| Author | Affiliation |
|---|---|
| Sarah Unterman, MD | University of Illinois at Chicago |
| Michael Zimmerman, MD | University of Illinois at Chicago |
| Carissa Tyo, MD | University of Illinois at Chicago |
| Ethan Sterk, DO | University of Illinois at Chicago |
| Lisa Gehm, MD | University of Illinois at Chicago |
| Marcia Edison, PhD | University of Illinois at Chicago |
| Enrico Benedetti, MD | University of Illinois at Chicago |
| Elizabeth Orsay, MD | University of Illinois at Chicago |
ABSTRACT
Background
As solid organ transplants become more common, recipients present more frequently to the emergency department (ED) for care.
Methods
We performed a retrospective medical record review of ED visits of all patients who received an organ transplant at our medical center from 2000–2004, and included all visits following the patients’ transplant surgery through December 2005 or until failed graft, lost to follow up, or death. Clinically relevant demographic variables, confounding and outcome variables were recorded. Kidney, liver and combined kidney with other organ transplant recipients were included.
Results
Five hundred ninety-three patients received kidney (395), liver (161), or combined renal (37) organ transplants during the study period, resulting in 1,251 ED visits. This represents 3.15 ED visits/patient followed over a mean of 30.8 months. Abdominal pain/gastrointestinal (GI) symptoms (31.3%) and infectious complaints (16.7%) were the most common presentations. The most common ED discharge diagnoses were fever/infection (36%), GI/Genitourinary (GU) pathology (20.4%) and dehydration (15%). Renal transplant recipients were diagnosed with infectious processes most often, despite time elapsed from transplant. Liver transplant patients had diagnoses of fever/infection most often in their first 30 days post transplant. Thereafter they were more likely to develop GI/GU pathology. After the first year of transplantation, cardiopulmonary and musculoskeletal pathology become more common in all transplant organ groups. Of the 1,251 ED visits, 762 (60.9%) resulted in hospitalization. Chief complaints of abdominal pain/GI symptoms, infectious complaints, cardiovascular and neurologic symptoms, and abnormal laboratory studies were significantly likely to result in hospitalization.
Conclusions
This study demonstrates a significant utilization of the ED by transplant recipients, presenting with a wide variety of symptoms and diagnoses, and with a high hospitalization rate. As the transplant-recipient population grows, these complex patients continue to present diagnostic and treatment challenges to primary care and emergency physicians.
INTRODUCTION
Since the first successful kidney transplant from a healthy live donor to his identical twin over half a century ago, transplant surgery has emerged as a well established treatment for end-stage organ disease.1,2 At the end of 2004, over 150,000 people were living with a functioning transplant, up from over 91,000 in 1998, with one-year graft and patient survival rates at or above 80–90%.2,3 One-year patient survival rates are somewhat higher for kidney than for liver transplant recipients (96% vs. 87%).3
As the transplant recipient population grows and lives longer, emergency physicians (EP) are increasingly faced with caring for these complex patients with acute and chronic medical and surgical conditions arising from their transplant surgeries, underlying medical conditions, immunosuppressive therapies and comorbidities. Surprisingly little research has been published in the general medical or emergency medicine literature. Review articles are available on specific topics in transplant recipients, including infectious disease treatment principles in transplantation,4 complications that cause liver transplant recipients to visit the emergency department (ED),5 the long-term medical complications for pediatric patients with renal transplants,6 the care of renal transplant recipients in the ED 7 and disease progression, comorbid conditions and patient mortality in renal transplant recipients.8 A few original research articles on the evaluation and care of the transplant patient in the ED provide some information on the infectious and medical complications of renal, liver and heart/lung transplant recipients.9,10,11,12 We describe our ED’s experience with transplant recipients, focusing on frequency and timing of presentation post-transplant, presenting complaints and diagnoses and comparison of liver and kidney transplants.
METHODS
Study Design
We performed a retrospective medical record review of ED visits of all patients who received an organ transplant at our medical center from 2000–2004 using standardized chart review methods.13 We included all ED visits following the patients’ transplant surgery through December 2005.
Setting
The study was conducted at an urban, university-based tertiary care medical center with over 50,000 ED patients per year. The transplant surgery program is well established. Transplants performed here include kidney, liver, combined kidney and liver, and a small number of pancreas, small bowel, heart and lung. The majority of transplant recipients continue their primary healthcare with our institution following their transplants.
Selection of participants
We obtained the patient roster from the Department of Transplant Surgery for all surgeries done from 2000–2004, without exclusions. Solid organ transplants (kidney, liver and combined kidney and liver transplants) were selected for analysis. Appropriate Institutional Review Board approval was obtained.
Methods of Measurement and Data Collection and Processing
Since 1995 this institution has used an electronic medical record (EMR) (Cerner Corporation, Kansas City, MO) that maintains all laboratory, imaging, gastrointestinal, cardiac and urologic procedures, pathology reports, hospitalizations, and both ED and outpatient visits. ED visit documentation consisted of triage, nursing and resident handwritten notes scanned into the database, with the vast majority of ED attending notes entered directly. The few handwritten attending notes were also scanned into the EMR. Registered ED visits without a physician note were considered to be “Left without being seen” (LWBS). ED visits were included for analysis for patients with functioning grafts and excluded for renal transplant recipients with graft failure and on dialysis.
As described in reference 13, the data were collected by trained abstractors (ED physicians) blinded to study hypothesis, using a standardized abstraction form and input data directly into a database (Microsoft OfficeAccess 2003). Each author abstracted one year of transplant patients, with the senior author (EO) assessing chart review and data extraction samples from each year for completeness and consistency. Interobserver reliability was not tested. Data elements included demographics (date and patient age at the time of transplant, gender, race/ethnicity); organ(s) transplanted; source of organ (cadaver, living related or living non-related); pathology leading to organ failure; and co-morbidities. In addition, we recorded the following outcome measures: date of ED visit; number of days post transplant; total number of ED visits; chief complaint; treatments rendered in the ED; ED final diagnosis; disposition and outcome (living, graft failure, death, lost to follow up or care transferred to primary care physician).
Chief complaints were grouped into the following categories: abdominal pain/gastrointestinal symptoms (includes vomiting, diarrhea, gastrointestinal bleed); fever/infection (includes soft tissue infections and abscesses); central nervous system symptoms (dizziness, weakness, headache, focal neurologic deficits); cardiopulmonary symptoms (shortness of breath, peripheral edema, chest pain or hypertension); urinary symptoms (dysuria, decreased urine output or hematuria);and “other” complaints (including clinic referral, musculoskeletal, injury and laboratory abnormalities). One chief complaint was assigned per visit. If more than one was listed, abstractors ascertained the most prominent complaint as listed in the triage note, with oversight by the senior author.
ED final diagnoses were grouped as infection (fever, wound infections, abscesses, urinary tract infections, pneumonia, presumed bacteremia); GI/genitourinary (GU) pathology (noninfectious, including elevated renal/liver function tests, suspected biliary anastomosis stenosis or leakage, hematuria, GI bleed, nausea, vomiting, diarrhea); dehydration; cardiopulmonary pathology (chest pain, hypertension, acute decompensated heart failure, asthma, thromboembolic disorders); musculoskeletal pathology (injury, strain, fracture); electrolyte abnormality; r/o acute/chronic rejection or graft failure; diabetes complications (steroid induced or primary disease); recurrence of primary disease (hypertension, diabetes, hepatitis); neurologic pathology [transient ischemic attach (TIA); cerebrovascular accident (CVA), headache]; hematologic pathology (anemia, thromboycytopenia, neutropenia, sickle cell complications); and other (e.g., dental pain, psychiatric complaints and medication refills). Multiple ED diagnoses were recorded. ED final diagnoses were then analyzed by time elapsed from transplant into the following categories: <30 days, 30 days – one year and > one year post transplant, based on established transplant literature.7
Data were analyzed utilizing Statistical Package for Social Sciences version 15.0 (SPSS Incorporated, Chicago, IL) after extraction from the Microsoft Access database. Statistical methods used in the analysis included cross tabulations, Chi-square analysis and analysis of variance.
RESULTS
From January 2000 through December 2004, 593 patients received kidney, liver or combined kidney and liver transplants. Of these, 13 patients died during their initial hospitalization or at <30 days post operation and 12 were lost to follow up or had their care transferred to an outside facility at <30 days post operation, leaving 568 patients for analysis. Demographic characteristics were: 312 male (54.9%), mean age 44.7 years (SD=15.6), 50 patients (8.8%) under 18; and 47 (8.3%) over 65 years of age. Race/ethnicity characteristics were: 216 (38%) African American, 188 (33.1%) Hispanic, 129 (22.7%) non-Hispanic white, 18 (3.2%) Asian, and 16 (2.8%) with no or “other” ethnicity reported. This was the first transplant for 483 (85%) patients. Forty-one patients (7.2%) died, 50 patients (8.8%) were lost to follow up or had their care transferred to outside facilities/healthcare provider after 30 days post transplant, and 52 patients (9.2%) developed graft failure at some time during the five-year time period of data collection. Patients were followed for a mean of 938 days (30.8 months, SD=557 days).
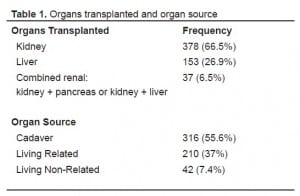
The majority of patients underwent renal transplant alone or in conjunction with pancreas or liver. The most common organ source was cadaveric (Table 1).
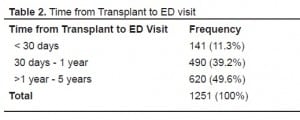
There were 1,251 ED visits by 400 (70.4%) of the transplant recipients. The majority were made by renal patients (66.2%), followed by liver (24.5%) and combined renal (9.3%) transplant recipients, reflecting the organs transplanted distribution in this sample. The mean number of ED visits per patient was 3.15 (SD=3.02) with no statistically significant differences based on organ transplanted or organ source. An ED record was not found for 51 registered ED visits (4.1%) and were considered LWBS (and therefore excluded from analysis) This rate is similar to the 3% rate of LWBS for the general ED population during this period. The distribution of ED visits in relation to time from transplant is shown in Table 2.
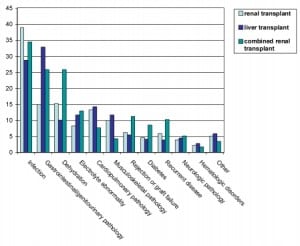
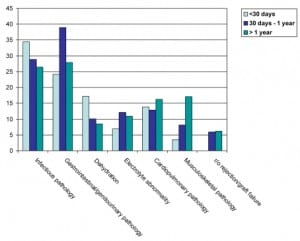
Overwhelmingly, across all transplant types, the most common presenting complaints were abdominal pain and GI complaints (nausea, vomiting, diarrhea and/or GI bleed, 31.3%) and infectious problems (fever, wound infections, abscesses, 16.7%) (Figure 1). Other common presenting symptoms were cardiovascular symptoms (shortness of breath, edema, chest pain, hypertension, 10.9%); neurologic symptoms (dizziness, weakness, neurologic deficits, 10.1%); lab abnormality (7%); urinary symptoms (5.8%); and “other,” which included clinic referral, musculoskeletal pain or injury, psychiatric symptoms, dental pain or other symptoms not fitting into the above categories (16.6%). No presenting complaint was listed for 21 visits (1.7%).
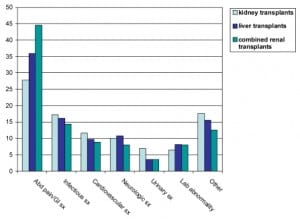
Of the 1,679 ED final diagnoses listed (more than one diagnosis per visit was possible), the most common were fever/infection (36%), GI/GU pathology (20.4%) and dehydration (15%). Diagnoses listed as “other” included a wide variety including psych disorders, dental complaints, medication refills, sent from clinic and others (Figure 2).
There were 81 ED visits with diagnosis of rule out rejection or graft failure. Those patients presented with chief complaints including: abdominal pain and GI complaints (53.1%), fever/infection (14.8%), shortness of breath with or without edema (13.6%), dizziness with or without weakness (6.2%), lab abnormality (6.2%), and other complaints (6.2%). These visits occurred significantly more often among kidney transplant patients (51) than among liver transplant patients (17) (p<0.016) and significantly more often among patients whose organ source was a cadaver (49) versus a living related donor (20) (p<0.006).
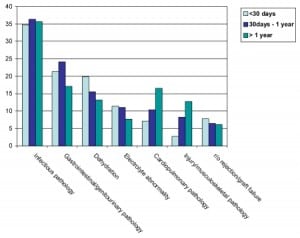
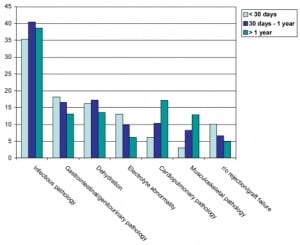
Infectious processes and noninfectious GI/GU pathology were the most common diagnoses in all transplant patients. Infectious diagnoses rates remained fairly constant and prevalent over time, while GI/GU pathology, dehydration and electrolyte abnormalities rates decreased after the first year of transplantation. Conversely, cardiopulmonary diagnoses (including hypertension) and injuries or musculoskeletal pathology rates increased with time elapsed from transplantation (Figure 3).
A total of 1,506 ED treatments were recorded. The most common were IV hydration (513, 34.1%); antimicrobial agents (antibiotics, antivirals and antifungals, 301, 20%); and other pharmaceutical treatments (antihypertensives, antipyretics, pain medications, hypoglycemic agents, antirejection agents and anticoagulation medications, 478, 31.3%). Critical care, including intubation, cardiac resuscitation or resuscitation for clinical shock, was rendered in 43 cases (2.9%).
Of the 1,251 ED visits, 762 (60.9%) resulted in hospitalization. This compares with an overall approximate 17% hospitalization rate for all ED patients during this time period. The chief complaints most likely to result in hospitalization from the ED were abdominal pain/GI symptoms (72.1% hospitalized), cardiovascular complaints (71.2%), fever/infection (70.6%), neurologic symptoms (65.4%), and abnormal labs (61.2%). All were statistically significant compared to all other chief complaints (p<0.05). Conversely, patients presenting with urinary symptoms or other complaints were unlikely to be hospitalized (33.8% and 33.3% not hospitalized, respectively, p< 0.05).
Renal Transplants
Three hundred seventy-eight patients underwent renal transplantation alone. The underlying pathologies leading to their organ failure were diabetes with or without hypertension (286, 75.6%); acquired renal disorders (glomerulonephritis, sclerosis, systemic lupus erythematosis, drug or contrast induced nephropathy; sickle cell anemia, 67, 17.7%); and congenital or structural anomalies (51, 13.5%). Some patients had more than one underlying pathology listed. The most common source of donated organs were living-related (47.6%), followed by cadaver (43.4%) and living non-related (9.0%).
Two hundred sixty five patients (70.1%) generated 828 ED visits, of which 464 (56%) resulted in hospitalization, a significantly lower rate than the hospitalization rate for the overall group (p<0.03). The most common chief complaints were abdominal pain and GI complaints (231, 27.9%) and infectious complaints/fever (143, 17.3%) (Figure 1). The ED discharge diagnoses paralleled these presenting complaints, with the most common being fever/infection (38.8%), dehydration (15.3%) and noninfectious GI/GU pathology (15%) (Figure 2). When analyzed by time elapsed since transplant, infectious processes remained the most common diagnosis and remained high over time. However, GI/GU pathology, dehydration, electrolyte abnormalities and r/o rejection/graft failure all decreased over time, while cardiopulmonary pathology and musculoskeletal pathology increased (Figure 4).
Thirty-seven patients had a renal transplant in combination with either liver or pancreas. Thirty-two (86.5%) of those patients generated 116 ED visits, of which 89 (76.7%) resulted in hospitalization, a significantly higher rate than the overall group (p< 0.001). These patients were notable in that their most prevalent chief complaints were GI complaints or abdominal pain (Figure 1). Their ED final diagnoses were similar to other renal transplant recipients, with infectious processes most common. However, they suffered more from dehydration, r/o rejection or graft failure, diabetes and recurrence of their underlying diseases than the other transplant recipients (Figure 2).
Liver Transplants
One hundred fifty-three patients underwent liver transplantation alone, due to underlying pathologies of: hepatitis A, B or C (90, 58.8%); alcohol abuse (52, 34%); liver carcinoma (28, 18.3%); or congenital/structural abnormalities (10, 6.5%). (More than one underlying pathology may be present). Source of the donated organ was quite different from that of the renal patients, with 77.6 % cadaveric, 17.1% living related and 5.3% living non-related. One hundred three patients (67.3%) had at least one ED visit, with a total of 307. Two hundred nine (68.1%) ED visits resulted in hospitalization, significantly higher than the entire sample (p<0.02). The most common presenting complaint was abdominal pain or GI symptoms (111, 36.2%) (Figure 1) and remained the most common for all elapsed time frames from transplant. Infectious processes were the most common ED diagnosis in the first 30 days following liver transplantation, then declined thereafter. After 30 days post-transplant, noninfectious GI/GU pathology diagnoses were prevalent, peaking during the 30 day – one-year time frame. Similar to the other transplant recipients, cardiopulmonary pathology and musculoskeletal pathology increased as time elapsed from transplant (Figure 5).
DISCUSSION
This large retrospective study demonstrates significant utilization of the ED by transplant recipients, with a wide variety of presenting symptoms and ED diagnoses and a high hospitalization rate. Our data show that transplant patients are most commonly admitted for infectious processes, GI/GU pathology and dehydration, resulting in high rates of antimicrobial use, intravenous hydration and other pharmaceutical treatments. As time elapsed from their transplants, the infectious pathology remained high, the GI/GU pathology, dehydration and electrolyte abnormalities decreased, and the cardiopulmonary and musculoskeletal pathology increased. This is the largest study to date of the ED visit profile of solid organ transplant recipients.
In our hospital’s EMR, the vast majority of ED attending notes are directly entered, with the remaining few scanned in. Clear, concise ED documentation that is easy to access and read made this review feasible. Despite a paucity of published material, two studies, one of liver and one of kidney transplant patients, allow some comparisons. Data for our liver transplant recipients are surprisingly similar to a descriptive study reporting on 143 patients with 290 ED visits.10
They found most common presenting complaints of abdominal (39%), febrile (17%), respiratory (13%) and neurologic (11%) symptoms. This compares to our reported presenting complaints of abdominal pain/GI/GU symptoms (36.2%), febrile/infectious (16.3%), neurologic (10.8%) and cardiopulmonary symptoms (9.8%). They reported similar patterns of ED final diagnoses, with abdominal (27%), infectious (24%), and metabolic (11%) disorders most frequent, compared to our reported discharge diagnoses of noninfectious GI/GU pathology (32.9%), infectious pathology (28.4%) and cardiopulmonary disorders (14.3%). The authors reported a hospitalization rate for their liver transplant patients of 69%, similar to our 68.1% rate. They reported an ED visit rate of 2.0 visits/patient over a mean follow-up time of nine months compared with our 2.0 visits/patient over a mean follow-up time of 30.8 months.
A study of 78 renal transplant recipients presenting to an ED in Turkey12 reported a wide variety of presenting signs and symptoms, with fever most common (26.9%), similar to our findings. That study reported a 57.7% hospitalization rate, similar to our 56%.12
High rates of hospitalizations are inherent in the complexity and risk of serious disease among transplant recipients. A wrong diagnosis or under treatment could have grave consequences for the graft or patient. Their signs and symptoms may be atypical or subtle with significant pathology. Consequently, admission is both prudent and common. Transplant recipients present to the ED with complex problems, both related and unrelated to their transplant. In addition to the post-operative complications, they continue with the morbidities that led to their organ failure, such as hypertension, diabetes, and hepatitis. One author writes in a review of kidney transplant survival, “Despite the introduction of various potent immunosuppressive agents, there has been little or no impact on the prevalence as well as progression of recurrent disease.”15 This is supported by the increasing prevalence of cardiopulmonary pathology with time demonstrated in our data.
Transplant patients are placed on life-long immunosuppressant regimens and are subject to a myriad of acute, recurrent and opportunistic infections.4,7,11,17,18 Furthermore, the medications themselves can cause serious side effects, such as renal tubular damage, neurotoxicity and neutropenia.17,18 Neurologic complications include infection, encephalopathy, seizure, stroke and peripheral neuropathy.19 There are also a variety of long term complications, including steroid-induced diabetes, hypertension, hypercholesterolemia, diarrhea and peptic ulcer disease.20,21,22,23 As patients survive longer, they are subject to increased rates of malignancy as a result of their immunocompromised states, including non-Hodgkin’s lymphoma, squamous cell cancers of the skin, cervical cancer and hepatobiliary cancer.24 Our data demonstrate increased prevalence of injury and musculoskeletal disorders as the time from transplant elapses, possibly due to the effects of long term steroid and immunosuppressive therapy. It is the combination of subtle presentations, prevalence of underlying pathologies and co-morbidities, adverse drug reactions and complications from the immunosuppressant therapies and the potential for serious morbidity inherent in the transplant recipient that makes these patients so challenging. EPs must be aware of these factors to provide the highest level of care.
LIMITATIONS
This study has several limitations. This is a single center, retrospective review, with a primarily minority patient population; 71.1% of the patients in this sample were either African American or Hispanic, and less than one quarter was non-Hispanic white. Racial disparities in renal transplant outcomes have been identified, with African Americans having a shorter graft half-life than other ethnicities.14,15,16 Additionally, post-transplant new-onset diabetes is increased among ethnic minorities, further increasing morbidity and utilization of healthcare resources.16 Ideally, a multi-center study with a large sample would provide more comprehensive data.
Not all ED visits by these transplant recipients were captured in this study, as we report only those to our institution. Patients may have been seen in other EDs during the study period, as some may live far from this institution. If transported by ambulance, the emergency medical system takes patients to the closest ED only. Almost 9% of our patient sample was lost to follow-up some time during the study period. Some patients were intentionally transferred to the care of their referring physicians, while others required nursing home or long term care, and still others moved out of the region.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted March 25, 2008; Revision Received August 17, 2008; Accepted August 17, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Elizabeth M. Orsay, MD. Associate Professor, Department of Emergency Medicine, University of Illinois at Chicago, 1740 W. Taylor, M/C 722, Chicago, IL 60612
Email: Lorsay@uic.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Sayegh MH, Carpenter CB. Transplantation 50 years later – progress, challenges and promises. NEJM. 2004;351:2761–2766. [PubMed]
2. Morris PJ. Transplantation – A medical miracle of the 20th century. NEJM.2004;351:2678–2680. [PubMed]
3. 2004 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1994–2003.Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; Rockville, MD: United Network for Organ Sharing; Richmond, VA: University Renal Research and Education Association; Ann Arbor, MI:
4. Fishman JA, Rubin RH. Infection in Organ-transplant recipients. NEJM.1998;338:1741–1751. [PubMed]
5. Savitsky EA, Uner AB, Votey Sr. Evaluation of orthotopic liver transplant recipients presenting to the emergency department. Ann Emerg Med. 1998;31:507–517. [PubMed]
6. Milliner DS. Pediatric Renal-Replacement Therapy coming of age. NEJM.2004;350:2637–2639. [PubMed]
7. Venkat KK, Venkat A. Care of the Renal Transplant Recipient in the Emergency Department. Ann Emerg Med. 2004;44:330–341. [PubMed]
8. Djamali A, Samagiego M, Muth B, et al. Medical care of Kidney Transplant recipients after the first posttransplant year. Clin J. Am Soc Nephrol. 2006;1:623–640. [PubMed]
9. Sternbach GL, Varon J, Hunt SA. Emergency Department presentation and care of heart and heart/lung transplant recipients. Ann Emerg Med. 1992;21:1140–1144.[PubMed]
10. Savitsky EA, Votey SR, Mebust DP, et al. A Descriptive Analysis of 290 Liver Transplant Patient Visits to an Emergency Department. Acad Em Med. 2000;7:898–905.
11. Trzeciak S, Sharer R, Piper D, et al. Infections and severe sepsis in solid-organ transplant patients admitted from a university-based ED. The American Journal of Emergency Medicine. 2004;22:530–533. [PubMed]
12. Tokalak I, Basaran O, Emiroslu R, et al. Problems in postoperative renal transplant recipients who present to the emergency unit: experience at one center. Transplant Proc.2004;36:184–186. [PubMed]
13. Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg that could be perceived . Med.1996;27:305–308.
14. Chakkera HA, O’Hare AM, Johansen KL, et al. Influence of Race on Kidney Transplant Outcomes within and outside the Department of Veteran Affairs. J Am Soc Nephrol.2005;16:269–277. [PubMed]
15. Hariharan S. Long-term kidney transplant survival. Am J Kidney Dis. 2001;38:S44–S50. [PubMed]
16. Higgins RSD, Fishman JA. Disparities in Solid Organ Transplantation for Ethnic Minorities: Facts and Solutions. Am J Transplant. 2006;6:2556–2562. [PubMed]
17. Freeman L, Awad Sh. Evaluation and management of solid organ transplant patients in the emergency department. Emergency Medicine Reports. 2004;25(2)
18. Chiu LM, Domagala BM, Park JM. Management of opportunistic infections in solid-organ transplantation. Prog Transplant. 2004;14:114–129. [PubMed]
19. Patchell RA. Neurological complications of organ transplantation. Annals of Neurology. 1994;36:688–703. [PubMed]
20. Sheiner P, Magliocca J, et al. Long term medical complications in patients surviving > 5 years after liver transplant. Transplantation. 2000;69:781–789. [PubMed]
21. Adams PL. Long-term patient survival: strategies to improve overall health. Am J Kidney Dis. 2006;47:S65–S85. [PubMed]
22. Gil-Vernet S, Amado A, Ortega F, et al. Gastrointestinal complications in renal transplant recipients: MITOS study. Transplant Proc. 2007;9:2190–2193. [PubMed]
23. Herrero JI, Benlloch S, Bernardos A, et al. Gastrointestinal complications in liver transplant recipients: MITOS study. Transplant Proc. 2007;39:2311–2313. [PubMed]
24. Penn I. The changing pattern of posttransplant malignancies. Transplant Proc.1991;23:1101–1103. [PubMed]