| Author | Affiliation |
|---|---|
| Erden Erol Ünlüer | Izmir Ataturk Research and Training Hospital, Department of Emergency Medicine, Izmir, Turkey |
| Adnan Pınar, MD | Izmir Buca State Hospital, Department of Cardiology, Izmir, Turkey |
| Hüseyin Bozdemir, MD | Izmir Buca State Hospital, Department of Cardiology, Izmir, Turkey |
| Serdar Bayata | Izmir Ataturk Research and Training Hospital, Department of Cardiology, Izmir, Turkey |
| Seran Ünlüer, MD | Izmir Buca State Hospital, Department of Cardiology, Izmir, Turkey |
| Özcan Yavaşi, MD | Izmir Ataturk Research and Training Hospital, Department of Emergency Medicine, Izmir, Turkey |
ABSTRACT
We present a case of Wellens’ syndrome together with upright T wave in lead V1 in a man presenting with atypical chest pain, and we discuss the significance of its prompt recognition by the emergency physicians who are involved in the evaluation of patients with coronary artery disease in emergency departments.
INTRODUCTION
As the electrocardiography (ECG) is a simple, noninvasive tool in the diagnosis and management of coronary artery disease (CAD), emergency physicians (EP) must be proficient in the interpretation of ECGs during evaluation of patients in the emergency department (ED). Sometimes specific T-wave changes for coronary artery disease in precordial ECG derivations may be interpreted as nonspecific T-wave changes by EPs. Failure to diagnose these conditions with subsequent inappropriate management may have fatal consequences.
CASE REPORT
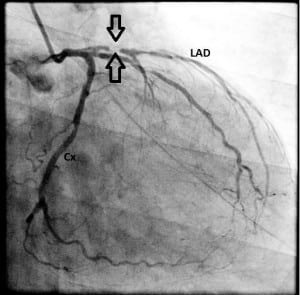
A 67-year-old man presented to the ED with anterior chest pain that did not radiate to the neck and left arm. The pain was localized, tight in nature, and had no association with exertion. The patient came from home where the chest pain initiated and was pain free on admission to the ED. His positive cardiac risk factors were smoking and hypertension. The examination was unremarkable. A 12-lead ECG was performed when the patient was free of discomfort and showed normal sinus rhythm with positive T wave in V1, which was greater than T waves in V6 (Figure 1, upper trace). Serum troponin I concentration was 0.03 ng/ml (normal values <0.04 ng/ml). The patient was admitted to the cardiology service for ECG and cardiac marker follow up. Approximately 4 h later, repeated ECG (Figure 1, lower trace) showed obvious positive T waves in V1 and biphasic T waves in leads V2–3 and negative T waves in V4–5 without chest pain. There were also inverted T waves in lateral leads. Repeated serum troponin I concentration was within the normal range. The electrocardiograph pattern raised the possibility of left anterior descending (LAD) coronary T-wave syndrome. The patient was transferred to another center for cardiac catheterization, which revealed a 95% proximal LAD artery occlusion (Figure 2). The patient underwent emergent percutaneous coronary intervention following coronary angiography with successful outcome.

DISCUSSION
Chest pain is one of the chief presenting complaints among patients attending EDs. Emergency physicians must be able to evaluate these patients and identify those with an underlying life-threatening cause. The ECG is a better predictor of adverse events than history and presenting symptoms in patients with probable acute coronary syndrome (ACS), and it plays a large role in the EP’s disposition decision.1
T-wave abnormalities are the most common ECG abnormality seen in ED patients, occurring in up to 30% of patients with a potential ACS, and their significance has been less clearly defined.2 Studies conducted on cardiac care unit patient populations have shown that, in patients with isolated precordial T-wave inversions, up to 87% have LAD artery stenosis documented at angiography.3 In patients with known CAD, T-wave flattening or inversions raise concern for an ACS; and in patients without known CAD, T-wave abnormalities should still be considered to raise a patient’s 30-day risk. Presence of isolated T-wave abnormalities at the time of ED presentation predict 30-day cardiovascular events, even in patients without a prior history of CAD.4
It has been shown that there is a close association between precordial T-wave inversions and LAD disease in the setting of unstable angina, and 47% of patients presenting with acute myocardial infarction with upright T-waves in V1–V3 had significant LAD disease in coronary angiography.3,5Studies have shown that development of new T-wave changes in the precordial leads (which need not be isolated in midprecordial leads) in patients with unstable angina is a predictor of significant stenosis of the LAD artery and can identify a subgroup of patients with angina with a poor response to medical treatment.3,6–8
In 1982, De Zwann et al9 described a characteristic ECG pattern associated with a critical stenosis of the LAD coronary artery and impending myocardial infarction. Tilkian10 was the first to use the term Wellens’ syndrome defined as a group of ECG signs that occur during the pain-free period in a patient with unstable angina. These ECG changes in the absence of pathologic Q waves are predictive of a critical proximal LAD stenosis.9 They consist of an isoelectric or minimally elevated ST segment followed by a concave or straight ST segment and symmetrically inverted (or biphasic) T waves in the precordial leads, frequently in V2–V3, but sometimes involving V4, V5, or V6.9 This was the case for our patient, who showed biphasic T waves in V2–3 and negative T waves in V4–5 during pain-free period. Other than Wellens’ syndrome, there was a subtle ECG change, which was an upright T wave in V1.
Wellens’ syndrome and positive T waves in lead V1 in patients with chest pain are preinfarction stages of coronary artery disease. Patients with this syndrome present with characteristic ECG findings in the precordial leads. Sometimes more subtle changes precede the development of the Wellens’ syndrome, such as isolated T-wave changes in precordial leads, which are also predictors of advanced LAD lesion and can be easily misinterpreted. While evaluating the ECG on ED settings, one should not forget these red flags for emergency patients. Once these changes have been recognized, cardiology consultation for possible coronary angiography is likely necessary to further evaluate the patient. Stress imaging is strongly discouraged in the presence of suspected left main or left main equivalent lesions and may result in fatal outcome in patients with Wellens’ syndrome.11,12
Without prompt diagnosis and aggressive intervention, patients with Wellens’ syndrome may go on to develop extensive anterior wall myocardial infarction, the majority occurring within a matter of days.9
CONCLUSION
Footnotes
Supervising Section Editor: Amal Mattu, MD
Submission history: Submitted February 11, 2011; Revision received August 17, 2011; Accepted May 31, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.5.6727
Address for Correspondence: Erden Erol Ünlüer
Izmir Ataturk Research and Training Hospital, Department of Emergency Medicine, Basin Sitesi Mahallesi, Gazeteci Hasan Tahsin Caddesi, 35360 Izmir, Turkey
E-mail: erolerdenun@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Jayes RL, Beshansky JR, D’Agostino RB, et al. Do patients’ coronary risk factor reports predict acute cardiac ischemia in the emergency department? A multicenter study. J Clin Epidemiol. 1992;45:621–626. [PubMed]
2. Lindsell CJ, Anantharaman V, Diercks D, et al. The Internet Tracking Registry of Acute Coronary Syndromes (i*trACS): a multicenter registry of patients with suspicion of ACS using standardized reporting guidelines for emergency department chest pain studies. Ann Emerg Med. 2006;48:666–677.[PubMed]
3. Haines DE, Raabe DS, Gundel WD, et al. Anatomic and prognostic significance of new T-wave inversion in unstable angina. Am J Cardiol. 1983;52:14–18. [PubMed]
4. Lin KB, Shofer FS, McCusker C, et al. Predictive value of T-wave abnormalities at the time of emergency department presentation in patients with potential acute coronary syndromes. Acad Emerg Med. 2008;15:537–543. [PubMed]
5. Robbins MJ, Sherman W, Schweitzer P, et al. Precordial T-wave polarity changes in acute inferior infarction. a poor indicator of associated disease of the left anterior descending coronary artery. Chest.1988;94:296–299. [PubMed]
6. Schlant RC, Levine HD, Bailey CC. “Isolated” T-wave negativity in the “ischemic phase” of myocardial infarction in man. Circulation. 1954;10:829–842. [PubMed]
7. Granborg J, Grande P, Pedersen A. Diagnostic and prognostic implication of transient isolated negative T waves in suspected acute myocardial infarction. Am J Cardiol. 1986;57:203–207. [PubMed]
8. Okada M, Yotsukura M, Shimada T, et al. Clinical implications of isolated T wave inversion in adults: electrocardiographic differentiation of the underlying causes of this phenomenon. J Am Coll Cardiol.1994;24:739–745. [PubMed]
9. De Zwann C, Bar FW, Wellens HJJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103:730–736. [PubMed]
10. Conover MB. Understanding Electrocardiography. St Louis, MO: Mosby;; 1996.
11. Ellestad MH. Stress Testing: Principles and Practice. Philadelphia, PA: FA Davis;; 1996.
12. Tandy TK, Bottomy DP, Lewis JG. Wellens’ syndrome. Ann Emerg Med. 1999;33:347–351.[PubMed]


