| Author | Affiliation |
|---|---|
| Nicholas Sparacino, DO | Banner Good Samaritan Medical Center, Department of Internal Medicine, Phoenix, Arizona |
| Marilyn Geninatti, MD | Carondelet Holy Cross Hospital, Department of Emergency Medicine, Nogales, Arizona |
| Gregory Moore, MD, JD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
ABSTRACT
A 49-year-old white man was admitted to the emergency department with nausea and diarrhea of 11 hours duration. He had experienced crampy abdominal pain as well. He reported that his stools had been dark and malodorous. He had no prior history of gastrointestinal disorders, nor travel, unusual oral or liquid intake. There was a remote history of alcohol abuse, but no hepatitis or cirrhosis. Recent alcohol intake was denied by the patient. He had no medical allergies. His past medical history was pertinent for a history of hypertension, congestive heart failure, and a dual chamber pacemaker insertion. There was no history of diabetes mellitus, smoking, or myocardial infarction. Medications included lisinopril, a small dose of aspirin daily, and thyroid supplement. Family history was negative for cardiomyopathy, sudden cardiac death, gastric or duodenal ulcers, colon cancer, or any congenital abnormalities.
Exam revealed a mildly obese pale gentleman in overt distress. His vitals in triage were a temperature of 97.6°F, blood pressure of 116/49, pulse of 58, and respiration rate of 24.
He was pale and diaphoretic. Exam of the head and neck revealed that he was anicteric, had no parotid enlargement, no telangiectasias, nor petechiae, no oral blood or lesions. His neck was unremarkable with nondistended neck veins, and no thyromegaly or tracheal shift. His chest was clear with a pacemaker pouch seen in the left deltopectoral area. Cardiac exam revealed cool moist slow capillary refill, a heart rate of 120 per minute, and normal heart sounds without rub or S3.
Abdomen exam showed no liver enlargement, hypoactive bowel sounds, no bruit or mass, no discrete tender areas. Genitourinary evaluation was unremarkable for testicular atrophy. He had 4-plus heme-positive stool with melena on exam of the rectum. Extremities were devoid of edema, clubbing, rashes, or petechiae. Neuro exam was nonfocal; he was initially a poor historian with generalized weakness. An arterial blood gas (ABG) with electrolytes and hemoglobin was ordered to get an immediate result and triage the acuity of the gastrointestinal bleeding.
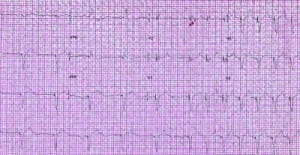
The patient had electrolytes of sodium 128, potassium 5.7 (hemolyzed specimen), low calcium of 4.3, and a hemoglobin of 10.7. The ABG suggested a metabolic debt with a hydrogen carbonate of 17.1. Glucose was elevated at 224 mg/dL. He was also immediately placed on the monitor, both for the complaint, the potential of atypical presentation for myocardial ischemia, and because he had a pulse discrepancy between triage and the initial clinical exam. On the monitor, he was seen to have a pulse of nearly 116 to 120 beats per minute, which was sinus tachycardia, alternating with a sinus rhythm at 60 beats per minute, and with apparent 2:1 block. His initial electrocardiogram (ECG) was recorded and is shown in the Figure. It shows sinus rhythm (sinus tachycardia) at approximately 120 to 128 beats per minute and 2:1 block for the first 6 ventricular beats, followed by 1:1 pacing at approximately 118 beats per minute. (The P-to-P wave interval measures just slightly longer in the last half of the ECGs). The patient received aggressive normal saline fluid resuscitation intravenously, followed by intravenous omeprazole and odansetron. As his hypovolemia corrected, he was noted to have a slowing of his sinus rate and resumption of consistent 1:1 pacing on the monitor. There was no evidence of myocardial injury on the labs for troponin. The patient went to the intensive care unit for evaluation and gastrointestinal and surgical consults.
EXPLANATION
Postventricular atrial refractory period (PVARP) plus atrioventricular (AV) interval equals or limits the upper rate limit. The patient has a physiologic sinus tachycardia, but the pacemaker is not programmed for rates this high. This ECG shows what appears to be 2:1 block in a 2-chambered pacemaker that is in AV synchronous mode, ie, the pacemaker paces the ventricle (synchronizes to the atrial impulse) at a programmed AV interval if no (intrinsic) ventricular beat is seen. This mode is used in patients with stable sinus function but with a disorder of AV conduction, such as prior complete heart block.
Dual pacemakers are also programmed to have an upper rate limit to avoid extremely fast heart rates if the patient develops sinus tachycardia or atrial flutter or fibrillation or if they have retrograde conduction through the AV node. The pacemaker will track or pace heart rates at the prespecified AV interval up to the upper rate limit. Upper rate limits are commonly 120 to 140 beats per minute. Upper rates above this are seldom useful in patients with already compromised cardiac function; thus, the pacemaker programming prevents unwanted congestive symptoms or prolonged tachycardia. PVARP is the period during which the pacemaker is programmed not to recognize or respond to a signal from the atrium. Pacemakers will not synchronize to or pace sinus or atrial impulse during this interval. The sum of the AV interval plus the PVARP defines the upper rate limit. Initially, in pacemaker history, this prevented dual-chambered pacemakers from developing endless loop tachycardia or pacemaker mediated tachycardia (PMT) from retrograde P waves (up to 50% of the population conducts retrograde through the AV node; this is called VA conduction). Thus, dual chambered pacemakers have rate limits that are both physiological and protective for the patient.1–3
It should also be mentioned that many newer pacemakers have algorithms that protect against PMT by automatically extending the PVARP when the upper rate limit is reached. Additionally, the newest generation of dual mode, dual chamber, and dual sensing pacemakers can often distinguish retrograde vs antegrade conduction of P waves, allowing for physiologic tachycardias to be sustained and nonphysiologic (retrograde P waves) terminated.4,5 This patient, usually hypertensive, was in incipient hypovolemic shock. The heart rate of 58 was likely a factor in his initial limited responses and poor perfusion. However, volume resuscitation rather than any change in his pacemaker programming was the only remedy needed. An expensive, time-consuming evaluation by a pacemaker interrogation or, worse, external pacing was unnecessary, since this phenomenon of PVARP was known to exist in dual-chambered pacemakers.
With subtle slowing of the sinus rate, the patient had perfect 1:1 tracking. This phenomenon of alternating (as shown in our Figure) can only happen when the sinus rate is very near the upper rate limit. Even a few millisecond differences in the sinus impulse rate can change the tracking from 1:1 to 2:1. The ECG captured this phenomenon occurring. As long as the patient had a heart rate under 118 beats per minute, he tracked perfectly, indicating his PVARP was the cause of the pseudo 2:1 conduction or block.
Footnotes
Thanks to Jodee Janda for editorial support.
Supervising Section Editor: Amal Mattu, MD
Submission history: Submitted November 24, 2010; Revision received March 9, 2011; Accepted April 8, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.4.2142
Address for Correspondence: Marilyn Geninatti, MD
Carondelet Holy Cross Hospital, Department of Emergency Medicine, 1171 Target Range Rd, Nogales, AZ 85621
E-mail: rocdocmg@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Barold SS. Eccentricities of dual chamber implantable pacemakers. Pacing Clin Electrophysiol.2000;;23:1290–1294. [PubMed]
2. Rognoni G, Occhetta E, Perucca A, et al. A new approach to the prevention of endless loop tachycardia in DDD and VDD pacing. Pacing Clin Electrophysiol. 1991;;14:1828–1834. [PubMed]
3. Ullah W, Stewart A. Pacemaker-mediated tachycardia. Heart. 2010;;96:1062. [PubMed]
4. Nitzsche R, Gueunoun M, Lascault G, et al. Endless-loop tachycardias: description and first clinical results of a new fully automatic protection algorithm. Pacing Clin Electrophysiology.1990;;13:1711–1718.
5. Wilson JH, Lattner S. Undersensing of P waves in the presence of an adequate P wave due to automatic post ventricular atrial refractory period extension. Pacing Clin Electrophysiol.1989;;12:1729–1732. [PubMed]


