| Author | Affiliations |
| Bryn E. Mumma, MD, MAS | University of California Davis, Department of Emergency Medicine, Sacramento, California |
| Deborah B. Diercks, MD, MSc | University of California Davis, Department of Emergency Medicine, Sacramento, California |
| James F. Holmes, MD, MPH | University of California Davis, Department of Emergency Medicine, Sacramento, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
The American Heart Association (AHA) recommends regionalized care following out-of-hospital cardiac arrest (OHCA) at cardiac resuscitation centers (CRCs). Key level 1 CRC criteria include 24/7 percutaneous coronary intervention (PCI) capability, therapeutic hypothermia capability, and annual volume of ≥40 patients resuscitated from OHCA. Our objective was to characterize the availability and utilization of resources relevant to post-cardiac arrest care, including level 1 CRCs in California.
Methods
We combined data from the AHA, the California Office of Statewide Health Planning and Development (OSHPD), and surveys to identify CRCs. We surveyed emergency department directors and nurse managers at all 24/7 PCI centers identified by the AHA to determine their post-OHCA care capabilities. The survey included questions regarding therapeutic hypothermia use and specialist availability and was pilot-tested prior to distribution. Cases of OHCA were identified in the 2011 OSHPD Patient Discharge Database using a “present on admission” diagnosis of cardiac arrest (ICD-9-CM code 427.5). We defined key level 1 CRC criteria as 24/7 PCI capability, therapeutic hypothermia, and annual volume ≥40 patients admitted with a “present on admission” diagnosis of cardiac arrest. Our primary outcome was the proportion of hospitals meeting these criteria. Descriptive statistics and 95% CI are presented.
Results
Of the 333 acute care hospitals in California, 31 (9.3%, 95% CI 6.4-13%) met level 1 CRC criteria. These hospitals treated 25% (1937/7780; 95% CI 24-26%) of all admitted OHCA patients in California in 2011. Of the 125 hospitals identified as 24/7 PCI centers by the AHA, 54 (43%, 95% CI 34-52%) admitted ≥40 patients following OHCA in 2011. Seventy (56%, 95% CI 47-65%) responded to the survey; 69/70 (99%, 95% CI 92-100%) reported having a therapeutic hypothermia protocol in effect by 2011. Five percent of admitted OHCA patients (402/7780; 95% CI 4.7-5.7%) received therapeutic hypothermia and 18% (1372/7780; 95% CI 17-19%) underwent cardiac catheterization.
Conclusion
Approximately 10% of hospitals met key criteria for AHA level 1 CRCs. These hospitals treated one-quarter of patients resuscitated from OHCA in 2011. The feasibility of regionalized care for OHCA requires detailed evaluation prior to widespread implementation. [West J Emerg Med. 2014;15(7):–758-763.]
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) occurs at a rate of 52.1 per 100,000 population and has a high mortality rate.1 Early cardiac catheterization and therapeutic hypothermia improve outcomes among post-OHCA patients,2-9 but both are currently underutilized.7,9-14 To improve access to these therapies, the American Heart Association (AHA) recommends regionalized OHCA care, including level 1 and 2 cardiac resuscitation centers (CRCs).15 Key criteria for level 1 CRCs include 24/7 percutaneous coronary intervention (PCI) capability, therapeutic hypothermia capability, and annual volume of ≥40 patients with return of spontaneous circulation following OHCA. The extent to which CRCs are available in the care of OHCA patients remains unknown. Our objective was to describe the availability and utilization of resources relevant to post-OHCA care. We hypothesized that fewer than 10% of hospitals would meet key level 1 CRC criteria and that a minority of OHCA patients would be admitted to these hospitals.
METHODS
Availability of Resources
We obtained a list of acute care hospitals in California from the Office of Statewide Health Planning and Development (OSHPD) and a list of 24/7 PCI centers in California from the AHA. We surveyed emergency department (ED) directors and nurse managers at all 24/7 PCI centers to determine their post-OHCA care capabilities. The survey included questions on therapeutic hypothermia, OHCA patient volume, and intensivist coverage (Appendix A). It was pilot-tested locally prior to distribution.We mailed surveys to ED directors at all 24/7 PCI centers in late 2011. A website link for online survey completion was provided in the cover letter. If no response was received after two mailings, we attempted to contact the medical director or nurse manager via telephone to verbally administer the survey.
Utilization of Resources
We performed a retrospective cohort study including all patients in the OSHPD Patient Discharge Database admitted during 2011, from an ED with a “present on admission” diagnosis of cardiac arrest (ICD-9-CM 427.5) or sudden death (ICD-9-CM 798). Acute care hospitals in California (excluding Veterans Affairs and military facilities) are required by law (California Health and Safety Code Section 128736) to report data for every inpatient encounter to OSHPD. These data do not represent a sample, but rather surveillance with 100% coverage. We excluded patients for whom hospital data were missing. For patients transferred from one hospital to another, the initial hospital providing care was considered the treating hospital. If the patient’s length of stay was one day or less, however, the hospital accepting the patient transfer was considered the treating hospital. Data obtained from OHSPD included patient age, gender, race, ethnicity, source of admission, source of payment, length of stay, disposition, diagnoses, “present on admission” codes, procedures, and treating hospital. Diagnoses include up to 25 conditions that existed at admission, developed during hospitalization, or affected treatment during hospitalization. Procedures include up to 21 procedures related to the patient’s stay. Diagnoses and procedures were coded according to the ICD-9-CM.16
We used the number of patients admitted to each hospital following OHCA to determine whether the hospital treated ≥40 patients resuscitated from OHCA. These data were combined with AHA data regarding 24/7 PCI status and with survey data regarding therapeutic hypothermia protocols. We merged data using hospital name and confirmed by hospital address. Key level 1 CRC criteria were defined as having 24/7 PCI capability, having a therapeutic hypothermia protocol, and admitting ≥40 patients following OHCA in 2011.15
Outcomes
The primary outcome was the proportion of hospitals meeting key level 1 CRC criteria. The secondary outcomes were the proportion of patients treated at a CRC and the proportion of patients receiving cardiac catheterization and therapeutic hypothermia.
Analysis
Data are described with descriptive statistics and 95% confidence intervals (CI) where appropriate. We performed analyses using STATA 12.0 (StataCorp LP, College Station, TX) and Google Maps (Google, Inc., Mountain View, CA). This study was deemed exempt from review by our institutional review board.
RESULTS
Availability of Resources
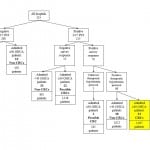
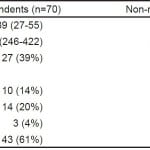
Of the 333 acute care hospitals in California, 125 were identified as 24/7 PCI centers by the AHA and were surveyed regarding their post OHCA resources (Figure 1). Seventy (56%; 95% CI 47-65%) responded to the survey; responding and non-responding hospitals were similar with regards to OHCA volume, number of licensed beds, teaching status, and trauma center status (Table).
Figure 1. Classification of hospitals.
PCI, percutaneous coronary intervention; OHCA, out-of hospital cardiac arrest; CRC, cardiac resuscitation center
Table. Characteristics of responding vs. non-responding hospitals.
OHCA, out-of hospital cardiac arrest
*Data presented as median (interquartile range).
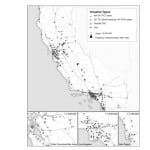
Nearly all (69/70; 99%, 95% CI 92-100%) reported having a therapeutic hypothermia protocol by 2011 (Figure 1). The remaining respondent noted that a protocol was being developed but was unsure whether it had been implemented. Per data from OSHPD, 54/125 (43%, 95% CI 34-52%) 24/7 PCI centers admitted ≥40 patients following OHCA in 2011. Overall, 31 hospitals (9.3%, 95% CI 6.4-13%) met key level 1 CRC criteria. An additional 23 (6.9%, 95% CI 4.4-10%) 24/7 PCI centers admitted ≥40 OHCA patients but did not respond to the survey regarding their therapeutic hypothermia protocol. The geographic distribution of cardiac resuscitation centers is shown in Figure 2.
Figure 2. Geographic distribution of cardiac resuscitation centers.
PCI, percutaneous coronary intervention; OHCA; out of hospital cardiac arrest; CRC, cardiac resuscitation centers; NAD, North American Datum
Half (34/68; 95% CI 38-62%) of the responding hospitals indicated that their protocol applied to patients with all arrest rhythms, and 40% (27/68; 95% CI 28-52%) reported that their protocol applied only to patients with ventricular tachycardia or ventricular fibrillation. Thirty-three hospitals (47%, 95% CI 35-59%) reported having 24/7 in-hospital intensivist staffing in their intensive care unit, 27 (39%, 95% CI 27-51%) reported intensivist staffing with limited in-hospital hours, and 10 (14%, 95% CI 7.1-25%) reported no intensivist staffing. Consistent with data from the AHA, all but one of the survey respondents reported that their hospitals had 24/7 interventional cardiac catheterization lab facilities (99%, 95% CI 92-100%).
Utilization of Resources
We identified 7,948 patients admitted to an acute care hospital in California with a “present on admission” diagnosis of cardiac arrest or sudden death. After excluding 168 patients for whom admitting hospital data were unavailable, we analyzed 7,780 patients. Median age was 66 years (interquartile range 55-79 years), and 4,493 (58%) were male. Ventricular rhythms were reported in 2,140 (28%). One quarter (1,937; 95% CI 24-26%) were treated at level 1 CRCs, and an additional 18% (1,423; 95% CI 17-19%) were treated at 24/7 PCI centers that admitted ≥40 patients resuscitated from OHCA (Figure 1). Only 129 patients were transferred from one acute care hospital to another, and the majority (105; 81%, 95% CI 74-88%) of these were not transferred to a level 1 CRC. Three quarters (95/129; 74%, 95% CI 65-81%) of transferred patients had managed care insurance, compared to 39% (3003/7780; 95% CI 38-40%) of all admitted OHCA patients.
Overall, 18% (1,372; 95% CI 17-19%) underwent cardiac catheterization, with two-thirds (912; 95% CI 64-69%) of these patients undergoing the procedure on the day of admission. Only 5% (402/7780; 95% CI 4.7-5.7%) of patients were reported to have received therapeutic hypothermia, and half of these had a ventricular rhythm (208/404; 51%, 95% CI 46-56%). Among the 47 hospitals with a therapeutic hypothermia protocol in 2010, only two (4.3%, 95% CI 0.5-15%) reported applying it to more than 20 patients in 2010. The majority indicated that it was used in five or fewer patients (15/47; 32%; 95% CI 19-47%) or were uncertain how often it was used (15/47; 32%, 95% CI 19-47%).
DISCUSSION
We identified 31 hospitals meeting key criteria for level 1 CRCs. Our survey data indicate that nearly all 24/7 PCI centers in California had a therapeutic hypothermia protocol established by 2011. This suggests that the 22 24/7 PCI centers admitting ≥40 resuscitated patients but not returning the survey also met key level 1 CRC criteria. Thus, approximately 15% of acute care hospitals in California meet key AHA criteria for level 1 CRCs and admit 43% of patients resuscitated from OHCA.
An important feature of systems of care in OHCA is early transfer of patients to level 1 CRCs.15 In our data, very few resuscitated patients were transferred to a level 1 CRC or to a 24/7 PCI center admitting ≥40 resuscitated OHCA patients. Insurance plan appeared to influence transfer practices, with transferred patients having a substantially higher rate of managed care coverage. Our data suggest that regionalized care between level 2 and level 1 CRCs is poorly developed and an area for future improvement. The geographic distribution of these hospitals with respect to the population requires evaluation to determine the feasibility of regionalized care for patients resuscitated from OHCA, particularly in rural areas. In addition, policy makers and hospital administrators need to determine the need for these centers to maximize availability of limited resources.
Similar to previous studies, both cardiac catheterization and therapeutic hypothermia were widely available but infrequently used in the study patient population.13,14,17 This finding is concerning as evidence suggests both these interventions improve patient outcomes. Prior studies suggest that lack of an organized protocol is a significant barrier to using therapeutic hypothermia,17 but this seems unlikely to be the reason for low utilization in our population given the widespread availability of therapeutic hypothermia protocols. Limited awareness of or agreement with the evidence supporting these recommendations and perception of poor patient prognosis may have contributed to low utilization.17,18 Additionally, concerns regarding cardiac catheterization outcome reporting may dissuade physicians and hospitals from performing this procedure in post-OHCA patients.19 Future research should investigate variables associated with the failure to perform cardiac catheterization and therapeutic hypothermia in this population. Once reasons these patients are not receiving these interventions are identified, interventions to maximize these procedures can be designed.
LIMITATIONS
The survey response rate was 56%, subjecting the data to response bias. Where possible, we used data from independent sources to minimize the effect of response bias. OSHPD includes up to 21 procedures for each patient; if a patient received more than 21 procedures during hospitalization, cardiac catheterization and/or therapeutic hypothermia may not have been reported. However, the OSHPD data regarding cardiac catheterization are similar to those recently reported in a Los Angeles cohort,20 and the OSHPD data on therapeutic hypothermia utilization are consistent with our survey results. We were unable to evaluate all elements in the AHA’s recommendations for regionalized systems of care in OHCA.15 Last, our data reflect availability and utilization of resources in California and may not be generalizable to areas outside of California. Resource allocation and healthcare spending priorities may differ between California and other areas.
CONCLUSION
Approximately 10% of hospitals meeting key AHA level 1 CRC criteria treated 25% of patients resuscitated from OHCA in 2011. Cardiac catheterization and therapeutic hypothermia were used in 18% and 5% of patients, respectively. The reasons for low utilization of cardiac catheterization and therapeutic hypothermia among resuscitated OHCA patients and the feasibility of regionalized care for these patients require detailed evaluation prior to widespread implementation.
Footnotes
Supervising Section Editor: Jeremy Hess, MD, MPH
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Bryn E. Mumma, MD, MAS, University of California, Davis, Department of Emergency Medicine, 4150 V Street, PSSB #2100, Sacramento, CA 95817. Email: mummabe@gmail.com.
Submission history: Submitted March 27, 2014; Revision received July 18, 2014; Accepted August 20, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant #UL1 TR000002. The first author is supported by the National Heart, Lung, and Blood (NHLBI) Research Career Development Programs in Emergency Medicine through grant #5K12HL108964-03 and the ZOLL-National Association of EMS Physicians EMS Resuscitation Research Fellowship.
REFERENCES
- Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423-31.
- Rittenberger JC, Guyette FX, Tisherman SA, et al. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79:198-204.
- Sunde K, Pytte M, Jacobsen D, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29-39.
- Gaieski DF, Band RA, Abella BS, et al. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009;80:418-24.
- Knafelj R, Radsel P, Ploj T, et al. Primary percutaneous coronary intervention and mild induced hypothermia in comatose survivors of ventricular fibrillation with ST-elevation acute myocardial infarction. Resuscitation. 2007;74:227-34.
- Wolfrum S, Pierau C, Radke PW, et al. Mild therapeutic hypothermia in patients after out-of-hospital cardiac arrest due to acute ST-segment elevation myocardial infarction undergoing immediate percutaneous coronary intervention. Crit Care Med. 2008;36:1780-6.
- Kern KB, Rahman O. Emergent percutaneous coronary intervention for resuscitated victims of out-of-hospital cardiac arrest. Catheter Cardiovasc Interv. 2010;75:616-24.
- Stub D, Hengel C, Chan W, et al. Usefulness of cooling and coronary catheterization to improve survival in out-of-hospital cardiac arrest. Am J Cardiol. 2011;107:522-7.
- Callaway CW, Schmicker RH, Brown SP, et al. Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out-of-hospital cardiac arrest. Resuscitation. 2014.
- Reynolds JC, Callaway CW, El Khoudary et al. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. J Intensive Care Med. 2009;24:179-86.
- Lettieri C, Savonitto S, De Servi S, et al. Emergency percutaneous coronary intervention in patients with ST-elevation myocardial infarction complicated by out-of-hospital cardiac arrest: early and medium-term outcome. Am Heart J. 2009;157:569-75 e1.
- Keelan PC, Bunch TJ, White RD, et al. Early direct coronary angioplasty in survivors of out-of-hospital cardiac arrest. Am J Cardiol. 2003;91:1461-3,A6.
- Abella BS, Rhee JW, Huang KN, et al. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation. 2005;64:181-6.
- Merchant RM, Soar J, Skrifvars MB, et al. Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit Care Med. 2006;34:1935-40.
- Nichol G, Aufderheide TP, Eigel B, et al. Regional systems of care for out-of-hospital cardiac arrest: A policy statement from the American Heart Association. Circulation. 2010;121:709-29.
- The International Classification of Diseases, 9th Revision, Clinical Modification. National Center for Health Statistics. Accessed January 14, 2014.
- Bigham BL, Dainty KN, Scales DC, Morrison LJ, Brooks SC. Predictors of adopting therapeutic hypothermia for post-cardiac arrest patients among Canadian emergency and critical care physicians. Resuscitation. 2010;81:20-4.
- Toma A, Bensimon CM, Dainty KN, et al. Perceived barriers to therapeutic hypothermia for patients resuscitated from cardiac arrest: a qualitative study of emergency department and critical care workers. Crit Care Med. 2010;38:504-9.
- Peberdy MA, Donnino MW, Callaway CW, et al. Impact of percutaneous coronary intervention performance reporting on cardiac resuscitation centers: a scientific statement from the American Heart Association. Circulation. 2013;128:762-73.
- Bosson N, Kaji AH, Niemann JT, et al. Survival and Neurologic Outcome after Out-of-Hospital Cardiac Arrest: Results One Year after Regionalization of Post-Cardiac Arrest Care in a Large Metropolitan Area. Prehosp Emerg Care. 2014.