| Author | Affiliation |
|---|---|
| Caleb P. Canders, MD | University of California Los Angeles Medical Center, Department of Emergency Medicine, Los Angeles, California |
| Gezman E. Abdullahi, MD | Olive View-University of California Los Angeles Medical Center, Department of Internal Medicine, Sylmar, California |
| Jorge A. Diaz, MD | Olive View-University of California Los Angeles Medical Center, Department of Emergency Medicine, Sylmar, California |
| Joshua Hui, MD | Olive View-University of California Los Angeles Medical Center, Department of Emergency Medicine, Sylmar, California |
CASE
A 63-year-old man presented with abdominal distension and shortness of breath for two days. He reported flatus and denied chest pain, anorexia, vomiting, or abdominal pain. Surgical history was notable for left hepatectomy, cholecystectomy and choledochojejunostomy with a Roux-en-Y. He was afebrile with a pulse in the 100s, blood pressure of 130/60, respiratory rate of 34, and oxygen saturation of 92% on room air. Breath sounds were decreased in the lower lung fields and bowel sounds were noted in the chest. Abdominal exam was notable for distension, tympany and normoactive bowel sounds, but no tenderness, rigidity or fluid wave.
Complete cell count, chemistry panel and lipase were normal. Bedside echocardiography was obscured by air. A computed tomography (CT) was obtained. What is the diagnosis?
DIAGNOSIS
Acute intestinal pseudo-obstruction (AIPO)
Also known as Ogilvie’s Syndrome, AIPO is a rare diagnosis seen in patients with history of trauma, recent surgery, neurologic disorder, infection or electrolyte abnormalities.1 Patients present with painless abdominal distension and have normal bowel sounds.2 Plain films show distended bowel without fluid levels. Abdominal CT is typically obtained to exclude mechanical obstruction, perforation or toxic megacolon.1 Most patients improve with fluids, bowel rest and nasogastric decompression. Neostigmine is also a safe and effective treatment.3–5 Surgery is only indicated if conservative therapy fails.1 If cardiac compression or tamponade is present, emergent decompression with percutaneous transabdominal catheterization can be performed.6 Mortality from AIPO is as high as 50%, and is mainly due to ischemic necrosis, perforation and other complications.1
Our patient’s vital signs normalized and his distension improved with fluid resuscitation and nasogastric decompression.
Figures

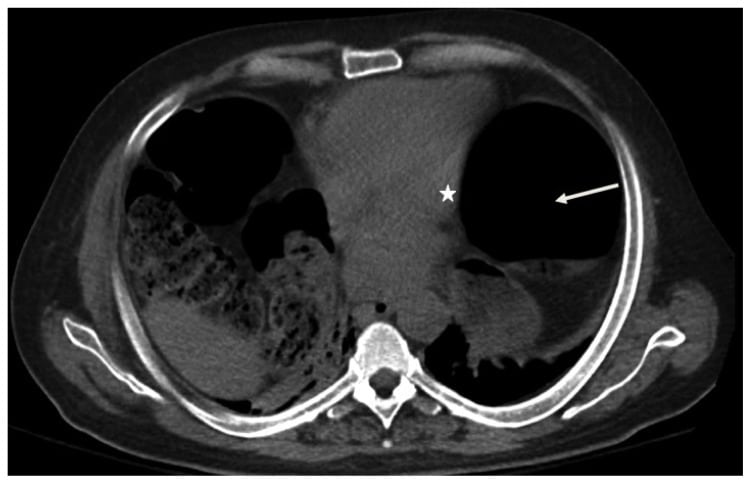
Figure 1
Dilated bowel (solid arrow) compressing the left atrium and lungs. Dilated colon contains stool and gas (dashed arrow).
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Caleb Canders, MD. David Geffen School of Medicine at UCLA, 924 Westwood Boulevard, Suite 300, Box 951777, Los Angeles, CA 90095-1777. Email: ccanders@mednet.ucla.edu. 7 / 2014; 15:354 – 355
Submission history: Revision received December 20, 2013; Accepted January 20, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Ozkurt H, Yilmaz F, Bas N Acute colonic pusedo-obstruction (Ogilvie’s syndrome): radiologic diagnosis and medical treatment with neostigmine. Report of 4 cases. Am J Emerg Med. 2009; 27:757
2 Vicario SJ, Price TG Bowel Obstruction and Volvulus. Tintinalli’s Emergency Medicine. 2004;
3 Ponec RJ, Saunders MD, Kimmey MB Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999; 341:137-41
4 Paran H, Silverberg D, Mayo A Treatment of acute colonic pseudo-obstruction with neostigmine. J Am Coll Surg. 2000; 190:315-318
5 Trevisani GT, Hyman NH, Church JM Neostigmine: safe and effective treatment for acute colonic pseudo-obstruction. Dis Colon Rectum. 2000; 43:599-603
6 Kwon OY, Lee JS, Choi HS Transabdominal decompression of extrapericardial tamponade due to intestinal obstruction. Am J Emerg Med. 2013; 31:441