| Author | Affiliation |
|---|---|
| Robert Bramante, MD | North Shore University Hospital, Department of Emergency Medicine, Manhasset, New York |
| Marek Radomski, DO | North Shore University Hospital, Department of Emergency Medicine, Manhasset, New York |
| Mathew Nelson, DO | North Shore University Hospital, Department of Emergency Medicine, Manhasset, New York |
| Christopher Raio, MD | North Shore University Hospital, Department of Emergency Medicine, Manhasset, New York |
Introduction
Discussion
Conclusion
Video
ABSTRACT
Lower abdominal pain in females of reproductive age continues to be a diagnostic dilemma for the emergency physician (EP). Point-of-care ultrasound (US) allows for rapid, accurate, and safe evaluation of abdominal and pelvic pain in both the pregnant and non-pregnant patient. We present 3 cases of females presenting with right lower quadrant and adnexal tenderness where transvaginal ultrasonography revealed acute appendicitis. The discussion focuses on the use of EP- performed transvaginal US in gynecologic and intra-abdominal pathology and discusses the use of a staged approach to evaluation using US and computed tomography, as indicated.
INTRODUCTION
Acute abdominal pain in female patients of reproductive age continues to present a diagnostic challenge for the emergency physician (EP). Abdominal pain accounts for 10% of all emergency department (ED) visits, and the abdominal and pelvic examinations are notoriously unreliable for differentiating between gynecologic and intraabdominal pathology.1–3 Multiple advanced imaging and diagnostic options may be used to evaluate medical, surgical, or gynecologic pathology. Point-of-care ultrasound (US) allows for the rapid, accurate and safe differentiation of multiple diagnoses in the ED.4–6 We present 3 cases of acute appendicitis diagnosed by EP point-of-care transvaginal ultrasonography.
Case 1
The first case involved a 20-year-old female who presented with 2 hours of sudden onset right-sided abdominal pain radiating to her groin. She had been undergoing treatment for a urinary tract infection with trimethoprim/ sulfmethaxazole. The patient exhibited no nausea, vomiting, diarrhea, vaginal discharge or vaginal bleeding. Vital signs were within normal limits without fever. The abdominal examination revealed focal right lower quadrant abdominal tenderness without rebound, guarding or masses. Adnexal tenderness on the right was also noted, and there were no genital lesions, masses, vaginal discharge or cervical motion tenderness. The urine pregnancy test was negative. Laboratory evaluation was significant for a leukocytosis (white blood cell count=15.5 K/uL). A complete metabolic panel and urinalysis were within normal limits.
Initially, testing with point-of-care US was pursued to evaluate for appendicitis or gynecologic causes of pain. Using a high frequency linear array transducer (L8-3 linear array, Zonare Medical Systems Inc., Mountain View, CA, USA) transabdominal US was performed first. However, the appendix was not visualized. Next, a transvaginal US was performed using an E9-4 endocavitary probe (Zonare Medical Systems Inc., Mountain View, California). Findings included a left ovarian complex follicular cyst, small to moderate amount of free fluid, and ovaries with normal arterial and venous blood flow. Additionally, a tender, blind-ended, non-compressible, non-peristalsing, tubular structure measuring 7 mm was noted in the right adnexa consistent with acute appendicitis. A surgical consultation was called and the patient was admitted to the surgical service. The patient underwent laparoscopic resection and pathology confirmed the diagnosis of acute appendicitis.
Case 2
The second patient was a 20-year-old female complaining of right lower quadrant and suprapubic abdominal pain and nausea for 1 day. The patient denied fever, vomiting, diarrhea, vaginal bleeding or vaginal discharge. Past medical history was significant for renal colic 1 year prior. Vital signs were again within normal limits without fever. The physical examination demonstrated a soft abdomen with right lower quadrant tenderness and rebound. No cervical motion or adnexal tenderness, masses, or discharge were noted on gynecologic examination. Laboratory evaluation was remarkable only for a leukocytosis of 18.2 K/uL. Urine pregnancy testing, complete metabolic panel and urinalysis were negative.
Transabdominal US was performed without visualization of the appendix. Transvaginal US was then performed by the EP, revealing a 3.8 cm right ovarian complex cystic structure. Bilateral ovarian stroma demonstrated normal echotexture with no signs of torsion. In the right adnexa, a 7 mm blind- ended, non-peristalsing, non-compressible, tubular structure with wall edema and surrounding free fluid was identified consistent with acute appendicitis (Figure 1). The patient was admitted to the surgical service for appendectomy. Laparoscopic resection was performed and pathology confirmed the diagnosis.
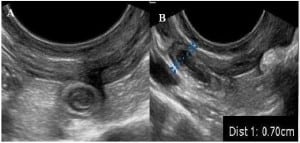
Transvaginal imaging of the right adnexa. (A) Transverse view of the appendix. (B) Long view of the appendix measuring 0.7 cm.
Case 3
The third case was an 18-year-old female with lower abdominal and pelvic pain for 1 week starting during her menstruation. She was afebrile with normal vital signs. Examination elicited right lower quadrant tenderness with guarding and no masses. Gynecologic examination demonstrated right adnexal tenderness without cervical motion tenderness, masses, lesions or discharge. Laboratory analysis was only pertinent for a leukocytosis of 12.1 K/uL.
A point-of-care endovaginal US was performed to evaluate for gynecologic pathology. A large amount of free fluid was present. Upon scanning the right adnexa an irregular tubular structure, containing an appendicolith, with surrounding hyperemia was seen (Figure 2). There was exquisite tenderness over this non-compressible structure, which measured 2.02 cm. The appendix was not visualized with transabdominal imaging. The patient was admitted to the surgical service and the diagnosis of perforated appendicitis was confirmed.

DISCUSSION
The evaluation of lower abdominal pain in the female patient presents a diagnostic dilemma for the EP. After excluding pregnancy and its complications from the differential diagnosis, there are still multiple intra-abdominal and gynecologic pathologic processes that must be considered. In our cases, the patients presented with right lower quadrant abdominal pain, and US allowed for the rapid, safe and accurate evaluation of emergent conditions, including appendicitis, ovarian torsion, and tubo-ovarian abscess.4–6 US was chosen as the initial imaging modality since it can be performed at the bedside rapidly. In addition, it allows for early initiation of appropriate treatment, consultation, and disposition.
Multiple gynecologic pathologies can be detected using US, including ovarian cysts, ovarian torsion, endometriosis, uterine fibroids and tubo-ovarian abscess. ED point-of-care US can evaluate for indicators of pelvic inflammatory disease and tubo-ovarian abscess.6 This presentation can be similar to appendicitis with lower abdominal pain, fever, adnexal tenderness and leukocystosis.
Ovarian torsion symptoms can also mimic acute appendicitis, with patients exhibiting lateralized lower quadrant abdominal pain with rapid onset.7 Ovarian torsion occurs more commonly on the right, which further confounds the differentiation from appendicitis.5 Multiple studies have stressed the importance of performing ultrasonograpy as the initial test of choice for patients presenting with lower abdominal and pelvic pain, as delay can lead to loss of the ovary in torsion, or unnecessary ionizing radiation exposure.6,8 A 2001 study showed that appendicitis was the most common preoperative diagnosis in patients with torsion, and torsion was considered in the initial differential in less than half of the patients in the study group.9
In each of our cases, point-of-care US was pursued first, with a plan to proceed to computed tomography (CT) if the US was normal or nondiagnostic. By custom and practice transabdominal US is attempted initially by the EP followed by transvaginal imaging if nondiagnostic. Appendicitis was diagnosed based on visualization of a blind-ended, non-compressible (using the transvaginal transducer and the free hand palpating over the lower abdomen), non-peristalsing, tubular structure measuring ≥ 6 mm in the right lower quadrant. Other associated signs of appendicitis include hyperemia, a visualized appendicolith, or free fluid around the appendix.6 Physical examination was not specific in our cases, as previously described in multiple cases of appendicitis diagnosed during evaluation for gynecologic pathology due to cervical motion or adnexal tenderness on examination.2,3
The staged approach of US for diagnosis of appendicitis followed by CT, as needed, is the path of choice. A 2010 study concluded that using a staged approach to imaging patients with suspected appendicitis, US had a negative predictive value of 97%, only 17% of patients required a CT, and the negative laparoscopy rate was 3%.8 US diagnosis avoids nephrotoxic contrast agents and ionizing radiation, which increases the lifetime risk of developing cancer.10 Using a staged approach, patients diagnosed by US alone had an acceptable 7% negative appendectomy rate and < 0.5% missed diagnosis rate, and with US followed by CT specificity was 91% and sensitivity was 99%.6 In each of our cases early point-of-care US allowed for early diagnosis, initiation of treatment and surgical consultation. The surgical service wanted confirmatory CT, which confirmed the point- of-care US diagnosis in each case. We believe this to be due to the atypical way in which the diagnosis was made, as our surgeons typically operate on ED US-diagnosed appendicitis.
The use of US to diagnose appendicitis is widely discussed in the literature. US for appendicitis has sensitivity between 75–99%, specificity between 86–100%, positive predictive value of 90%, and a negative predictive value between 95–97%.3,11–14 CT sensitivity for appendicitis is 92% and specificity is 96%.15 Transvaginal US should be considered in females of child-bearing age with right lower quadrant abdominal pain for numerous reasons. Delayed diagnosis of torsion or tubo-ovarian abscess can lead to infertility, mortality, or chronic pelvic pain. In addition, in a study in which transabdominal and transvaginal US was performed, 24% of patients had appendicitis only diagnosed by transvaginal scanning.16 ED performed endovaginal US was shown to modify clinician decision making when performed prior to or in lieu of CT imaging.17 Our cases demonstrate point-of-care US should be encouraged among practitioners as the initial modality. In suspicious cases, the appendix should be sought in addition to evaluating for other pelvic pathology as it can obviate the need for CT.
CONCLUSION
While abdominal pain in the reproductive female continues to present a diagnostic dilemma to the EP, point-of-care US contributes to the rapid and safe evaluation and disposition in these cases. US should be considered early in the evaluation, as part of a staged approach, to guide the overall management pathway or clinch the diagnosis. Practitioners performing point-of-care US should be alert to additional findings when performing transvaginal US as the appendix may be visualized, avoiding misdiagnosis or exposure to additional radiologic studies. Further research should aim to demonstrate the true reduction in CT use and change in disposition when US is used as a primary modality in this patient subset.
Video
Transvaginal imaging of the right adnexa demonstrating a non-compressing, enlarged appendix with an appendicolith (hyperechoic with posterior shadow)
http://www.youtube.com/watch?v=yOdcmlEso-4
Footnotes
Address for Correspondence: Robert Bramante, MD, North Shore University Hospital, 300 Community Drive, Manhasset, NY 11030. Email: BramanteMD@gmail.com.
Submission history: Revision received October 28, 2012; Submitted December 10, 2012; Accepted December 12, 2012
Conflicts of Interest : By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. van Randen A, Lameris W, van Es HW, et al. A comparison of the accuracy of US and Computed Tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011;21:1535–1545.[PMC free article] [PubMed]
2. Molander P, Paavonen J, Sjoberg J, et al. Transvaginal sonography in the diagnosis of acute appendicitis. US Obstet Gynecol. 2002;20:496–501. [PubMed]
3. Haider Z, Condous G, Ahmed S, et al. Tansvaginal sonographic diagnosis of appendicitis in acute pelvic pain. J US Med. 2006;25:1243–1244. [PubMed]
4. Adhikari S, Blaivas M, Lyon M. Role of bedside transvaginal ultrasonography in the diagnosis of tubo-ovarian abscess in the emergency department. J Emerg Med. 2008;34:429–433. [PubMed]
5. Albayram F, Hamper U. Ovarian torsion and adnexal torsion: spectrum of sonographic findings with pathologic correlation. J US Med. 2001;20:1083–1089. [PubMed]
6. Ramarajan N, Krishnamoorthi R, Barth R, et al. An interdisciplinary initiative to reduce radiation exposure: evaluation of appendicitis in a pediatric emergency department with clinical assessment supported by a staged US and computed tomography pathway. Acad Emerg Med. 2009;16:1258–1265.[PubMed]
7. Villalba ML, Huynh B, So M, et al. An ovary with a twist: a case of interesting sonographic findings of ovarian torsion. J Emerg Med. 2005;29:443–446. [PubMed]
8. Toorenvliet DR, Wiersma F, Bakker RFR, et al. Routine US and limited computed tomography for the diagnosis of acute appendicitis. World J Surg. 2010;10:2278–2285. [PMC free article] [PubMed]
9. Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med. 2001;38:156–159.[PubMed]
10. Wan MJ, Krahn M, Ungar WJ, et al. Acute appendicitis in young children: cost-effectiveness of US versus CT in diagnosis- a Markov decision analytic model. Radiology. 2009;250:378–386. [PubMed]
11. Terasawa T, Blackmore CC, Bent S, et al. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141:537–546. [PubMed]
12. Pacharn P, Yin J, Linam LE, et al. Sonography in the evaluation of acute appendicitis: are negative sonographic findings good enough? J US Med. 2010;12:1749–1755. [PubMed]
13. van Randen A, Lameris W, van Es HW, et al. Profiles of US and CT imaging features with a high probability of appendicitis. Eur Rad. 2010;20:1657–1666. [PMC free article] [PubMed]
14. Chen SC, Chen KM, Wang SM, et al. Abdominal sonography screening of clinically diagnosed or suspected appendicitis before surgery. World J Surg. 1998;22:449–452. [PubMed]
15. Hlibczuk V, Dattaro JA, Jin Z, et al. Diagnostic accuracy of noncontrast computed tomography for appendicitis in adults: a systematic review. Ann Emerg Med. 2010;55:51–9e1. [PubMed]
16. Caspi B, Zbar AP, Mavor E, et al. The contribution of transvaginal US in the diagnosis of acute appendicitis: an observational study. US Obstet and Gynecol. 2003;21:273–276. [PubMed]
17. Tayal VS, Bular M, Swanson DR, et al. ED endovaginal US in nonpregnant women with right lower quadrant pain. Amer J Emerg Med. 2008;26:81–85. [PubMed]


