Brief Research Report
Treatment Protocol Assessment
Prospective Validation of Modified NEXUS Cervical Spine Injury Criteria in Low-risk Elderly Fall Patients
Westjem Read More
Emergency Department Access
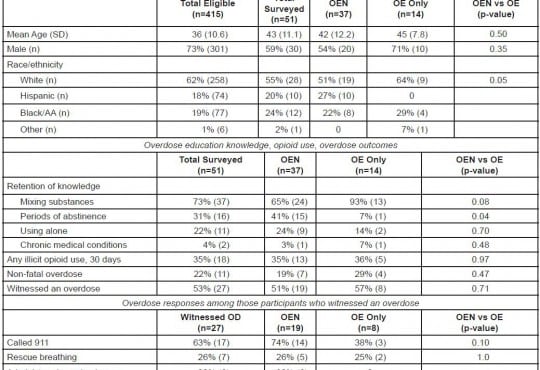
Association of Insurance Status with Severity and Management in ED Patients with Asthma Exacerbation
Westjem Read More
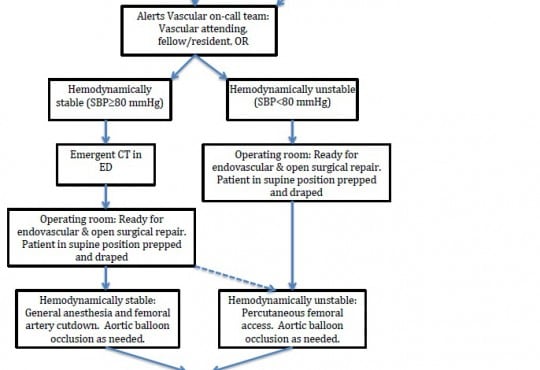
Treatment Protocol Assessment