| Author | Affiliation |
|---|---|
| Teresa A Saultes, DO | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
| Diane Devita, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
| Jason D. Heiner, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, WA |
ABSTRACT
While unsafe abortions have become rare in the United States, the practice persists. We present a 24-year-old female with a 21-week twin gestation who presented to the emergency department with complications of an attempted self-induced abortion. Her complicated clinical course included sepsis, chorioamnionitis, fetal demise, and a total abdominal hysterectomy with bilateral salpingo-oophorectomy for complications of endomyometritis. We discuss unsafe abortions, risk factors, and the management of septic abortion. Prompt recognition by the emergency physician and aggressive management of septic abortion is critical to decreasing maternal morbidity and mortality.
INTRODUCTION
Internationally, approximately 42 million pregnancies are terminated each year with an estimated 20 million terminations in unsafe conditions.1 The World Health Organization estimates that 68,000 women die annually due to the complications of unsafe abortions, with sepsis as the primary cause of death.1,2 Although 97% of unsafe abortions occur in developing countries, today’s emergency physician (EP) may still encounter this rare entity and its complications, which have persisted despite the legalization of abortion here.3 While unsafe abortions in the U.S. are now rare occurrences for which little research exists, recent literature reports of self-induced abortions have predominantly involved adolescents.4,5,6 A 2008 Centers for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report (MMWR) regarding U.S. abortion surveillance estimated the number of deaths for legal and illegal abortions from 1972–2004 to be 393 and 95, respectively.7Although recognized as an underestimation, the CDC has reported between zero and two annual maternal deaths from 1979–2004 in the U.S. due to complications of abortion.7
Roughly 40% of all unsafe abortions are performed on women ages 15–24, and adolescents account for 19% of all reported legal abortions.1,6 Young women choosing to abort may face barriers that lead them to a self-induced or otherwise unsafe termination of pregnancy. In the U.S. the number of abortion providers has decreased and about one-third of women live in a county with no abortion provider. States are increasingly mandating parental involvement in a minor’s decision to have an abortion. In 2001 the inflation-adjusted cost of an abortion rose, with the national average ranging from $350–$900 for a first trimester abortion. 6,8 These issues are likely to influence the young women who will eventually seek care by an EP for complications associated with an unsafe abortion.
We report a case of an attempted self-induced abortion via the intrauterine insertion of a metal coat hanger that was complicated by sepsis. This patient’s presentation illustrates both the major complication of septic abortion and the diagnostic challenge for the EP when a patient conceals the preceding events. We briefly review self-induced abortions and discuss diagnostic strategies as well as the management of the patient presenting with a septic abortion. Finally, we address the role that the EP may play in identifying patients who may be at particular risk for this dangerous entity.
CASE REPORT
A 24-year-old previously healthy female (gravida 3, para 2) arrived by ambulance to the emergency department (ED) with sudden onset of diffuse, severe abdominal pain. She endured emesis and vaginal spotting for one day and a history of irregular menses making her unsure if she were pregnant. Her blood pressure was 82/51 mmHg; heart rate, 113 beats/min; respiratory rate, 22 breaths/min; temperature, 36.4°C (97.5°F); and O2 saturation, 97% on room air. She was given two liters normal saline bolus. She was in obvious discomfort, with a diffusely tender, gravid abdomen, with the contracting fundus just below the umbilicus. Laboratory tests revealed a hematocrit of 25%, white blood cell count (WBC) of 12,000 mm3 and a positive urine pregnancy test. Serum electrolytes, and renal and liver functions were normal. Markers of disseminated intravascular coagulation, prothrombin time (PT), partial thromboplastin time (PTT), fibrinogen, and D-dimer were all normal, as was urine toxicology screen. Fetal heart tones were 177 beats/minute.
Once the obstetrics and gynecology (OB) service was consulted the patient admitted to prior knowledge of her gravid state with no prenatal care. A transabdominal ultrasound revealed a twin pregnancy at 21 weeks gestation, no obvious evidence of abruption, and a significant amount of abdominal free fluid. She then confessed to attempting to end her pregnancy earlier that day by passing a coat hanger deep into her vagina until she felt a “pop,” followed by a gush of fluid and the onset of her abdominal pain. Speculum exam noted no evidence of lower genitourinary injury. Given the patient’s persistent hemodynamic instability and acute abdomen, the general surgery service performed exploratory laparotomy, where one liter of blood was found in her abdomen with a hemostatic wound at the uterine fundus. Broad spectrum antibiotics (ampicillin, gentamicin, and clindamycin) were given. Her postoperative course included sepsis, chorioamnionitis, fetal demise, acute respiratory distress syndrome (ARDS), and a total abdominal hysterectomy with bilateral salpingo-oophorectomy for complications of endomyometritis.
DISCUSSION
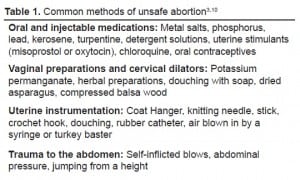
Methods to terminate pregnancy have existed since ancient times. The Chinese Emperor Shen Nung described the use of mercury for inducing abortion 5000 years ago.9 Over 100 methods have been described to induce abortion and can be divided into four categories: oral and injectable medicines, vaginal preparations and cervical dilators, uterine instrumentation, and trauma to the abdomen (Table 1).3,10 All of these can impose a serious threat to the life and well-being of the mother, with abortions later in the pregnancy associated with greater maternal morbidity and mortality.3 Uterine insertion of rigid foreign objects increases the risk of perforation, and intrauterine instillation of soap solutions increases the risk of uterine necrosis, renal failure, central nervous system toxicity, cardiac depression, and respiratory arrest.11 Information about potential methods of unsafe abortions are found in the Internet, lay publications, and common cultural knowledge. For example, a survey of primarily Hispanic women in New York City found that a substantial number were familiar with the use of misoprostol as an abortifacient and 5% had used the method themselves.6
In the U.S. serious complications from abortions requiring hospitalization are estimated to occur less than one per 1,000 abortions.12 Septic abortion, the major complication associated with both legal and illegal abortions, is associated with fever, endometritis, and parametritis, with treatment aimed at eliminating the infectious process.13 While there is a paucity of research regarding the current mortality of sepsis associated with abortion or in pregnant patients, the overall mortality of sepsis in these patients may be as high as 20% to 50%.14 The signs and symptoms, similar to those of pelvic inflammatory disease, include fever, malodorous vaginal discharge, cervical motion tenderness, and pelvic or abdominal pain. In addition, trauma to the cervix or upper vagina may be recognized if there has been an unsafe abortion.15 Infections from septic abortion are usually polymicrobial and include anaerobes (streptococcus, bacteroides), aerobes (Escherichia coli), and sexually transmitted pathogens. Infection from Clostridium perfringens carries a particularly high morbidity and mortality, and in Third World countries tetanus may cause death from septic abortion.2,13
The diagnosis of septic abortion is made clinically and must be considered when any woman of childbearing age presents with vaginal bleeding, abdominal pain, and fever. Typically the patient is young or unmarried and hesitant to reveal that she has had or attempted an abortion; she delays seeking care until she is very ill.13 A positive pregnancy test may indicate either a present pregnancy or a recent pregnancy if the uterus is empty. Other laboratory tests in the evaluation should include a complete blood count, blood type with Rh status, tests of hepatic and renal function, serum electrolytes, prothrombin time, partial thromboplastin time, platelet count, disseminated intravascular coagulation panel, and gram stain and culture of any uterine discharge.16 Ultrasound may reveal retained intrauterine material, intra-abdominal free fluid, and possibly pelvic abscesses. Other imaging modalities include computed tomography and magnetic resonance imaging, which may demonstrate uterine emphysema or intraperitoneal air from uterine perforation.
Because the majority of obstetrical infections are polymicrobial, broad-spectrum antibiotics should be given until the causative organisms are identified. A standard regimen includes ampicillin, gentamicin, and either clindamycin or metronidazole.10,15 The patient’s status of tetanus immunization should also be addressed. Currently there are no evidence-based recommendations specific to the obstetric patient who is critically ill or septic. Early goal-directed therapy has shown to improve survival, although these goals were established in nonpregnant patients. Either crystalloids or colloids may be used for volume expansion, and both inotropes and vasopressors are given by protocol to these ill patients who may also be gravid.17 In general, a transfusion threshold at a hemoglobin of 7.0 to 9.0 g/dL is reasonable, and if time allows, type-specific and CMV-safe (leukoreduced) transfusions are preferred.17 Finally, early consultation with OB and general surgery is imperative as laparatomy may be indicated if there is suspicion of uterine perforation, bowel injury, abscess formation, or clostridial infections.
CONCLUSION
We present a case of a woman with an unwanted pregnancy who attempted self-induced abortion with a coat hanger. The ease of air travel, cultural and educational barriers, and diminishing providers who perform legal abortions all contribute to this disease process. Patients often delay treatment and may present to the ED in florid septic shock. A female presenting with abdominal pain, fever, vaginal bleeding, and a positive pregnancy test mandates the consideration of septic abortion. Early goal-directed therapy and broad-spectrum antibiotics should be given with prompt consultation with OB and general surgery. Early recognition and aggressive management of septic abortion is critical to decrease maternal morbidity and mortality.
Footnotes
This manuscript was written as part of official Department of Defense duties and is in the public domain, and therefore copyright cannot be assigned. The views expressed herein are solely those of the authors and do not represent the official views of the Department of Defense or Army Medical Department.
Supervising Section Editor: Laleh Gharahbaghian, MD
Submission history: Submitted March 11, 2009; Revision Received June 17, 2009; Accepted June 19, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Teresa Saultes, DO, Dept. of Emergency Medicine, Madigan Army Medical Center, Tacoma, WA 98431
Email: teresasaultes@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. World Health Organization Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2000. 4th ed. Geneva, Switzerland: World Health Organization; 2004.
2. Finkielman JD, De Feo FD, Heller PG, et al. The clinical course of patients with septic abortion admitted to an intensive care unit. Intensive Care Med. 2004;30:1097–102. [PubMed]
3. Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet.2006;368:1908–19. [PubMed]
4. Honigman B, Davila G, Petersen J. Reemergence of self-induced abortions. J Emerg Med.1993;11:105–12. [PubMed]
5. Smith JP. Risky choices: the dangers of teens using self-induced abortion attempts. J Pediatr Health Care. 1998;12:147–51. [PubMed]
6. Coles MS, Koenigs LP. Self-induced medical abortion in an adolescent. J Pediatr Adolesc Gynecol.2007;20:93–95. [PubMed]
7. Strauss LT, Gamble SB, Parker WY, et al. Abortion surveillance—United States, 2005 MMWR Surveillance Summaries November282008. 571–32.32Available athttp://www.cdc.gov/mmwr/preview/mmwrhtml/ss5713a1.htm Accessed March 6, 2009.
8. Alan Guttmacher Institute Source Presentation: Trends in abortion in the United States, 1973–2005 January2008. Available at http://www.guttmacher.org/presentations/trends.pdf Accessed March 6, 2009.
9. Glenc F. [Induced abortion—a historical outline] Pol Tyg Lek. 1974;29:1957–8. (polish). [PubMed]
10. Singh S. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. Lancet. 2006;268:1887–92. [PubMed]
11. Burnhill MS. Treatment of women who have undergone chemically induced abortion. J Reprod Med. 1985;30:610–14. [PubMed]
12. Grimes DA, Creinin MD. Induced abortion: an overview for internists. Ann Intern Med.2004;140:620–6. [PubMed]
13. Stubblefield PG, Grimes DA. Current concepts: septic abortion. N Engl J Med. 1994;331:310–14.[PubMed]
14. Fernández-Pérez ER, Salman S, Pendem S, et al. Sepsis during pregnancy. Crit Care Med.2005;33:S286–93. [PubMed]
15. DeCherney AH, Nathan L. Current diagnosis and treatment obstetrics and gynecology. 10th ed. New York, NY: McGraw-Hill; 2007.
16. Stone CK, Humphries R. Current diagnosis and treatment emergency medicine. 6th ed. East Norwalk, CT: McGraw-Hill; 2008.
17. Guinn DA, Abel DE, Tomlinson MW. Early goal directed therapy for sepsis during pregnancy.Obstet and Gynecol Clin N Am. 2007;34:459–79.


