| Author | Affiliation |
|---|---|
| Samuel L. Burleson, MD | University of Alabama School of Medicine, Department of Emergency Medicine, Birmingham, Alabama |
| Henry E. Wang, MD, MS | University of Alabama School of Medicine, Department of Emergency Medicine, Birmingham, Alabama |
CASE
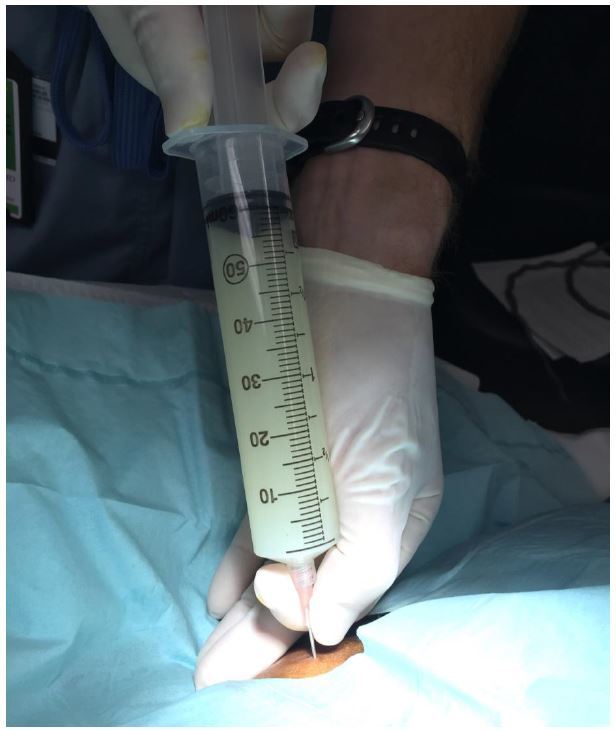
A 58-year-old female with a past medical history of hepatitis C virus-induced cirrhosis presented to the emergency department with three days of increasing abdominal pain, chills, and nausea and vomiting. Abdominal physical examination revealed gross ascites with fluid wave. Diagnostic paracentesis resulted in the aspiration of approximately 60mL of white turbid peritoneal fluid (Figure).
DISCUSSION
The differential diagnosis of turbid peritoneal fluid includes spontaneous bacterial peritonitis, chylous ascites, and pseudochylous ascites. Spontaneous bacterial peritonitis is suggested by a predominance of polymorphonuclear cells, a positive Gram stain or a positive culture.1 Chylous ascites refers to increased concentration of triglycerides (>200mg/dL)2 in the peritoneal fluid, typically the result of traumatic lymphatic obstruction, tumor, tuberculosis, filariasis, congenital abnormalities or nephrotic syndrome.1,2 Cirrhosis may cause up to 11% of atraumatic chylous ascites.3 Pseudochylous ascites results from degeneration of leukocytes or tumor cells without high levels of triglycerides or active infection.4 Chylous and pseudochylous ascites may be differentiated by triglyceride levels.1
Given the patient’s established history of chronic liver disease, the inpatient team focused on spontaneous bacterial peritonitis as the potential etiology for the turbid peritoneal fluid. The patient was treated empirically with antibiotics. Formal abdominal ultrasonography affirmed a cirrhotic liver with large volume ascites and no evidence of mass. Peritoneal fluid cultures were negative for bacterial growth, suggesting that the fluid represented sterile ascites. Triglyceride assays were not performed. Repeat paracentesis on hospital day 3 revealed straw-colored peritoneal fluid. The patient was discharged home on hospital day 4 after clinical improvement.
Footnotes
Section Editor: Rick A. McPheeters, DO
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Henry E. Wang, MD, MS, University of Alabama at Birmingham, Department of Emergency Medicine, 619 19th Street South, OHB 251, Birmingham, AL 35249. Email: hwang@uabmc.edu. 3 / 2016; 17:189 – 190
Submission history: Revision received December 7, 2015; Submitted December 31, 2015; Accepted January 5, 2016
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kasper DL, Braunwald E, Fauci AS, et al. Harrison’s principles of internal medicine. 2005.
2. Al-Busafi SA, Ghali P, Deschênes M, et al. Chylous ascites: evaluation and management. 2014.
3. Steinemann DC, Dindo D, Clavien PA, et al. Atraumatic chylous ascites: systematic review on symptoms and causes. J Am Coll Surg. 2011;212(5):899-905.
4. Runyon BA, Akriviadis EA, Keyser AJ. The opacity of portal hypertension-related ascites correlates with the fluid’s triglyceride concentration. Am J Clin Pathol. 1991;96(1):142-3.


