| Author | Affiliation |
|---|---|
| Mohammad Jalili, MD | Tehran University of Medical Sciences, Department of Emergency Medicine, Tehran, Iran |
| Reza Azizkhani, MD | Tehran University of Medical Sciences, Department of Emergency Medicine, Tehran, Iran |
ABSTRACT
A 32-year-old man presented to the emergency department (ED) with lower abdominal pain and constipation. He related chronic ingestion of large amounts of opium. Physical examination showed mild abdominal tenderness and gingival discoloration. Diagnostic studies showed a mild hypochromic, microcytic anemia with basophilic stippling of the red blood cells. Abdominal imaging showed no intra-abdominal pathology. A diagnosis of lead toxicity was confirmed through serum lead levels. The patient was put on chelation therapy and his signs and symptoms started to resolve. As a comprehensive search for other sources of lead was unsuccessful, opium adulterants were considered as the culprit. Chemical analysis of the opium confirmed this. Contaminated drugs have been reported as a source of exposure to toxins such as arsenic or lead. While other reports deal with patients from clinics, this report illustrates lead toxicity from ingestion of contaminated opium in the ED.
INTRODUCTION
Lead poisoning is the most common toxicity of environmental origin in the United States (U.S.).1 One in every 20 children in the U.S. has toxic blood levels,2 while three million or more adult workers are estimated to be at risk for toxic lead exposure.3 Exposure may result from ingestion or inhalation of lead compounds. It may also be due to direct skin contact with organic lead or resorption from a retained bullet in joints. Although the incidence of occupational and adult lead poisoning has declined,4 the problem still exists in various parts of the world. Chronic lead toxicity often presents gradually and is nonspecific. Characteristic symptoms and signs of acute lead poisoning include abdominal colic, malaise, nausea, vomiting, constipation, fatigue, anemia, peripheral neuropathy, renal impairment, hepatic disorder, and CNS dysfunction.5 Abdominal pain is one of the common manifestations of lead poisoning and sometimes brings the patient to the emergency department (ED). For the emergency physician (EP), however, this is a challenging diagnosis, due to rarity of the disease combined with the complexity of the presentations. Furthermore, exposure to lead is usually considered only when the patient’s history points to well-known traditional sources of lead, such as paint or printing material. However, unusual and exotic causes of chronic lead poisoning have been described. Examples include adulterated marijuana,6Indian herbal medicine,7 and “moonshine” whiskey.
We report a case of chronic lead poisoning, which occurred as a result of chronic ingestion of opium adulterated with lead.
CASE REPORT
A 32-year-old man presented to our ED with five weeks of abdominal pain. It was constant and, though diffuse, was worse in the lower abdomen. It did not radiate to the back, arms, or chest and was not associated with food. He reported constipation for two weeks, which did not respond to laxatives. He also had loss of appetite but denied nausea or vomiting. The pain was not accompanied by chills, diarrhea, or other symptoms. No recent weight loss was reported.
He had no significant co-morbidity such as hypertension, diabetes, or ischemic heart disease, and he had not been hospitalized. He was addicted to opium, and stated that he ingested about 20 grams per day. He conceded that he had obtained opium from the black market, from the same source for many years. He denied intravenous injection. He underwent a course of ultra-rapid detoxification about two months previously, but resumed consumption of opium two weeks later. His medications included ranitidine, vitamin B6, and hyoscine (all without prescription). He was unemployed at the time of presentation but had worked as a janitor, and had no known exposure to lead.
His vital signs were stable: blood pressure, 100/70 mmHg; pulse rate, 80 beats per minute; and respiratory rate, 14 breaths per minute; pulse oximetry, 98% on room air, and temperature, 98.3°F (37°C). His head and neck examination revealed a dark line along the gingival margin. Chest examination was normal. Abdomen revealed mild tenderness to deep palpation of the lower abdomen, without rebound, guarding, or costovertebral angle tenderness. Neurological examination was normal. Laboratory results are presented in Table 1.
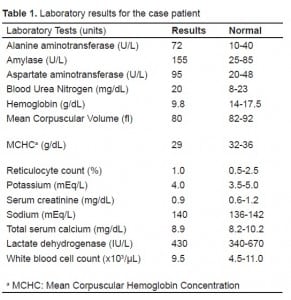
A peripheral blood smear revealed basophilic stippling of red cells. An abdominal ultrasound, computed tomography scan with intravenous and oral contrast of the abdomen were normal. The presentation, physical findings, lab studies and lack of another explanation led the EP to suspect lead toxicity. He was admitted to the floor, and a whole blood lead level result was 50 μg/dL (2.42 μmol/L). The diagnosis of lead toxicity was made and the patient was put on chelation therapy with 2,3-dimercaptosuccinic acid (DMSA). His abdominal pain subsided over the next week and he was discharged. Marked resolution of all signs and symptoms occurred by one-month follow up. As thorough investigation of the patient’s past history failed to reveal any other source of exposure except opium, lead toxicity was attributed to the adulterants of opium. Analysis of the opium obtained from the patient’ house, performed by atomic absorption measurement using a Shimadzu AA670 atomic absorption spectrometer (Shimadzu, Japan), showed 35.2 mg of lead per 100 g of opium.
DISCUSSION
Toxic effects of lead may occur acutely after a single exposure or, more commonly, through chronic low-level exposure. Recognition of lead poisoning depends on a high index of suspicion and a thorough patient history. The insidious onset, non-specific complaints,8 and lack of diagnostic signs facilitate the missed diagnosis of lead poisoning. Lead poisoning should be considered in the differential diagnosis of abdominal pain.9 The combination of abdominal or neurological dysfunction with a hemolytic anemia should raise the suspicion of lead toxicity. The definitive diagnosis of lead poisoning rests on finding an elevated blood lead level, regardless of symptoms.10
All patients with symptoms consistent with lead toxicity and an elevated blood lead level should be treated. Treatment includes British anti-Lewisite (BAL) or succimer (DMSA) with or without CaNa-EDTA.11
Some traditionally recognized sources of lead exposure include lead smelting, battery, rubber and plastic manufacturing, printing, and soldering of lead products.12 While attempts have been made to contain these sources of exposure to lead, some others such as herbal medicine7 and adulterated drugs6 are emerging and are worthy of noting.
Opium is still one of the most frequently abused drugs. Informal, and often illegal, laboratories refine opium into a sticky, brown paste, which is pressed into bricks and sun dried. This material can then be ingested or smoked. This process results in introduction of impurities such as lead into the product. On the other hand, lead is sometimes deliberately added to opium by the smugglers to increase its weight during trading. Although the amount of lead in opium is usually small,13 when taken in large amounts opium adulterated with lead can produce clinical toxicity.
Intravenous injection of adulterated drug and inhalation of contaminated heroin have previously been mentioned as a source of lead poisoning in drug addicts.14 Lead toxicity has also been reported in a case series from Germany following smoking of adulterated marijuana.6 Opium has previously been reported as a source of both arsenic and lead poisoning.13–18 In 1973, in the earliest report of this peculiar source of lead, a middle-aged Chinese woman and her father were diagnosed to suffer from lead poisoning due to ingestion of home-made opium.18 More recently, three cases have been reported from a central province in Iran.19 All were middle-aged men who had been admitted for abdominal pain. The case we are reporting is another piece of evidence showing the relationship between opium ingestion and lead poisoning. Furthermore, to the best of our knowledge, there has been no report of such cases from the ED. It is interesting that this chronic complication lead to an acute presentation, which brought the patient to us. It is therefore very important for the EP to keep this diagnosis in mind when facing a patient with vague abdominal pain.
CONCLUSION
Metabolic processes, including lead poisoning, should be considered in the differential diagnosis of abdominal pain, especially when its cause is unclear. The sources of lead are numerous and, with new products and processes the list must be updated. In cases of consumption of illicit drugs and substances, where the ingredients and the processing method are not known, the suspicion should be investigated more vigorously. Our case emphasizes the need for a thorough history, including details of social habits in patients with cryptic abdominal pain.
Footnotes
Supervising Section Editor: Jeffrey R. Suchard, MD
Submission history: Submitted September 10, 2008; Revision Received July 5, 2009; Accepted July 5, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Mohammad Jalili, MD, Department of Emergency Medicine, Tehran University of Medical Sciences, Keshavarz Blvd., Tehran, Iran
Email mjalili@tums.ac.ir
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Landrigan PJ, Todd AC. Lead poisoning. West J Med. 1994;161:153–9. [PMC free article] [PubMed]
2. Markowitz G, Rosner D. Cater to the children: the role of the lead industry in a public health tragedy, 1900–1955. Am J Public Health. 2000;90:36–46. [PMC free article] [PubMed]
3. Paloucek FP. Lead poisoning. Am Pharm. 1993;33:81–8. [PubMed]
4. Prickle JL, Brody DJ, Gunter EW, et al. The decline of blood lead levels in the United States: The National Health and Nutrition Examination Surveys (NEHANES) JAMA. 1994;272:284–91. [PubMed]
5. Cullen MR, Robins JM, Eskenazi B. Adult inorganic lead intoxication: presentation of 31 new cases and a review of recent advances in the literature. Medicine (Baltimore) 1983;62:221–47. [PubMed]
6. Busse F, Omidi L, Timper K, et al. Lead poisoning due to adulterated marijuana. NEJM.2008;358:1641–2. [PubMed]
7. Dundabin DW, Tallis GA, Popplewell PY, et al. Lead poisoning from Indian herbal medicine (Ayurveda) Med J Aust. 1992;157:835–6. [PubMed]
8. Hettmansberger TL, Mycyk MB. Lead poisoning presents a difficult diagnosis. Am Fam Physician.2002;66:1839–40. [PubMed]
9. Sood A, Midha V, Sood N. Pain in abdomen-do not forget lead poisoning. Indian J Gastroenterol.2002;21:225–6. [PubMed]
10. Centers for disease control and prevention: screening young children for lead poisoning: guidance for state and local public health officials. Atlanta: CDC; 1997.
11. Lifshitz M, Hashkanazi R, Phillip M. The effect of 2,3-dimercaptosuccinic acid in the treatment of lead poisoning in adults. Ann Med. 1997;29:83–5. [PubMed]
12. Heneretig F. Goldfrank LR Goldfrank’s toxicologic emergencies. 6th ed. Stamford, CT: Appleton & Lange; 1998. Lead; pp. 1277–1309.
13. Aghaee-Afshar M, Khazaeli P, Behnam B, et al. Presence of Lead in Opium. Arch Iran Med.2008;11:553–4. [PubMed]
14. Algora M, Martin-Castillo A, Zabala P, et al. Lead poisoning due to drug addiction: a new source of poisoning with clinical interest and important epidemiological consequences. Ann Med Interna.1989;6:483–5.
15. Jayasinghe KS, Misbah SA, Soosainathan S, et al. Contaminated opium as a source of chronic arsenic poisoning in Sri Lanka. Ceylon Med J. 1983;28:22–7. [PubMed]
16. Datta DV. Arsenic adulteration in opium (Arsenicosis-a real danger to health in developing countries) J Assoc Physicians India. 1978;26:223–7. [PubMed]
17. Narang AP, Chawla LS, Khurana SB. Levels of arsenic in Indian opium eaters. Drug Alcohol Depend. 1987;20:149–53. [PubMed]
18. Chia BL, Leng CK, Hsii FP, et al. Lead Poisoning From Contaminated Opium. Br Med J. 1973;1:354.[PMC free article] [PubMed]
19. Masoodi M, Zali MR, Ehsani-Ardakani MJ, et al. Abdominal pain due to lead-contaminated opium: a new source of inorganic lead poisoning in Iran. Arch Iran Med. 2006;9:72–5. [PubMed]


