| Author | Affiliation |
|---|---|
| Carl J. Smith, BA | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Tareg Bey, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Sherif Emil, MD, CM | University of California, Irvine School of Medicine, Division of Pediatric Surgery |
| Christoph Wichelhaus, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine |
ABSTRACT
Introduction:
Ovarian torsion (OT) occurs primarily in women of child-bearing age, but is rare in the pediatric population. The clinical presentation often consists of nonspecific abdominal complaints making the diagnosis difficult. Radiologic and sonographic evidence can be misleading. Although the delay in diagnosis from symptom onset is common, rapid diagnosis of ovarian torsion is imperative to prevent morbidity.
Case:
We present the case of a four-year-old female who presented to the emergency department (ED) with a five-day history of intermittent abdominal pain and emesis. Initial diagnosis was suspicious for intussusception; however, on operative exploration, she was found to have a right adnexal torsion secondary to an ovarian teratoma. A right salpingo-oophorectomy was performed.
Conclusion:
Early diagnosis of ovarian torsion may increase ovarian salvage and reduce morbidity. Faced with abdominal pain of uncertain etiology in a female child, emergency physicians should include ovarian torsion secondary to an ovarian mass in the differential diagnosis.
INTRODUCTION
Ovarian torsion (OT) in the pediatric population is rare. Although it can be idiopathic, it is frequently due to a cystic or solid ovarian mass. The clinical presentation of OT often consists of vague abdominal complaints, making the diagnosis difficult. 1,2 Initial clinical and sonographic evidence is often misleading.2–5 Cases of OT mimicking various abdominal pathologies have been described in the literature, but OT masquerading as intussusception is not well described.6–8 Although the symptoms of OT are not diagnostically specific, the presentation and examination is almost always strongly suggestive of an acute surgical abdomen. Prompt surgical involvement should not be delayed by diagnostic evaluation under these circumstances. Although the delay in diagnosis from symptom onset is common, rapid diagnosis of ovarian torsion is imperative to prevent morbidity and optimize ovarian preservation.1,9,10 Emergency physicians should consider OT caused by an ovarian mass when evaluating female patients of any age who present with lower abdominal pain.
CASE REPORT
A four-year-old female presented to the emergency department (ED) with a five-day history of severe, intermittent abdominal pain. She initially had several bouts of non-bloody, non bilious emesis that resolved after one day. Two days later, she had intermittent, crampy abdominal pain and tactile fevers. She was seen by her primary medical doctor who treated her for presumed constipation. Two days later, she continued to have episodic severe abdominal pain, recurrence of vomiting and a decrease in appetite and urine output. Upon presentation to the ED, the patient was witnessed to have several bouts of severe abdominal pain.
The patient’s medical history was significant for chronic otitis media requiring myringotomy tubes. She had no recent travel and no pets at home. Her brother at home had nausea and vomiting. The patient was born full-term by an uncomplicated repeat C-section. Medications included milk of magnesia, polyethylene glycol, and acetaminophen. She had no known drug allergies, and her immunizations were up to date.
On examination her vital signs were within normal limits. She appeared non-toxic and playful. On abdominal examination there was mild distention, diffuse tenderness, and mild guarding in the left lower quadrant. Rectal examination was negative for occult blood. While in the ED, the patient continued to have recurrent episodes of colicky abdominal pain.
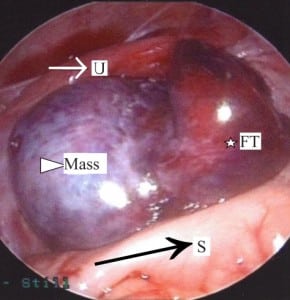
Abnormal laboratory results were limited to an elevated white blood cell (WBC) count of 17.2 103/μL, elevated neutrophils of 12.4 103/μL, a urinalysis with WBC 22/HPF, and a low serum chloride level of 99 mEq/L. An acute abdominal series was unremarkable. A limited pelvic ultrasound (US) demonstrated a mass, measuring 2.9×2.7×2.4 cm, posterior to the bladder and left of midline, without peristalsis or internal vascularity (Figure 1). The radiologist reported the US as highly suspicious for intussusception because it demonstrated the classic target sign. A normal appendix was identified. The sonographic examination was limited due to sudden intense patient pain and consequently the ovaries were not visualized.

Limited pelvic ultrasound demonstrating a rounded mass in the left lower pelvis (arrow and crosses)
The pediatric surgical team was consulted, and the patient underwent diagnositic laparoscopy for treatment of a presumed intussusception with a lead point. Laparoscopy, however, showed no bowel pathology but instead revealed a complete 720° ovarian torsion with necrosis of the entire right fallopian tube and presence of an ovarian mass (Figure 2). On inspection, the liver, diaphragm, peritoneal surfaces, omentum, and pelvis were without evidence of tumor involvement. A laparoscopic right salpingo-oophorectomy was performed. The mass was placed in an endobag and removed piecemeal through a 12 mm trocar. Hair and sebaceous material were noted in the mass, supporting the gross diagnosis of an ovarian teratoma. Pathology confirmed the diagnosis of a benign, mature teratoma. Tumor markers including beta-HCG and alpha-fetoprotein were normal. The patient recovered without complications, and was discharged the following day. She will be followed with an annual examination and US of the contralateral ovary.
The torsed, ischemic left adnexa is seen between the sigmoid colon (black arrow/S) posteriorly and the uterus (white arrow/U) anteriorly. The fallopian tube (star/FT) is severely congested. The mass (triangle) has caused significant ovarian enlargement.
DISCUSSION
Although they can be found at any age, the incidence of benign cystic teratomas is highest during the reproductive years, accounting for 10% to 20% of all benign ovarian tumors.11,12 In a 34-year study of patients presenting with ovarian teratomas (with or without torsion), 44% complained of lower abdominal pain, 25% had a mass or swelling, 21% were found incidentally, and 40% had symptoms of an acute abdomen.13 In children, teratomas are usually benign with surgical removal being curative.9,14 Two-thirds of children with ovarian teratomas have a palpable abdominal mass.3
Ovarian torsion has been defined as total or partial rotation of the adnexa around its vascular axis.2 This torsion interferes first with the venous and lymphatic circulation and progresses rapidly to arterial occlusion. The ovary quickly becomes necrotic, and may cause eventual infection and peritonitis.9 Delayed diagnosis past eight hours makes adnexal preservation unlikely.10,11 Surgical salvage of ovaries in the presence of torsion varies from 0% to 31% among institutions.2,9,15
The clinical features of OT are variable. Houry and Abbott15 described the cardinal features of OT as pain, nausea, vomiting, and rarely fever. Two large reviews of OT reported sudden pain (87% to 100%), nausea/vomiting (59% to 85%), and palpable abdominal mass (63%) as the most common presentations.2,4 Other symptoms may include constipation, fever, or urinary symptoms.1 Pain characteristics of OT are also variable, described as sharp or stabbing (70%), sudden (59%), or radiating to flank, back, or groin (51%). The most common complaint is lower quadrant pain (90%).15 While laboratory and diagnostic tools may aid in diagnosis of OT, they should never delay a surgical consult when OT is clinically suspected. Leukocytosis is present in nearly 50% of patients, while the urinalysis is typically normal.1 Torsion can be intermittent; therefore, diagnostic tests may be negative at the time of examination.1
With an incidence of 3%, ovarian torsion is the fifth most common gynecologic emergency in women.15 The risk of OT complicating a case of ovarian teratoma is approximately 5% to 15% in adults and 3% to 16% in children.13,16,17 Adnexal torsion accounts for up to 2.7% of all pediatric cases presenting with acute abdominal pain. Most reviews report three to five cases of torsion per year at large institutions.10 In one study, 17% of girls who underwent surgery for presumed appendicitis were found to have OT.9OT should therefore be included in the differential diagnosis of the pediatric female patient with abdominal pain.
Intussusception presents most frequently between the ages three months to five years, with 60% occurring in the first year of life.18,19 The classic triad consists of intermittent colicky abdominal pain, vomiting, and bloody mucous stools. This triad occurs only 20–40% of the time, with at least two of these findings occurring in 60% of patients.20 The colicky abdominal pain usually lasts for one to five minutes and then abates for five to 20 minutes with the child often looking better or lethargic between episodes. Frank blood in the stool is a late and unreliable sign for intussusception. No laboratory test reliably excludes or provides a diagnosis of intussusception.1
As seen in our case, the presenting symptoms and physical examination in OT and intussusception can overlap. Abdominal pain and vomiting can be seen with both. The pelvic examination may reveal adnexal tenderness with a mass. In addition, each may present with rebound tenderness.1,16 With younger children, who are unable to have a pelvic examination, ultrasound may be diagnostic.1
The many nonspecific signs and symptoms of OT and intussusception give a vast differential diagnosis for the female patient presenting with an acute surgical abdomen (Table 1). The lack of sensitivity and specificity of clinical parameters for OT vs. intussusception makes the diagnosis difficult. In White’s study, 2 initial clinical suspicion in surgically proven cases of OT existed in only 19.2% of cases.
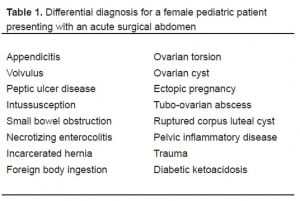
Differential diagnosis for a female pediatric patient presenting with an acute surgical abdomen
The primary diagnostic modality employed for suspected OT is US. The most common finding in female children is an enlarged heterogenous-appearing ovary—also described as an echogenic pelvic mass with no visualization of the ipsilateral ovary.9,21 Doppler technology is not helpful in the diagnosis of OT because results are often equivocal.2,21Emergency physicians have diagnosed OT using bedside US that identified the enlarged ovarian mass and midline shift.4,5,22
Abdominal x-rays are neither sensitive nor specific for intussusception.23,24 Classically, radiographs show a paucity of air in the right upper and lower quadrants with or without a soft tissue mass.25 Many institutions use US to diagnose intussusception, and a Doppler flow study to identify areas of ischemia.26 Classic US findings include the “target lesion” or “doughnut sign,” which is the presence of several concentric rings. The target lesion averages 2.9 cm in diameter in the pediatric population.27 The inner ring represents the proximal portion of the bowel with the outer ring representing the distal portion. Sonography is now considered a reliable means to diagnose intussusception.25 Once diagnosed by US, a barium or air enema can be done with the intent of reducing the intussusception.
Our patient’s radiographs were unremarkable. The US was read as likely intussusception, based on presence of a target lesion and consistent clinical history. The mass seen on US demonstrated no peristalsis and no internal vascularity. These are non-specific signs seen in both OT and intussusception.4,5,27 In retrospect, the radiologist concluded that this mass was the torsed ovary. A second ultrasound radiologist who reviewed the images in a blinded fashion concluded that the images were suspicious for either an ovarian mass or intussusception. He stated that on several views the mass had the appearance of an intussusceptum within an intussuscipiens. Given the clinical history and the limited pelvic ultrasound he agreed that it was a difficult diagnosis to make.
CONCLUSION
Pediatric ovarian torsion is rarely diagnosed in the ED by physical examination or imaging studies. Both sources can be difficult to interpret or misleading. Although laboratory and diagnostic tools may aid in diagnosis of OT, they should never delay a surgical consult when OT is clinically suspected. This case is presented to increase awareness of the key features of ovarian torsion in association with an ovarian teratoma. This difficult diagnosis accentuates the need for emergency physicians to consider OT in the differential diagnosis and workup of females presenting with abdominal pain.
Footnotes
We thank Dr. Joyce Pais for reviewing the abdominal radiographs and Dr. Jeff Janes and Dr. Imelda Ho for reviewing the ultrasound images.
Supervising Section Editor: Paul F. Walsh, MB, BCh, BAO, MSc
Submission history: Submitted May 12, 2008; Revision Received July 7, 2008; Accepted July 14, 2008.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Shahram Lotfipour, MD, MPH. 101 The City Drive South, Rte 128-01, Orange, CA 92868-3298
Email: SHL@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. McCollough M, Sharieff GQ. Abdominal surgical emergencies in infants and young children. Emerg Med Clin N Am. 2003;21:909–935.
2. White M, Stella J. Ovarian torsion: 10-year perspective. Emergency Medicine Australasia. 2005;17:231–237. [PubMed]
3. Sisler CL, Siegel MJ. Ovarian teratomas: a comparison of the sonographic appearance in prepubertal and postpubertal girls. AJR Am J Roentgenol. 1990;154:139–141.[PubMed]
4. Shadinger LL, Andreotti RF, Kurian RL. Preoperative sonographic and clinical characteristics as predictors of ovarian torsion. J Ultrasound Med. 2008;27:7–13.[PubMed]
5. Villalba ML, Huynh B, So M, Mackenzie JD, Ledbetter S, Rybicki F. An ovary with a twist: a case of interesting sonographic findings of ovarian torsion. J Emerg Med.2005;29:443–446. [PubMed]
6. Baker JL, Gull S, Jesudason EC, Abernethy LJ, Losty PD. Appendicitis masquerading as malignancy. Arch Dis Child. 2004;89:481–482. [PMC free article] [PubMed]
7. Hoey BA, Stawicki SP, Hoff WS, Veeramasuneni RK, Kovich H, Grossman MD. Ovarian torsion associated with appendicitis in a 5-year old girl: a case report and review of the literature. J Pediatr Surg. 2005;40:e17–e20. [PubMed]
8. Kienstra AJ, Ward MA. Third place winner Three-year-old female with intermittent ovarian torsion. J Emerg Med. 2002;23:375–377. [PubMed]
9. Kokoska ER, Keller MS, Weber TR. Acute ovarian torsion 252 in children. Am J Surg.2000;180:462–465. [PubMed]
10. Breech LL, Hillard PJ. Adnexal torsion in pediatric and adolescent girls. Curr Opin Obstet Gynecol. 2005;7:483–489. [PubMed]
11. Takeda A, Manabe S, Mitsui T, Nakamura H. Laparoscopic management of mature cystic teratoma of bilateral ovaries with adnexal torsion occurring in a 9-year-old premenarchal girl. J Pediatr Adolesc Gynecol. 2006;19:403–406. [PubMed]
12. Matz MH. Benign cystic teratomas of the ovary: a review. Obstet Gynecol Surv.1961;16:591–594. [PubMed]
13. Ayhan A, Bukulmez O, Genc C, Karamursel BS, Ayhan A. Mature cystic teratomas of the ovary: case series from one institution over 34 years. Eur J Obstet Gynecol Reprod Biol. 2000;88:153–157. [PubMed]
14. Brown MF, Hebra A, McGeehin K, Ross AJ., 3rd Ovarian masses in children: a review of 91 cases of malignant and benign masses. J Pediatr Surg. 1993;28:930–933. [PubMed]
15. Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med.2001;38:156–159. [PubMed]
16. Wittich AC. Adnexal torsion presenting as an acute abdomen in a patient with bilateral cystic teratoma of the ovary. J Am Osteopath Assoc. 2002;102:231–233.[PubMed]
17. Benjapibal M, Boriboonhirunsarn D, Suphanit I, Sangkarat S. Benign cystic teratoma of the ovary: a review of 608 patients. J Med Assoc Thai. 2000;83:1016–1020. [PubMed]
18. Parashar UD, Holman RC, Cummings KD, et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000;106:1413–1421.[PubMed]
19. Ugwu BT, Legbo JN, Dakum NK, et al. Childhood intussusception: a 9-year review.Ann Trop Paediatr. 2000;20:131–135. [PubMed]
20. Kuppermann N, O’Dea T, Pinckney L, et al. Predictor of intussusception in young children. Arch Pediatr Adolesc Med. 2000;154:250–255. [PubMed]
21. Servaes S, Zurakowski D, Laufer MR, et al. Sonographic findings of ovarian torsion in children. Pediatr Radiol. 2007;37:446–451. [PubMed]
22. Johnson S, Fox JC, Koenig KL. Diagnosis of ovarian torsion in a hemodynamically unstable pediatric patient by bedside ultrasound in the ED. Am J Emerg Med.2006;24:496–497. [PubMed]
23. Smith DS, Bonadio WA, Losek JD, et al. The role of abdominal x-rays in the diagnosis and management of intussusception. Pediatr Emerg Care. 1992;8:325–327. [PubMed]
24. Yang ST, Tsai CH, Chen JA. Differential diagnosis between intussusception and gastroenteritis by plain film. Zhonghua Min Guo Xiao Er Ke Yi Xue Hue Za Zhi.1995;36:170–175.
25. Byrne AT, Goeghegan T, Govender P, Lyburn ID, Colhoun E, Torreggiani WC. The imaging of intussusception. Clinical Radiology. 2005;60:39–46. [PubMed]
26. Bhisitkul DM, Listernick R, Shkolinik A, et al. Clinical 294 application of ultrasonography in the diagnosis of intussusceptions. Pediatr J. 1992;121:182–186.
27. Ko SF, Lee TY, Ng SH, et al. Small bowel intussusception in symptomatic pediatric patients: experience with 19 surgically proven cases. World J Surg. 2002;26:438–443.[PubMed]


