| Author | Affiliation |
|---|---|
| Andy Kahn, MD | Baylor Medical Center at Garland |
| Amy L. Kahn, MD | Baylor Medical Center at Garland |
| J Christian Fox, MD, RDMS | University of California, Irvine Medical Center, Department of Emergency Medicine |
| Mark I. Langdorf, MD, MHPE, RDMS | University of California, Irvine Medical Center, Department of Emergency Medicine |
ABSTRACT
This case study describes a pregnant patient with vaginal bleeding who had a bedside endovaginal ultrasound in the emergency department (ED). The emergency physician identified a live intra-uterine pregnancy (IUP) with another structure that appeared to be a second gestational sac. The patient subsequently had an endovaginal ultrasound in the radiology department 46 minutes later. The attending radiologist described one live IUP and a subchorionic hemorrhage. Comparison of the ED and radiology ultrasound showed that the second structure, identified as a subchorionic hemorrhage, had significantly decreased in size. Endovaginal ultrasound in the evaluation of possible ectopic pregnancy is a useful bedside tool in the ED. We discuss a pitfall that can occur with endocavitary ultrasound when a twin gestation is presumed.
INTRODUCTION
Emergency department (ED) bedside ultrasound is a fast and accessible tool for clinical evaluation of various patient symptoms. This technique allows a more rapid disposition and can aid rapport with patients and improve their education.1 Pelvic ultrasound is one of the six major emergency ultrasound applications.2 An endovaginal probe can reveal findings that help to diagnose a possible live intrauterine pregnancy (IUP), ectopic pregnancy, or abnormal IUP. As vaginal bleeding remains one of the 10 most common reasons for visits to the ED3 and as bleeding occurs in 21% of pregnancies before the twentieth week,4 bedside endovaginal ultrasound has become a mainstay of ED evaluation.
However, the acquisition of bedside ultrasound skills is not without pitfalls. Even experienced ED sonographers can misinterpret images, as bedside ultrasound is limited by patient physiology, the limited image quality of portable equipment, and time constraints. We describe a misinterpretation of an ED ultrasound in the common scenario of first trimester vaginal bleeding.
CASE REPORT
A 24-year-old G3P1A1 Hispanic female presented to the ED at six and one-half weeks by dates with vaginal bleeding of one-day duration, requiring the use of one sanitary pad. She described mild, colicky, bilateral lower quadrant abdominal pain. She denied fever, chills, nausea, vomiting, diarrhea, dysuria, and hematuria. She had a spontaneous abortion one year earlier. The patient had no previous surgeries or medical problems. She was taking no medications and denied alcohol, tobacco, or illicit drugs.
On presentation to the ED, vital signs were: pulse of 86 beats per minute, respiratory rate 20 breaths per minute, blood pressure 129mmHg/62mmHg, temperature 37.5 degrees Celsius and O2 saturation 99% on room air. Physical exam revealed a nontoxic female in no acute distress. Abdominal examination was non-tender and non-distended, with normal bowel sounds. The uterus was not palpable. There was no rebound tenderness or guarding. On pelvic exam, the cervical os was closed and scant blood was noted in the vaginal vault. No active bleeding was present. The patient had a positive Chadwick’s sign. Bimanual exam revealed neither masses nor cervical motion tenderness. The remainder of the physical exam was unremarkable.
Laboratory results revealed: WBC of 9,200 cells/mL, hemoglobin of 13.9 g/dL, hematocrit of 41.2%, and 270,000 platelets/mL. Serum beta human chorionic gonadotropin was 25,845 mIU/mL (normal values for first trimester pregnancy at this institution: 5,000 to 200,000 mIU/mL). Clean-catch urinalysis demonstrated specific gravity of 1.010, pH of 7, no WBCs, 6 RBCs, small leukocyte esterase, large hemoglobin, few bacteria, and negative nitrite, glucose, and ketones. The patient’s blood type was O, Rh positive.
A bedside ultrasound was performed using a 7.5 MHz endovaginal probe (BK Hawk 2102 Ultrasound, Copenhagen, Denmark). Sagittal and coronal planes of the uterus and adnexa were obtained. There was no free fluid in the anterior or posterior cul-de-sacs. The adnexa were visualized and appeared normal, with no evidence of extra-uterine gestation. Two fluid-filled oval structures were noted in the patient’s uterus (Figure 1D). One of the sacs (measuring approximately 1.5cm × 0.7cm) contained a fetal pole and fetal heart motion (labeled G on image). Power flow Doppler was not used because of questionable risk to the fetus5. The second sac (labeled S on image), measured approximately 1.2cm by 0.6cm. In it, a hyperechoic area similar in size and shape to a fetal pole was observed. Fetal heart motion was not visualized in this area. Scanning through sagittal and coronal planes did not uncover any physical connection between these two sacs. The patient tolerated the endovaginal probe without significant pain or complications. The ED bedside ultrasound interpretation was one live IUP with a possible second gestational sac. To better evaluate the sac without cardiac motion, the patient subsequently had an endovaginal ultrasound in the radiology department 46 minutes later (ATL 5500 SonoCT, Bothell, WA). These images are shown in Figure 1 as Radiology Dept Images 1–3 (Figure 1A,B,C). The attending radiologist described one live IUP and a subchorionic hemorrhage. Comparison of the ED and radiology ultrasound showed that the second structure, identified as a subchorionic hemorrhage, had significantly decreased in size. There was no noted increase in vaginal bleeding between ED and radiology scans.
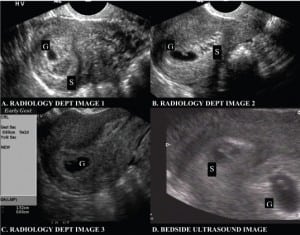
Endovaginal ultrasound with one live intrauterine pregnancy and a separate subchorionic hemorrhage resembling two gestational sacs. (S= subchorionic hemorrhage; G= gestational sac)
The patient was discharged home on pelvic rest with obstetrical follow-up.
DISCUSSION
First trimester vaginal bleeding is a common chief complaint in the ED. It has been shown that EM residents can diagnose live intrauterine pregnancy with good sensitivity (91%) and specificity (99%) when fetal cardiac activity is present.6 In this case, a live IUP was diagnosed. However, a separate finding was unable to be definitively explained. This confusion was despite considerable experience in bedside ultrasound, including endocavitary sonography, by the emergency physician. Therefore, the patient was sent for a pelvic ultrasound in the radiology department. This case illustrates the utility of pelvic ultrasound at the bedside and the importance of recognizing limitations when unsure of sonographic findings.
The emergency physician must rule in an IUP, thereby making the diagnosis of ectopic pregnancy highly unlikely. One in 4000 pregnancies in the general population may include simultaneous IUP and ectopic pregnancy, also known as a heterotopic pregnancy.7 With ovarian hyperstimulation accompanying in-vitro fertilization, heterotopy occurs as often as 1 in 100 pregnancies.8 This patient was noted to have an IUP and no signs of ectopic pregnancy, such as free fluid or adnexal mass.
In addition to an IUP, a pseudogestational sac must be included in the differential diagnosis. Stimulation from an ectopic pregnancy may cause fluid collection in the endometrium, and the physician may miss an important diagnosis of ectopic pregnancy due to the identification of a pseudogestational sac, which has only one hyperechoic ring. Identification of an IUP is confirmed when a gestational sac greater than five millimeters in diameter with a lucent center is surrounded by two concentric and hyperechoic rings, known as the double decidual sign. This sac must be located in the endometrium and contain a fetal pole or a yolk sac. When the gestational sac is larger than 10 millimeters in diameter, lack of cardiac activity in a definite fetal pole or absence of a fetal pole is a probable abnormal IUP. In this case, the ED bedside ultrasound does not show a double decidual sign. However, a hyperechoic structure inside the subchorionic hematoma appears similar to a fetal pole. The images from the radiology department do not display a distinct echogenicity inside the sac. This case adds another diagnosis to be considered when identifying a structure in the uterus. Subchorionic hemorrhage appears as a collection of black fluid on ultrasound.9 Lack of a double decidual sign helps to differentiate it from a true IUP.
The subchorionic hemorrhage seen on the bedside ultrasound resembled a hypertrophied endometrium with scant fluid. These findings can mislead novice sonographers into diagnosing an intrauterine pregnancy.10 The time from ED to radiology sonography allowed the size and shape of the hemorrhage to change, further resembling a subchorionic hemorrhage. Clinical increase in vaginal bleeding was not observed. This is not surprising given that the total volume of the subchorionic hemorrhage first identified in the ED was less than 1cc. The detection of a subchorionic hemorrhage on ultrasound increases the risk for miscarriage, stillbirth, placental abruption, and preterm labor.11 It is controversial whether hematoma size influences the likelihood for carrying a pregnancy to term.12,13,14,15
In this case, an IUP and a subchorionic hemorrhage were both seen on a sonogram performed by the radiology department and initially interpreted as a possible twin gestation on the first ultrasound done by the emergency physician. Correct interpretation of bedside endovaginal ED ultrasound can be challenging and carries high risk. This case highlights the need for cautious interpretation and the importance of pursuing uncertain findings with confirmatory studies and the best available equipment. In other words, in a situation like this one where an IUP and another uncertain finding is present, a formal sonogram must be ordered in order to avoid the pitfall of missing a significant diagnosis when a bedside ultrasound may not be sufficient.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted October 13, 2007; Revision Received December 18, 2007; Accepted January 6, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Andy Kahn, MD. 1717 Main Street, Suite 5200, Dallas, TX, 75201
E-mail: andykahn@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Blaivas M, Sierzenski P, Plecque D, Lambert M. Do emergency physicians save time when locating a live intrauterine pregnancy with bedside ultrasonography? Acad Emerg Med. 2000;7:988–993. [PubMed]
2. Davis DP, Campbell C, Wang J, Poste J. The influence of operator confidence on the accuracy of emergency department ultrasound. Acad Emerg Med. 2003;10:486–487.
3. American College of Emergency Medicine Clinical Policies Committee. Clinical policy for the initial approach to patients presenting with a chief complaint of vaginal bleeding.Ann Emerg Med. 1997;29:435–458. [PubMed]
4. Coppola PT, Coppola M. Vaginal bleeding in the first 20 weeks of fetal pole or pregnancy. Emerg Med Clin North Am. 2003;21:667–677. [PubMed]
5. Hershkovitz R, Sheiner E, Mazor M. Ultrasound in obstetrics: a review of safety. Eur J Obstet Gynecol Reprod Biol. 2002;101:15–18. [PubMed]
6. Loffredo AJ, Dyne PL. Emergency medicine residents can perform beside ultrasound with a high degree of sensitivity and specificity to detect intrauterine pregnancy with cardiac activity. Acad Emerg Med. 2001;8:547.
7. Bello G, Schonoholz D, Moshirpur J. Combined pregnancy: the Mount Sinai experience.Obstet Gynecol Surv. 1986;41:603–613. [PubMed]
8. Dumesic Daniel A, MD, Damario Mark A, MD, Session Donna R., MD Interstitial heterotopic pregnancy in a woman conceiving by in vitro fertilization after bilateral salpingectomy. Mayo Clin Proc. 2001;76:90–92. [PubMed]
9. Dart RG. Role of pelvic ultrasonography in evaluation of symptomatic first-trimester pregnancy. Ann Emerg Med. 1999;33:310–320. [PubMed]
10. Hill LM, Kislak S, Martin JG. Transvaginal sonographic detection of the pseudogestational sac associated with ectopic pregnancy. Obstetrics & Gynecology.1990;75:986–988. [PubMed]
11. Ball RH, Ade CM, Schoenborn JA, Crane JP. The clinical significance of ultransonographically detected subchorionic hemorrhages. Am J Obstet Gynecol.1996;174:996–1002. [PubMed]
12. Bennett GL, Bromley B, Lieberman E, Benacerraf BR. Subchorionic hemorrhage in first-trimester pregnancies: prediction of pregnancy outcome with sonography.Radiology. 1996;200:803–806. [PubMed]
13. Pedersen JF, Mantoni M. Prevalence and significance of subchorionic hemorrhage in threatened abortion: a sonographic study. Am J Roentgenol. 1990;154:535–537.[PubMed]
14. Bloch C, Altchek A, Levy-Ravetch M. Sonography in early pregnancy: the significance of subchorionic hemorrhage. Mt Sinai J Med. 1989;56:290–292. [PubMed]
15. Sauerbrei EE, Pham DH. Placental abruption and subchorionic hemorrhage in the first half of pregnancy: US appearance and clinical outcome. Radiology. 1986;160:109–112. [PubMed]


