| Author | Affiliation |
|---|---|
| Micah J. Gaspary, MD | Naval Medical Center San Diego, CA |
| Jonathan Auten, DO, PGY-III | Naval Medical Center San Diego, CA |
| David Durkovich, MD | Naval Medical Center San Diego, CA |
| Preston Gable, MD | Naval Medical Center San Diego, CA |
ABSTRACT
Abdominal pain is one of the most common presenting complaints to the emergency department. Mesenteric venous thrombosis represents an important cause to consider in patients with acute abdominal pain. The diagnosis is often delayed, and cases traditionally have been identified either at laparotomy or at autopsy. In this case, we describe a 21-year-old female with acute onset of right lower quadrant pain attributable to a hyperhomocysteinemia related non-occlusive superior mesenteric vein thrombosis. This case highlights how the use of computed tomography in select cases can lead to earlier recognition of this condition and increasingly allow for non-surgical treatment.
INTRODUCTION
Abdominal pain represents one of the most common presenting complaints to United States emergency departments (ED). In 2006 alone, 10% of the 119.2 million visits listed nausea, vomiting and abdominal pain as the chief complaints.1 Only a very small percentage of ED patients with abdominal pain will have appendicitis, and 25% or more of persons presenting with abdominal pain will receive the diagnosis of undifferentiated abdominal pain.1 One of the important causes to consider in the differential of the ED patient with acute or subacute abdominal pain is mesenteric ischemia.
Mesenteric venous thrombosis (MVT) is well established as a cause of intestinal ischemia that is distinct from mesenteric arterial occlusion and accounts for approximately 15% of all mesenteric ischemia cases.2,3 Unfortunately, the symptoms of MVT are subtle and not generally associated with characteristic laboratory abnormalities or distinct physical exam findings. This traditionally led to a delay in diagnosis of this condition until ischemia developed, at which point MVT was most often identified at laparotomy or on autopsy.4,5 The presentation of non-occlusive thrombus can evolve over days to weeks and is often characterized by vague, nonspecific symptoms with delay in diagnosis due to the slow progression of symptoms.6,7 Early identification of the condition allows for conservative treatment with anticoagulation and improved outcomes.8 This case highlights how the use of contrast enhanced computed tomography (CT) in the ED when indicated based on history, physical exam and laboratory findings can lead to earlier diagnosis of MVT.
CASE REPORT
A 21-year-old female presented to the ED with two days of acute, sharp, right lower quadrant pain (RLQ). Her pain had started as periumbilical pain, which migrated to the RLQ. She endorsed one week of nausea and vomiting without anorexia and did not relate pain to meals. She denied any traumatic events. Her past medical history was significant for a gonadal vein thrombosis after the birth of her first child and chronic pelvic pain for the previous seven months. One week prior to her ED presentation, she had completed a six-month course of warfarin for the gonadal vein thrombosis. At the time of presentation, she was on no medications and had no known drug allergies. There was no family history of bleeding or clotting disorders. Her physical exam was significant for RLQ abdominal tenderness without guarding, rigidity or peritoneal signs.
The patient underwent a workup for abdominal pain in the ED consisting of a complete blood count, chemistry panel, urinalysis, liver function tests and lipase, as well as a contrast CT scan of her abdomen and pelvis to evaluate for appendicitis. Basic laboratory values were normal. CT showed a partially occluding thrombus in the superior mesenteric vein (SMV). Her presentation was consistent with intermittent ischemia in a watershed distribution of the cecum, appendix and terminal ileum. The patient was anticoagulated with weight-based enoxaparin and referred to hematology. A detailed outpatient workup revealed elevated serum homocysteine levels, but was negative for other causes of coagulopathy. She has been subsequently treated with vitamin B12, folate and warfarin.
A follow-up CT at one month showed full resolution of the SMV thrombosis, and at six months she had no residual RLQ pain (Figure 1).

DISCUSSION
Various studies show the diagnosis of MVT is associated with mortality rates of approximately 20–38%. Those same studies cite early diagnosis, before the development of intestinal ischemia, and early use of anticoagulation as associated with decreased mortality.3,5,7,8 Improvements in imaging modalities and increased awareness of this condition have led to increasing opportunities for non-operative management.8,9 CT is generally the imaging modality of choice due to its high sensitivity (90–100%), wide availability and relatively low cost. Magnetic resonance imaging (MRI) also has been used to identify the condition and has shown a similarly high sensitivity. Ultrasound with Doppler analysis of flow in the mesenteric and portal venous systems has also been used with success; however, ultrasound reports a lower sensitivity (73–80%) and can be technically difficult to perform and interpret.8 No characteristic laboratory abnormalities are associated with MVT. Observations from a small group of Swedish patients suggest leukocytosis as the most common laboratory abnormality. They also suggest that a normal D-dimer can be used as an exclusion test for this diagnosis, although no reports exist on the reliability of this test for excluding MVT.7
Poor prognostic indicators for MVT include an acute presentation, defined as less than three days of symptoms at presentation, and the presence of bowel ischemia. In general, the diagnosis is characterized by a prodromal period of days to weeks of abdominal pain that is usually out of proportion to physical findings.2,5,9 A study out of Pakistan described 20 cases of MVT and found the most common clinical findings included abdominal pain, abdominal tenderness and absent bowel sounds. Patients were typically older, with the highest proportion of patients presenting between ages 70–79 years.7 A recent meta-analysis found that in contrast to the general presentation of MVT, patients with hyperhomocysteinemia were slightly younger. The mean age of patients in this study was 57 years old.10
Mesenteric vein thrombosis is categorized as primary if no cause is identified or secondary if a hypercoagulable state or other pro-thrombotic condition is present (Table). Hyperhomocysteinemia is one of the known causes of secondary venous thromboembolism (VTE) and is specifically linked to the occurrence of mesenteric thromboses.11–12
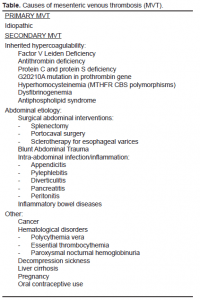
Multiple studies have shown that an increased proportion of patients with MVT have a hypercoagulable state.3,7,9,12 A specific hypercoagulable state is identified in approximately 60–75% of patients with MVT (Table).3,7,9 Prothrombotic states linked to MVT include antithrombin III deficiency, protein C or S deficiency, Factor V Leiden, prothrombin gene mutation, antiphospholipid antibodies, hyperhomocysteinemia, oral contraceptive use and malignancy.3,7 In addition, inflammatory states, post-operative states and trauma have been linked to the development of VTE.3
The link between hyperhomocysteinemia and VTE has been well established.11–14 The mechanism for this increased VTE rate, on the other hand, is not well understood. There are several possible mechanisms for the increase in VTE in patients with hyperhomocysteinemia. A discussion of these is beyond the scope of this case report.11
The majority of recent studies of MVT report increased survival with early initiation of anticoagulation therapy.5,8,9 Patients who are subsequently found to have a prothrombotic state are generally treated with lifelong anticoagulation. Patients with hyperhomocysteinemia are also prescribed supplementation of folate and B vitamins.4,11,15
The decision to perform advanced imaging to assist in diagnosis of undifferentiated abdominal pain relies on history, physical exam and laboratory findings weighed against the risks associated with ionizing radiation of diagnostic studies and contrast media. However, clinicians should consider the earlier use of contrast CT scans in patients with undifferentiated abdominal pain and a known or suspected prothrombotic state. An extensive hypercoagulable work-up in patients diagnosed with MVT is recommended, along with a referral to a hematologist.16,17
CONCLUSION
Abdominal pain represents one of the most common chief complaints of patients presenting to the ED. This case highlights a non-occlusive SMV thrombosis that mimicked the clinical presentation of acute appendicitis. This atypical cause of abdominal pain historically has been difficult to diagnose and resulted in significant mortality and morbidity. Contrast enhanced CT helps to differentiate the etiology of the more than three million cases of undifferentiated abdominal pain seen annually. In the case of mesenteric vein thrombosis, it has led to earlier recognition, which in turn has allowed for increased use of non-surgical treatment. This paradigm shift has led to improved outcomes and decreased mortality in patients that present with mesenteric vein thrombosis.
Footnotes
Supervising Section Editor: Rick A McPheeters DO
Submission history: Submitted October 12, 2010; Revision received November 30, 2010; Accepted December 3, 2010
Reprints available through open access at http://scholarship.org/uc/uciem_westjem
Address for Correspondence: Micah J. Gaspary, 3577 Utah St, San Diego CA
Email: micah.gaspary@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
REFERENCES
1. Pitts SR, Niska RW, Xu J, et al. National hospital ambulatory medical care survey: 2006 emergency department summary. CDC website. Available at:http://www.cdc.gov/nchs/data/nhsr/nhsr007.pdf. Accessed 5 October, 2010.
2. Abdu RA, Zakhour BJ, Dallis DJ. Mesenteric venous thrombosis–1911 to 1984. Surgery.1987;101:383–8. [PubMed]
3. Mock JN, Orsay EM. Primary mesenteric venous thrombosis: an unusual cause of abdominal pain in a young, healthy woman. Ann Emerg Med. 1994;23:352–5. [PubMed]
4. Hotoleanu C, Andercou O, Andercou A. Mesenteric venous thrombosis with bowel infarction and hyperhomocysteinemia due to homozygous methylenetetrahydrofolate reductase C677T genotype.Vasc Endovascular Surg. 2008;42:477–81. [PubMed]
5. Kumar S, Sarr MG, Kamath PS. Mesenteric venous thrombosis. N Engl J Med. 2001;345:1683–8.[PubMed]
6. Rhee RY, Gloviczki P. Mesenteric venous thrombosis. Surg Clin N Am. 1997;77:327–37.[PubMed]
7. Acosta S, Alhadad A, Svensson P, et al. Epidemiology, risk and prognostic factors in mesenteric venous thrombosis. Br J Surg. 2008;95:1245–51. [PubMed]
8. Zhang J, Duan ZQ, Song QB, et al. Acute mesenteric venous thrombosis: a better outcome achieved through improved imaging and a changed policy of clinical management. Eur J Endovasc.2004;28:329–34.
9. Alvi AR, Khan S, Niazi SK, et al. Acute mesenteric venous thrombosis: improved outcome with early diagnosis and prompt anticoagulation therapy. Int J Surg. 2009;7:210–3. [PubMed]
10. Ray JG. Meta-analysis of hyperhomocysteinemia as a risk factor for venous thromboembolic disease. Arch Intern Med. 1998;158:2101–6. [PubMed]
11. Lee R, Frenkel EP. Hyperhomocysteinemia and thrombosis. HematolOncol Clin N Am.2003;17:85–102.
12. Elhajj II, Salem ZM, Birjawi GA, et al. Heterozygous prothrombin 20210G/A mutation, associated with hyperhomocysteinemia, and homozygous methylenetetrahydrofolate reductase 677C/T mutation, in a patient with portal and mesenteric venous thrombosis. Hematol J. 2004;5:540–2.[PubMed]
13. den Heijer M, Rosendaal FR, Blom HJ, et al. Hyperhomocysteinemia and venous thrombosis: a meta-analysis. Thromb Haemost. 1998;80:874–7. [PubMed]
14. Quere I, Gris JC, Dauzat M. Homocysteine and venous thrombosis. Semin Vasc Med. 2005;5:183–9. [PubMed]
15. Bos MJ, den Heijer M. Hyperhomocysteinemia and Venous Thrombosis. Seminars in Thrombosis and Hemostasis. 1998;24:387–91. [PubMed]
16. Soulier K, Delevaux I, Andre M, et al. Mesenteric venous thrombosis: early diagnosis with abdominal CT scan and screening for coagulopathies. Six observations. Revue de Medecine Interne.2001;22:699–705. [PubMed]
17. Rieu V, Ruivard M, Abergel A, et al. Mesenteric venous thrombosis: A retrospective review of 23 Cases. Annales de Medecine Interne. 2003;154:133–8. [PubMed]


