versions 11.2 and 11.3 (adopted May 2006)) were used during this study. Non-transported patients who may have received ALS interventions, such as albuterol or dextrose, would be categorized in the non-transport group.
CONCLUSION
The procedure rate and cardiac arrest rate was low among these common EMD categories. ALS medications were common in all categories and most determinants. Many determinants and subgroups are of questionable use. There are some trends toward more cardiac arrests and procedures among higher priority determinants. Despite these trends, there is still significant over triage and concerning rates of ALS interventions in lower acuity determinants. Other systems might consider a similar analysis as a way of determining the appropriate ambulance response for common complaints.
Footnotes
The authors thank the employees of the San Mateo County EMS Agency and the San Mateo Public Safety Communications Division, for their support in this study.
Supervising Section Editor: Christopher A. Kahn, MD
Submission history: Submitted September 30, 2009; Revision received January 25, 2010; Accepted February 8, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Karl Sporer, MD, Emergency Services, Room 1E21, San Francisco General Hospital, 1001 Potrero Ave., San Francisco, Ca. 94110
Email: Karl.Sporer@emergency.ucsf.edu
FINANCIAL DISCLOSURE
KAS receives compensation for medical direction from American Health and Safety Training, Inc. and the San Francisco Fire Department.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. KAS receives compensation for medical direction from American Health and Safety Training, Inc. and the San Francisco Fire Department.
REFERENCES
1. Bailey ED, O’Connor RE, Ross RW. The use of emergency medical dispatch protocols to reduce the number of inappropriate scene responses made by advanced life support personnel. Prehosp Emerg Care. 2000 Apr–Jun;4(2):186–9. [PubMed]
2. Flynn J, Archer F, Morgans A. Sensitivity and specificity of the Medical Priority Dispatch System in detecting cardiac arrest emergency calls in Melbourne. Prehosp Disaster Med. 2006;21(2):72–6.[PubMed]
3. Shah MN, Bishop P, Lerner EB, et al. Derivation of emergency medical services dispatch codes associated with low-acuity patients. Prehosp Emerg Care. 2003 Oct–Dec;7(4):434–9. [PubMed]
4. Myers JB, Hinchey P, Zalkin J, et al. EMS dispatch triage criteria can accurately identify patients without high-acuity illness or injury. Prehospital Emergency Care. 2005;9:119.
5. Shah MN, Bishop P, Lerner EB, et al. Validation of EMD dispatch codes associated with low-acuity patients. Prehosp Emerg Care. 2005 2005 January March;9(1):24–31. [PubMed]
6. Michael GE, Sporer KA. Validation of low-acuity emergency medical services dispatch codes.Prehosp Emerg Care. 2005 Oct–Dec;9(4):429–33. [PubMed]
7. Palumbo L, Kubincanek J, Emerman C, et al. Performance of a system to determine EMS dispatch priorities. Am J Emerg Med. 1996 Jul;14(4):388–90. [PubMed]
8. Neely KW, Eldurkar J, Drake ME. Can current EMS dispatch protocols identify layperson-reported sentinel conditions? Prehosp Emerg Care. 2000 Jul–Sep;4(3):238–44. [PubMed]
9. Feldman MJ, Verbeek PR, Lyons DG, et al. Comparison of the medical priority dispatch system to an out-of-hospital patient acuity score. Acad Emerg Med. 2006 Sep;13(9):954–60. [PubMed]
10. Craig A, Schwartz B, Feldman M. Development of evidence-based dispatch response plans to optimize ALS paramedic response in an urban EMS system (abstract) Prehospital Emergency Care.2006;10(1):114.
11. Sporer KA, Youngblood GM, Rodriguez RM. The ability of emergency medical dispatch codes of medical complaints to predict ALS prehospital interventions. Prehosp Emerg Care. 2007 Apr–Jun;11(2):192–8. [PubMed]
12. Sporer KA, Johnson NJ, Yeh CC, et al. Can emergency medical dispatch codes predict prehospital interventions for common 9-1-1 call types? Prehosp Emerg Care. 2008 Oct–Dec;12(4):470–8.[PubMed]
13. Ramanujam P, Guluma KZ, Castillo EM, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics-san diego experience. Prehosp Emerg Care. 2008 Jul–Sep;12(3):307–13. [PubMed]
14. Clawson J, Olola C, Heward A, et al. Cardiac arrest predictability in seizure patients based on emergency medical dispatcher identification of previous seizure or epilepsy history. Resuscitation.2007 Nov;75(2):298–304. [PubMed]
15. Clawson J, Olola C, Heward A, et al. Ability of the medical priority dispatch system protocol to predict the acuity of «unknown problem» dispatch response levels. Prehosp Emerg Care. 2008 Jul–Sep;12(3):290–6. [PubMed]
16. Clawson J, Olola C, Heward A, et al. The Medical Priority Dispatch System’s ability to predict cardiac arrest outcomes and high acuity pre-hospital alerts in chest pain patients presenting to 9-9-9. Resuscitation. 2008 Sep;78(3):298–306. [PubMed]
17. Clawson J, Olola C, Scott G, et al. Effect of a Medical Priority Dispatch System key question addition in the seizure/convulsion/fitting protocol to improve recognition of ineffective (agonal) breathing. Resuscitation. 2008 Nov;79(2):257–64. [PubMed]
18. Clawson J, Olola CH, Heward A, et al. Accuracy of emergency medical dispatchers’ subjective ability to identify when higher dispatch levels are warranted over a Medical Priority Dispatch System automated protocol’s recommended coding based on paramedic outcome data. Emerg Med J. 2007 Aug;24(8):560–3. [PMC free article] [PubMed]
19. Neely KW, Eldurkar JA, Drake ME. Do emergency medical services dispatch nature and severity codes agree with paramedic field findings? Acad Emerg Med. 2000 Feb;7(2):174–80. [PubMed]
20. Calle P, Houbrechts H, Lagaert L, et al. How to evaluate an emergency medical dispatch system: a Belgian perspective. Eur J Emerg Med. 1995 Sep;2(3):128–35. [PubMed]
21. Clawson J, Olola C, Heward A, et al. The Medical Priority Dispatch System’s ability to predict cardiac arrest outcomes and high acuity pre-hospital alerts in chest pain patients presenting to 9-9-9. Resuscitation. 2008 Jun 16;
22. Johnson NJ, Sporer KA, Craig AM, et al. Does Emergency Medical Dispatch priority predict Delphi process derived levels of prehospital intervention? (abstract) Prehospital Emergency Care.2009;13:143.
23. Heward A, Damiani M, Hartley-Sharpe C. Does the use of the Advanced Medical Priority Dispatch System affect cardiac arrest detection? Emerg Med J. 2004 Jan;21(1):115–8. [PMC free article][PubMed]
24. Merchant RM, Kurz MM, Gupta R, et al. Identification of Cardiac Arrest by Emergency Dispatch.Academic Emergency Medicine. 2005;12(5, Suppl):457.
25. Neely KW, Norton RL, Schmidt TA. The strength of specific EMS dispatcher questions for identifying patients with important clinical field findings. Prehosp Emerg Care. 2000 Oct–Dec;4(4):322–6. [PubMed]
26. Schmidt T, Neely KW, Adams AL, et al. Is it possible to safely triage callers to EMS dispatch centers to alternative resources? Prehosp Emerg Care. 2003 Jul–Sep;7(3):368–74. [PubMed]
27. Stiell IG NL, Wells GA, Beaudoin T, et al. Multicenter controlled clinical trial to evaluate the impact of advanced life support on out-of-hospital chest pain patients. Acad Emerg Med. 2003 May;10(5):501–2.
28. Stiell IG, Spaite DW, Field B, et al. Advanced life support for out-of-hospital respiratory distress.N Engl J of Med. 2007;356(21):2156–214. [PubMed]


