| Author | Affiliation |
|---|---|
| Csaba Dioszeghy, MD | Yeovil District Hospital NHS Foundation Trust, Somerset, UK |
| Gyorgyi Kamaras, MD | Yeovil District Hospital NHS Foundation Trust, Somerset, UK |
| Aniko Frigyik, MD | Jahn Ferenc Teaching Hospital, Budapest, Hungary |
ABSTRACT
A 65-year-old woman presented to the emergency department after a seizure. An unexplained bradycardia and heart murmur were detected and an emergency bedside echocardiography was performed. This revealed a mass in the left atrium. The provisional diagnosis of left atrial tumor was later confirmed by formal echocardiography and ultimately by histology. The first presentation of primary cardiac tumors can be misleading and sometimes presents with neurological manifestations. An early echocardiography can be diagnostic and could lead to early surgical intervention with better prognosis.
CASE REPORT
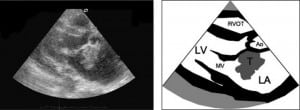
A 65-year-old woman presented to the emergency department after an episode described by bystanders as a short episode of tonic – clonic activity with a complete loss of consciousness. She had no urinary incontinence and suffered no obvious traumatic injury. She had suffered two similar episodes during the preceding few weeks and at the time of presentation was waiting for further neurologic investigations. On admission the patient was oriented without evidence of postictal confusion. Breathing and oxygenation were normal. A slow and irregular heart rate (HR: 40/min) with a blood pressure of 160/100 mmHg were noted. There was a loud systolic murmur at the apex. Atrial fibrillation was recorded on the electrocardiogram. Glasgow Coma Scale was 15, and there was no lateralization or other neurological abnormality. We carried out a bedside echocardiography with suspicion of valvular disease which might have led to the sudden collapse. On the echocardiography a 35 x 28 mm mobile mass was attached to the interatrial septum and floating inside the left atrium (Figure 1).
Following this examination the patient was referred to the cardiothoracic center where further echocardiography raised suspicion for atrial myxoma. Computer tomography (CT) revealed the possibility of multiplex metastatic lesions in the lungs and brain. Unfortunately, the patient’s overall status deteriorated before she could undergo cardiac surgery, and she died 12 days after admission. Autopsy verified a 55 x 35 mm atrial tumor with metastases to the pericardium, both lungs and cerebellum. The tumor was classified as mesothelioma by histology.
DISCUSSION
While primary cardiac tumors are rare, their potentially lethal course could sometimes be avoided with timely diagnosis, hence the importance of early diagnosis and adequate surgical treatment. The incidence of primary cardiac tumors in autopsy series ranges from 0.02 – 2.8 / 1000, with a median age of 50 (range: 1 – 81 years) and with a female male ratio of approximately 6:4.1 About 75% of primary cardiac tumors are benign, most of them being atrial myxoma located in the left atrium.2Mesothelioma is usually also benign, but can occasionally be malignant.2 The clinical symptoms are mostly non-specific and usually originate from one or more of the following main features of these tumors: hemodynamic consequences of the mass obstructing the flow, arrhythmogenic effects due to invasion into the myocardium, distant signs resulting from embolization and systemic non-specific symptoms (anemia, fever, weight loss, etc.).1,2 Mesothelioma often causes pericardial effusion and tamponade but also can present with pericardial constriction.3–5 Benign mesothelioma infiltrating the atrioventricular node, causing conduction disturbances and sudden death, has also been described in the literature.6 Mesothelioma, which infiltrates the atrial wall, can develop an intracavitary pendulous extension mimicking atrial myxoma and can also cause outflow obstruction.7 Approximately 10% of all primary cardiac tumors can be completely asymptomatic.8
Echocardiography is the standard modality for making the diagnosis, although other imaging techniques (magnetic resonance imaging or CT) can be useful for further evaluation. Transthoracic and transoesophageal echocardiography have 95% and 100% sensitivity, respectively.8 However, echocardiography is usually obtained only if there is a suspected cardiac pathology. It is not a routine investigation after a seizure.
Neurological manifestations of atrial tumors have already been described in prior reports. These are either stroke (usually as a result of embolization from the tumor) or seizures caused mainly by cerebral metastasis.4 The intracardiac flapping tumor can cause outflow obstruction, which may result in syncope. However, in many cases the syncope is misinterpreted as a seizure.9 Ekinci et al10reviewed 113 cases with neurological presentations of which 12% had seizures and 28% had syncope. The most common neurological symptoms were ischemic stroke (83%), psychiatric presentations (23%) and headache (15%), of which symptoms often overlapped.10 Sudden hemodynamic collapse has also been described as first presentation of myxoma.11
Benign primary cardiac tumors have a good prognosis if diagnosis is established early and surgical excision is successful. Long term (15 – 20 years) survival was reported as 85–92 % .1 On the other hand, the prognosis of malignant primary cardiac tumors is very poor.2
The importance of early diagnosis of primary cardiac tumors and the fact that this could be easily initiated with a simple and non-invasive technique emphasizes the role of focused bedside ultrasound and echocardiography by emergency physicians. The use of echocardiography by non-cardiology medical practitioners is becoming more accepted.12 Emergency physicians can be trained to perform brief point-of-care focused echocardiographic examinations, which has been shown to be effective in many areas, including assessing left and right ventricular function, recognizing pericardial effusions, and diagnosing valvular abnormalities.12–14 In our case, the cardiac tumor was discovered by the emergency physician trained in bedside emergency echocardiography, and the patient was immediately referred to the cardiothoracic center where detailed examination was carried out.
CONCLUSION
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted September 23, 2009; Revision received January 29, 2010; Accepted February 12, 2010
Reprints available through open access at http://scholarship.org/uc/uciem_westjem
Address for Correspondence: Dr Csaba Dioszeghy, MD, FCEM, Emergency Department, Yeovil District Hospital, Higher Kingston, Yeovil, Somerset, United Kingdom BA22 8QT
Email: c.dioszeghy@btinternet.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kuon E, Kreplin M, Weiss W, et al. The challenge presented by right atrial myxoma. Herz.2004;29:702–9. [PubMed]
2. Vander STJ. Unusual primary tumors of the heart. Semin Thorac Cardiovasc Surg. 2000;12(2):89–100. [PubMed]
3. Meysman M, Noppen M, Demeyer G, et al. Malignant epithelial mesothelioma presenting as cardiac tamponade. Eur Heart J. 1993;149(11):1576–7. [PubMed]
4. Lengyel M. Heart tumors in adults [Hungarian] Orvosi Hetilap. 1989;130(42):2239–44. [PubMed]
5. Kainuma S, Masai T, Yamauchi T, et al. Primary malignant pericardial mesothelioma presenting as pericardial constriction. Ann Thorac & Cardiovasc Surg. 2008;14(6):396–8. [PubMed]
6. Bharati S, Bicoff JP, Fridman JL, et al. Sudden death caused by benign tumor of the atrioventricular node. Arch Intern Med. 1976;136(2):224–8. [PubMed]
7. Lund O, Hansen OK, Ardest S, et al. Primary malignant pericardial mesothelioma mimicking left atrial myxoma. Case report. Scand J of Thorac Cardiovasc Surg. 1087;21(3):273–5. [PubMed]
8. Percell RL, Henning RJ, Siddique PM. Atrial myxoma: case report and a review of the literature.Heart Dis. 2003;5(3):224–30. [PubMed]
9. Moss AJ, Schwartz PJ, Crampton RS, et al. The long QT syndrome. Prospective longitudinal study of 328 families. Circulation. 1991;84:1136–44. [PubMed]
10. Ekcini EI, Donnan GA. Neurological manifestations of cardiac myxoma: A review of the literature and report of cases. Intern Med J. 2004;34(5):243–9. [PubMed]
11. Maruyama T, Chino C, Kobayashi T, et al. A survivor of near sudden death caused by giant left atrial myxoma. J Emerg Med. 1999;17(6):1003–6. [PubMed]
12. Duvall WL, Croft LB, Goldman ME. Can hand-carried ultrasound devices be extended for use by the non-cardiology medical community? Echocardiography. 2003;20(5):471–6. [PubMed]
13. Croft LB, Stanizzi M, Harish S. Impact of frontline, limited, focused and expedited echocardiography in the adult emergency department using a compact echo machine. Circulation.2001;104:II–335.
14. Moore CL, Rose GA, Tayal VS, et al. Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med. 2002;9:186–93. [PubMed]


