| Author | Affiliation |
|---|---|
| Karim El-Kersh, MD | University of Louisville, Department of Pulmonary, Critical Care, and Sleep Disorders Medicine, Louisville, Kentucky |
| Rodrigo Cavallazzi, MD | University of Louisville, Department of Pulmonary, Critical Care, and Sleep Disorders Medicine, Louisville, Kentucky |
| Mohamed Saad, MD | University of Louisville, Department of Pulmonary, Critical Care, and Sleep Disorders Medicine, Louisville, Kentucky |
| Juan Guardiola, MD | University of Louisville, Department of Pulmonary, Critical Care, and Sleep Disorders Medicine, Louisville, Kentucky |
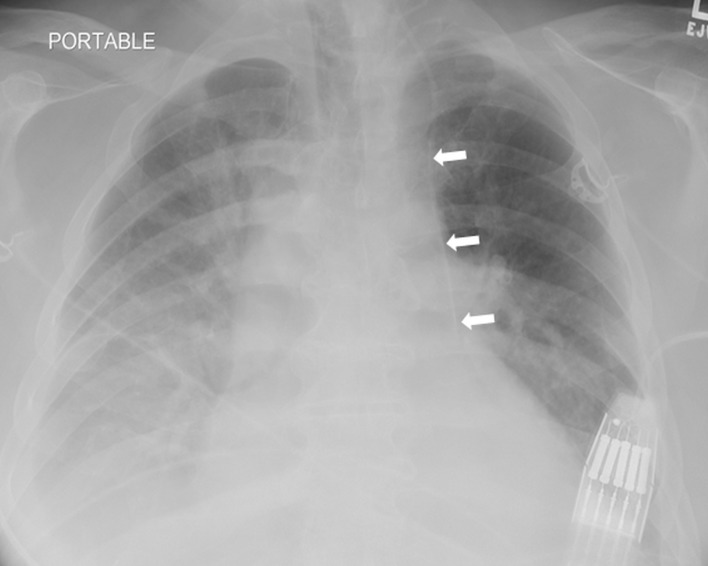
A 62-year-old man presented to the emergency department with hypotension and diarrhea secondary to Clostridium difficile infection. Due to poor peripheral access, a left internal jugular vein triple lumen central venous catheter (CVC) was inserted for fluid resuscitation. The CVC was placed under real-time ultrasound guidance, which revealed normal anatomy, with no resistance during placement. Good blood return was noted in all three ports. Follow-up chest radiograph showed an abnormal course of the CVC (Figure 1). Despite the abnormal course, blood gas analysis and pressure transduction via the CVC were consistent with venous placement. Chest computed tomography without contrast revealed placement of the CVC in the left pericardiophrenic vein (Figure 2).
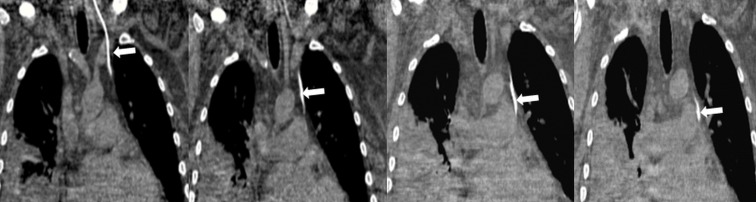
Left paramediastinal central line position can be extravascular with direct placement in the mediastinum or pleural space, arterial with extension into the descending thoracic aorta, or venous. Differential diagnosis of venous left paramediastinal CVC position includes left-sided superior vena cava, left internal mammary vein, left superior intercostal vein and left pericardiophrenic vein.1 The left pericardiophrenic vein accompanies the left pericardiophrenic artery and the left phrenic nerve along the left pericardium before joining the floor of the left brachiocephalic vein opposite to the entrance of left internal jugular vein. Misplaced catheter tip can migrate into the pericardial space resulting in cardiac tamponade due to fluid administration into the pericardium.2 The use of central venous catheters should be postponed, if possible, until a chest radiograph has documented correct placement.
Footnotes
Section Editor: Jeffrey R. Suchard, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Karim El-Kersh, Department of Pulmonary, Critical Care and Sleep Disorders Medicine, Ambulatory Care Building, 550 S. Jackson Street, Louisville, KY 40202. E-mail: karim.elkersh@louisville.edu. 5 / 2015; 16:422 – 423
Submission history: Revision received February 8, 2015; Accepted February 22, 2015
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kazerooni EA, Gross BA. Cardiopulmonary imaging. Philadelphia: Lippincott Williams & Wilkins; 2004.
2. van Haeften TW, van Pampus EC, Boot H, et al. Cardiac tamponade from misplaced central venous line in pericardiophrenic vein. Arch Intern Med. 1988;148:1649-1650.


