| Author | Affiliation |
|---|---|
| Ryan W Coates, DO | Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, Allentown, Pennsylvania |
| Kevin R Weaver, DO | Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, Allentown, Pennsylvania |
| Rezarta Lloyd, DO | Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, Allentown, Pennsylvania |
| Nicole Ceccacci, DO, | Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, Allentown, Pennsylvania |
| Marna Rayl Greenberg, DO, MPH | Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, Allentown, Pennsylvania |
ABSTRACT
Infants with food protein-induced enterocolitis syndrome (FPIES) may present to the emergency department (ED) with vomiting and hypotension. A previously healthy, 5-month-old male presented with vomiting and hypotension 2 to 3 hours after eating squash. The patient was resuscitated with intravenous fluids, antibiotics, and admitted for presumed sepsis. No source of infection was ever found and the patient was discharged. The patient returned 8 days later with the same symptoms after eating sweet potatoes; the diagnosis of FPIES was made during this admission. Two additional ED visits occurred requiring hydration after new food exposure. FPIES should be considered in infants presenting with gastrointestinal complaints and hypotension. A dietary history, including if a new food has been introduced in the last few hours, may help facilitate earlier recognition of the syndrome.
INTRODUCTION
Food allergies are prevalent in the first 2 years of life (between 1%–10% of the population) and are usually immunoglobulin E (IgE) mediated hypersensitivity reactions.1 Food protein-induced enterocolitis syndrome (FPIES) is a severe non-IgE mediated food hypersensitivity reaction that frequently goes unrecognized and misdiagnosed at the initial presentation.2–7 Symptoms usually occur before 9 months of age within 4 hours of ingesting the provoking agent and consist of profuse vomiting, diarrhea (sometimes bloody), lethargy, acidosis (mean pH 7.03), and dehydration.6 It is unknown what percentage of patients present to the emergency department (ED) versus primary care settings, but hypotension is seen in 20% of the cases and transient methemoglobinemia (including clinical cyanosis) may also be seen in about one-third of the cases.2–6,8,9
Unrecognized FPIES can lead to multiple admissions for sepsis workups, or for anemia, and failure to thrive, which occur presumably from malabsorption and/or rectal bleeding.2,3 While the most common provoking foods are cow’s milk and soy protein based formulas, FPIES has also been documented with solid foods of low allergenicity, such as cereals, vegetables, and poultry.2–6 FPIES is a clinical diagnosis that can be made after a thorough dietary history. It should be considered in the differential diagnosis of infants presenting to the ED with predominant gastrointestinal signs and symptoms of sepsis particularly in the absence of fever and recurrent presentations.
CASE REPORT
A 5-month-old previously healthy male presented to the ED with a chief complaint of altered mental status and respiratory distress after 2 to 3 hours of sudden vomiting and 1 blood streaked stool. He was born full-term by spontaneous vaginal delivery without complication and up-to-date with vaccinations. The patient was lethargic; his eyes were open but did not track, he made no cry, and he was minimally responsive to pain. His initial blood pressure (BP) was unobtainable, pulse (HR) 189, respirations (RR) 73 and shallow, but with normal oxygen saturation (100%) on room air. His skin was pale and capillary refill was greater than 5 seconds, and he had a rectal temperature of 38.7°C. He had no wheezes or crackles; his abdomen exam revealed no distention or mass, and normal bowel sounds were present. A sepsis evaluation was initiated and the patient was found to have leukocytosis of 26.6 × 109 cells per L with 75% neutrophils and a platelet count of 694 × 109 cells per L. He had evidence of acidosis with venous CO2 of 17 mEq/L. Chest and abdominal radiographs were negative for infiltrates, free air, bowel edema, or intramural air. Urinalysis demonstrated no evidence of urinary tract infection.
After intravenous (IV) fluid boluses totaling 20 cc/kg, the infant’s skin color, capillary refill, and activity improved. After this first hour of resuscitation, the BP was finally obtainable at 97/70, and other vitals were improving (HR 150, RR 50). The patient was given empiric antibiotics and admitted to the pediatric ICU for presumed sepsis. Over the next 72 hours, urine, cerebrospinal fluid, and blood cultures were negative and the child improved clinically. Soon after he returned to his baseline functional status and was discharged home without further antibiotic treatment. During his hospital stay, it was discovered that his parents were introducing new foods into his diet. Consideration was given to possible food allergies, and the patient was referred for outpatient follow up.
The patient returned to the ED 8 days after hospital discharge for a recurrence of the same symptoms. A few hours after ingesting sweet potatoes, he became lethargic with profuse vomiting and bloody diarrhea. His vital signs were BP 110/64, HR 160, RR 52, and pulse oxygen saturation 100%. Fever was notably absent (37.3°C rectal) with this episode, but the patient was thought to be in septic shock. During this second hospital admission, sepsis workup was again negative, and the child responded well to IV fluid boluses, and empiric antibiotics were again administered. He returned to baseline and was tolerating formula within 3 days. Consultation with an allergist revealed the episodes occurred after ingesting squash and sweet potatoes, respectively, both new foods to the patient’s diet. The diagnosis of FPIES was made. The patient underwent outpatient IgE allergen testing, which was negative.
The patient was brought to the ED for a third time, 4 weeks later, for repetitive vomiting and diarrhea after ingestion of oatmeal. Symptoms had largely resolved by arrival. He was afebrile, tachycardic with normal capillary refill and normal respiratory rate. After 3 hours of observation in the ED, the patient was tolerating oral rehydration solution and was able to be discharged home.
The patient was brought to the ED for a fourth time, 8 weeks later, after having been fed a banana by a sibling. He was afebrile, tachycardic, lethargic, and vomiting profusely. After 6 hours of IV rehydration and observation, the patient’s activity level normalized. He tolerated oral liquids and was discharged home.
DISCUSSION
FPIES was first described by Powell10–12 as a syndrome of profuse vomiting and diarrhea in infancy related to food allergy. It represents an allergic inflammation of both the small and large intestine in infants.9 It has been suggested that increased tumor necrosis factor-alpha (TNF-α) expression by activated T cells in the epithelium and lamina propria of the small intestine increases intestinal permeability, which contributes to pathogenesis of FPIES.12 Chung et al13 also found that in addition to increased TNF-α, infants with FPIES also have decreased expression of transforming growth factor β1 (TGF-β1) receptor. TGF-β is known to protect the epithelial barrier by stimulating the synthesis of extracellular matrix, proteins, collagen, and fibronectin.13 Increased expression of TGF-β1 is seen in older children after weaning.13 This may partially explain why FPIES is only seen in young children; however, the precise pathogenesis of FPIES is still not known.
The increased intestinal permeability in FPIES causes profuse vomiting, diarrhea, and dehydration leading to hypotension and acidosis. Thrombocytosis has a reported frequency as high as 63% of those who have blood testing resulted.7 Decreased catylase activity during periods of acute intestinal inflammation leads to increased intestinal nitrites causing increased heme oxidation and methemoglobinemia.6 This response is transient and recovers without intervention with resolution of the acute inflammation.8,9
If performed, duodenal biopsies may reveal crypt abscesses as well as villous atrophy with increased tissue staining for TNF-α, and jejunal biopsies reveal flattened villi, edema, and increased numbers of lymphocytes, eosinophils, as well as mast cell infiltration.3,9 Stool studies typically have occult blood and leukocytes, with a predominance of neutrophils and eosinophils.9
FPIES is a clinical diagnosis and endoscopy is rarely performed. This child had already had rice, oatmeal, and pears introduced to his diet without difficulty before his first ED visit. The relevance of the particular foods ingested that initiated his response is unknown. However, oral food challenge with 0.3–0.6 gm/kg of the suspected allergen with reproduction of symptoms and an increase of absolute neutrophil count by at least 3,500 cells/mm in the peripheral blood confirms the diagnosis.8
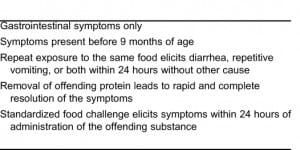
Although the clinical picture of sepsis makes FPIES a diagnostic challenge, the ED physician can arrive at this diagnosis more quickly by obtaining a dietary history as part of the evaluation, particularly in the face of previous negative sepsis workups with invasive procedures. This is especially true since fever may be present or absent. In cases where there is no fever, FPIES should be considered higher on the differential. Other considerations for the differential that may be considered on the first or second presentation might also include metabolic, toxicologic, intestinal (eg, intussusception) etiologies. Sicherer et al have proposed the diagnostic criteria for FPIES found in the Table.3,5,13
Management of acute FPIES is primarily supportive with continued fluid resuscitation. Patients require monitoring until hemodynamically stable and tolerating oral fluids. Occasionally, pressors are needed in addition to IV fluids to treat hypotension, and parenteral steroids are thought to help by diminishing the presumed T-cell mediated allergic response.6 There is no substantial evidence to suggest that antiemetics in this setting are beneficial. While steroid use is reported, no evidence-based study demonstrating clear benefit of treatment or dosing recommendations is readily apparent.3,6,7 Epinephrine is not recommended unless being used as a pressor if fluid resuscitation is unsuccessful, or for a known concurrent IgE mediated allergy.6,7
Long-term management of FPIES consists of identifying the causal protein and cross-reacting proteins and removing them from the child’s diet. Parents are urged to consult with an allergist and a pediatric dietician, but in general, breastfeeding and extensively hydrolyzed casein formulas are well tolerated.3 FPIES can be avoided by cautious introduction of solid foods and specific avoidance of grains as first foods.6 The prognosis for FPIES is good: the majority of children will outgrow their food-protein intolerance by the age of 3 with no long-term sequelae.2,5,7
CONCLUSION
FPIES is an important diagnosis to consider for the emergency physician in the infant presenting with profuse vomiting and diarrhea, particularly during time periods when parents are introducing new foods into the child’s diet. Early recognition may spare the young child the burden of recurrent hospitalizations and unnecessary and painful diagnostic testing as well as prevent the development of failure to thrive in these patients.
Footnotes
Supervising Section Editor: Paul Walsh, MB, BCh, BAO, MSc
Submission history: Submitted November 14, 2010; Revision received February 15, 2011; Accepted February 16, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.2.2134
Address for Correspondence: Marna Rayl Greenberg, DO, MPH
Lehigh Valley Hospital and Health Network, Department of Emergency Medicine, 1909 Earls Ct, Allentown, PA 18103
E-mail: mrgdo@ptd.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Schneider Chafen JJ, Newberry SJ, Riedl MA, et al. Diagnosing and managing common food allergies: A systematic review. JAMA. 2010;;303:1848–1856. [PubMed]
2. Sampson HA, Burks AW. Adverse reactions to foods. In: Adkinson NF, Middleton E, editors.Middleton’s Allergy: Principles and Practice. 7th ed. New York, NY: Mosby Elsevier; 2008. pp. 1139–1167.
3. Van der Poel LA, Fox A, du Toit G. Food protein-induced enterocolitis syndrome (FPIES): a review. Curr Allergy and Clin Immunol. 2009;;22:56–57.
4. Nowak-Wegrzyn A, Sampson HA, Wood RA, et al. Food protein-induced enterocolitis syndrome caused by solid food proteins. Pediatrics. 2003;;111:829–835. [PubMed]
5. Levy Y, Danon YL. Food protein-induced enterocolitis syndrome—not only due to cow’s milk and soy. Pediatr Allergy Immunol. 2003;;14:325–329. [PubMed]
6. Sicherer SH. Food protein-induced enterocolitis syndrome: case presentations and management lessons. J Allergy Clin Immunol. 2005. pp. 149–156. [PubMed]
7. Mehr S, Kakakios A, Frith K, Kemp AS. Food protein-induced enterocolitis syndrome: 16-year experience. Pediatrics. 2009;;123:e459–e464. [PubMed]
8. Sampson HA. Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 8th ed. Philadelphia, PA: Saunders Elsevier;; 2006. Food allergies; pp. 427–439.
9. Talley NJ. Gut eosinophilia in food allergy and systemic and autoimmune diseases. Gastroenterol Clin N Am. 2008;;37:307–332.
10. Powell GK. Milk- and soy-induced enterocolitis of infancy. J Pediatr. 1978;;93:553–560.[PubMed]
11. Powell GK. Food protein-induced enterocolitis of infancy: differential diagnosis and management.Compr Ther. 1986;;12:28–37. [PubMed]
12. Powell GK. Enterocolitis in low-birth-weight infants associated with milk and soy protein intolerance. J Pediatr. 1976;;88:840–844. [PubMed]
13. Chung HL, Hwang JB, Park JJ, et al. Expression of transforming growth factor β1, transforming growth factor type I and II receptors, and TNF-α in the mucosa of the small intestine in infants with food protein-induced enterocolitis syndrome. J Allergy Clin Immunol. 2002;;109:150–154.[PubMed]


