| Author | Affiliation |
|---|---|
| Margaret K. Sande, MD, MS | Denver Health & Hospital Authority, Denver, Colorado
University of Colorado, Aurora, Colorado |
| Kerry B. Broderick, MD | Denver Health & Hospital Authority, Denver, Colorado
University of Colorado, Aurora, Colorado |
| Maria E. Moreira, MD | Denver Health & Hospital Authority, Denver, Colorado
University of Colorado, Aurora, Colorado |
| Brooke Bender, MPH | Denver Health & Hospital Authority, Denver, Colorado |
| Emily Hopkins, MSPH | Denver Health & Hospital Authority, Denver, Colorado |
| Jennie A. Buchanan, MD | Denver Health & Hospital Authority, Denver, Colorado
University of Colorado, Aurora, Colorado |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Abstract
Introduction:
There is currently no standard forensic medicine training program for emergency medicine residents. In the advent of sexual assault nurse examiner (SANE) programs aimed at improving the quality of care for sexual assault victims, it is also unclear how these programs impact emergency medicine (EM) resident forensic medicine training. The purpose of this study was to gather information on EM residency programs’ training in the care of sexual assault patients and determine what impact SANE programs may have on the experience of EM resident training from the perspective of residency program directors (PDs).
Methods:
This was a cross-sectional survey. The study cohort was all residency PDs from approved EM residency training programs who completed a closed-response self-administered survey electronically.
Results:
We sent surveys to 152 PDs, and 71 responded for an overall response rate of 47%. Twenty-two PDs (31%) reported that their residency does not require procedural competency for the sexual assault exam, and 29 (41%) reported their residents are required only to observe sexual assault exam completion to demonstrate competency. Residency PDs were asked how their programs established resident requirements for sexual assault exams. Thirty-seven PDs (52%) did not know how their sexual assault exam requirement was established.
Conclusion:
More than half of residency PDs did not know how their sexual assault guidelines were established, and few were based upon recommendations from the literature. There is no clear consensus as to how PDs view the effect of SANE programs on resident competency with the sexual assault exam. This study highlights both a need for increased awareness of EM resident sexual assault education nationally and also a possible need for a training curriculum defining guidelines for EM residents performing sexual assault exams.
INTRODUCTION
In 2009 more than 125,000 sexual assaults were reported in the United States (U.S.).1 Emergency physicians (EP) work closely with law enforcement as victims often present to emergency departments (ED) for evaluation, and physician documentation and testimony in sexual assault cases is valuable for the prosecution of offenders. Studies show that accurate and thorough documentation of injuries correlates with higher rates of charges filed and successful conviction of perpetrators.2,3
The American Board of Emergency Medicine’s Model of Clinical Practice of Emergency Medicine includes sexual assault patient assessment and the completion of the sexual assault examination as integral topics and skills, but there are no recommendations regarding the number of hours or content dedicated to resident training in assessment of sexually assaulted patients.4 While EPs remain the initial primary providers treating victims of violent crimes, many are not properly trained to care for sexual assault patients. Guidelines providing educational direction for emergency medicine (EM) residency forensic training and sexual assault training are sparse.5
Over the last 35 years, sexual assault nurse examiner (SANE) programs, sometimes referred to as sexual assault forensic examiner programs (SAFE) or sexual assault response teams (SART) have improved the quality of care for sexual assault victims. (We collectively refer to these programsas SANE programs for simplicity).3,6 There are now over 600 SANE programs in the U.S. and associated territories; these programs are quickly becoming the model of care for assault victims.3,7 While the creation of SANE programs has improved patient care, it is unclear how these programs impact EM resident training at academic institutions.
The purpose of this study is two-fold: to gather information from the program directors (PDs) of U.S. EM residency programs’ regarding the current training of EM residents in the care of sexual assault patients, and to survey what PDs think has been the overall impact of SANE programs on EM resident training.
METHODS
This is a cross-sectional survey of current program directors of U.S. EM residency training programs. The survey was available over a 3-month period from June 16 to September 16, 2010. No identifiable information was requested in the survey; responses were submitted electronically, anonymously, and voluntarily. Approval for this study was obtained from the Colorado Multiple Institutional Review Board; no informed consent was required.
We generated a list of current PDs from the 152 approved EM residency training programs from the Society of Academic Emergency Medicine residency catalog. A survey was developed by consensus of the authors of this paper and piloted to non-PDs for comment. We then circulated electronically a final survey consisting of 15 questions via Zoomerang (MarketTools Company, San Francisco, CA). The survey is included as the Figure.

Survey distributed to program directors and associated responses.
We conducted participant recruitment via an electronic invitation that described the intent of the project. Various Dillman techniques, including the use of a shorter questionnaire, regular follow-up via email, and university sponsorship were used to strengthen the response rate.8
We aggregated data into an Excel database (Microsoft Corporation, Redmond, WA) that was then transferred into SAS or Stata formats using translational software (dfPower/DBMS Copy, DataFlux Corporation, Cary, NC). We performed all statistical analyses using SAS Version 9.2 (SAS Institute, Inc., Cary, NC) or Stata Version 10 (Stata Corporation, College Station, TX). Descriptive statistics for continuous variables were expressed as medians with interquartile ranges and proportions as percentages with 95% confidence intervals (CIs).
RESULTS
Of the 152 EM programs asked to complete the survey, 62 PDs completed the survey in its entirety, and 9 completed a portion of the survey for a total of 71 respondents (47%). The primary investigator reviewed the survey results, and answers to questions by partial responders were manually added into the overall data set.
Among the 71 who responded, the majority (79%) have a SANE program at their institution and a majority (61%) note that their residents work in hospitals offering 24-hour SANE coverage. Descriptive statistics of those responding to the survey are included in Table 1. Descriptive data about the implementation of SANE programs at institutions with residency programs are included in the Figure (questions 9,12, and 13).
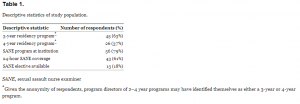
Descriptive statistics of study population.
When PDs were asked about their residency programs’ requirements in sexual assault education, the majority of responding PDs (41%) reported their residents are required only to observe sexual assault exam completion. Of those reporting required demonstration of exam performance, most PDs (38%) note their residents are required to perform 5 or fewer sexual assault exams to achieve procedural competency. Additional findings regarding required competency in sexual assault exam completion are included in Table 2. With regard to didactics, the majority of PDs (69%) report their residents receive 1–5 hours of sexual assault education (Figure questions 6–7).
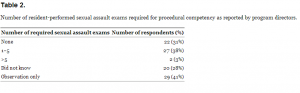
Number of resident-performed sexual assault exams required for procedural competency as reported by program directors.
After defining how many sexual assault exams are required of residents for demonstration of competency, PDs were asked how such requirements were established (Table 3). One PD (1%) cited a literature-based recommendation, while the majority of PDs (52%) did not know how their sexual assault exam requirements were established. The remaining respondents cited various other methods, such as consensus decision, or reported that their residency program did not have a set requirement.
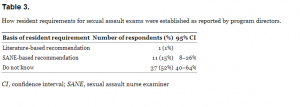
How resident requirements for sexual assault exams were established as reported by program directors.
Among institutions reporting the availability of SANE programs, PD opinions differed as to whether SANE is felt to have helped or hindered resident education. Of the 56 PDs responding to the question, the majority (45%) felt SANE programs have had no effect on resident sexual assault examination education. Additional findings and associated confidence intervals are presented in Table 4. PDs were asked to further explain their responses to this question, and themes generated from those responses are summarized in Table 5.
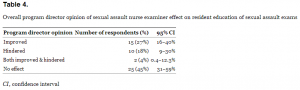
Overall program director opinion of sexual assault nurse examiner effect on resident education of sexual assault exams
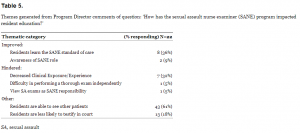
Themes generated from Program Director comments of question: ‘How has the sexual assault nurse examiner (SANE) program impacted resident education?’
DISCUSSION
To our knowledge, this is the first survey addressing sexual assault education across U.S. EM training programs. This study highlights the current state of sexual assault education across EM residencies, associated PD attitudes and attention paid to this area of resident education, and the possible effect of SANE programs on resident training and education.
There is significant variation in sexual assault training across EM residency programs. In our study, 31% of PDs report their EM residency programs do not require procedural competency in the SANE exam, 41% require observation alone, and 38% of programs require fewer than 5 exams. Only 2 programs (3%) reported requiring more than 5 sexual assault exams. This is in stark contrast to the training of SANE providers, who must perform a median of 80 hours of mandated clinical and didactic training to obtain procedural competency.9 This study highlights the dichotomy in expectations between SANE versus resident competency and is noteworthy given that both groups care for the same patient population. Literature evaluating EM residents’ skills in sexual assault exams does support that improvements in sexual assault examination skills can be made by providing tailored SANE-based training, as was done at the University of New Mexico, where a curriculum that included didactics, role play, and skills training was implemented. A study of this program found that resident skills can be on par with that of SANE providers.10 Broader national support for a training program such as this is worth future consideration.
Second, there are equally varying degrees of awareness paid by EM residency PDs to this component of their residents’ overall education, despite the EM Model of Clinical Practice curriculum’s inclusion of sexual assault education. More than a quarter (28%) of responding PDs did not know how many resident-performed sexual assault exams are required for demonstration of procedural competency, and more than half of PDs had no insight regarding how their sexual assault guidelines were established. The overall response rate (47%) of this study may also be indicative of decreased attention paid to sexual assault education, though this can only be postulated. While in this study the majority of responding PDs reported they work at institutions with SANE programs (79%), given many physicians will ultimately practice in settings where there is no SANE program, it remains an important component of EM residency training.
Lastly, this study highlights that there is no clear consensus regarding how PDs feel SANE programs have affected resident education in sexual assault. The most commonly held opinion among PD respondents in this study was that SANE programs do not impact residency training, while 27% believed that resident training is improved, and 18% believed training is negatively impacted. There is a paucity of literature regarding the impact of SANE programs on resident competency in treating and examining a sexual assault patient. While SANE programs have been shown to enhance patient care and accuracy of evidence collection, there remains the possibility that the availability of a SANE program may decreases resident exposure to these patients and in turn affects their competency and comfort with the sexual assault exam due to limited exposure.3,6 Resident training with a SANE nurse can be an excellent opportunity to learn how to proficiently perform exams. However, competency in all procedural components is likely not obtained solely by observation, but also by performing the complete exam and evidentiary collection. If SANE programs continue to thrive, it is possible the EM model of clinical practice may evolve and there may be a shift away from sexual assault examination education for resident physicians. However, many SANE programs have physician advisors; arguably it is important that they be competent in the forensic evaluation of the sexually assaulted patient. Many likely rely on training from residency or an interest in the care of this patient population. In the future EM might consider adopting the Australian curriculum of formal forensic fellowships after EM training as specialty training.11
LIMITATIONS
The main limitations of this study are a result of its design as an electronic survey. The response rate was 47%, which is comparable to other web-based surveys, as one review paper reported a mean response rate of 36.8% for email surveys.12 Our study was subject to response bias given that 79% of respondents have a SANE program at their institution. While we do not know the actual percent of EM residency programs with SANE programs, this is likely biased toward recruitment of PDs who have a SANE program at their institution. The study is inherently limited, given that data is self-reported and sexual assault residency requirements or the basis for them may vary from what is reported. Because of anonymity we were unable to characterize responders versus non-responders.
CONCLUSION
In gathering information from U.S. EM residency PDs, we conclude there is no national consensus as to how an EM resident physician are educated in sexual assault examination and that there are varied attitudes and attention paid to this area of resident education.
Second, there is lack of consensus as to the effect of SANE programs on EM resident education in sexual assault exams. Given the overall success of SANE programs to date, it is anticipated that SANE programs will continue to coexist at residency training sites. In order to better elucidate the effect of SANE programs on resident training, future work should be targeted to residents at programs with SANE versus those without, and if possible target residents at programs before and after the implementation of SANE programs. Projects such as these would more directly assess impact of SANE on resident preparedness in this area of their training.
These results should spur conversation within residency leadership about the status of their own sexual assault educational initiatives, and perhaps serve as the catalyst for groups with interest in this area to convene and assess the need for a national training model in sexual assault education.
Footnotes
Address for Correspondence: Margaret K. Sande, MD, MS. University of Colorado Department of Emergency Medicine, 12401 East 17th Ave., Box B215, Aurora, CO 80045. Email: mksande@gmail.com.
Submission history: Revision received March 25, 2012; Submitted February 13, 2013; Accepted February 15, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Truman JL, Rand M Bureau of Justice statistics bulletin: national crime victimization survey. criminal victimization, 2009. . ;
2 McGregor MJ, Du Mont J, Myhr TL Sexual assault forensic medical examination: is evidence related to successful prosecution?. Ann Emerg Med. 2002; 39:639-47
3 Campbell R, Patterson D, Lichty LF The effectiveness of sexual assault nurse examiner (SANE) programs: a review of psychological, medical, legal and community outcomes. Trauma Violence Abuse. 2005; 6:313-29
4 2011. Model of the Clinical Practice of Emergency Medicine. Available at:https://www.abem.org/PUBLIC/_Rainbow/Documents/2011%20EM%20Model%20-%20Website%20Document.pdf. Accessed February 1, 2013.
5 Wiler JL, Bailey H The need for emergency medicine resident training in forensic medicine. Ann Emerg Med. 2007; 50:733-738
6 Sievers V, Murphy S, Miller JJ Sexual assault evidence collection more accurate when completed by sexual assault nurse examiners: Colorado’s experience. J Emerg Nurs. 2003; 29:511-14
7 Sexual Assault Nurse Examiner, Sexual Assault Response Team SANE Program Locator. Available at:http://www.sane-sart.com/staticpages/index.php?page=20031023141144274. Accessed February 1, 2013.
8 Dillman DA . Mail and internet surveys: the tailored design method. 2007;
9 Ciancone AC, Wilson C, Collette R, Gerson LW Sexual Assault Nurse Examiner programs in the United States. Ann Emerg Med. 2000; 35:353-7
10 McLaughlin SA, Monahan C, Doezema D Implementation and evaluation of a training program for the management of sexual assault in the emergency department. Ann Emerg Med. 2007; 49:489-94
11 Young S, Wells D, Summers I Specific training in clinical forensic medicine is useful to ACEM trainees. Emerg Med Australas. 2004; 16:441-5
12 Sheehan KB E-mail survey response rates: a review. J Comput Mediat Commun. 2001; 6:0


