| Author | Affiliation |
|---|---|
| Patrick M. Lank, MD | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
| Elizabeth Pines, MD | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
| Mark B. Mycyk, MD | Northwestern University Feinberg School of Medicine, Department of Emergency Medicine, Chicago, Illinois |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Abstract
Introduction:
The use of synthetic drugs of abuse in the United States has grown in the last few years, with little information available on how much physicians know about these drugs and how they are treating patients using them. The objective of this study was to assess emergency physician (EP) knowledge of synthetic cannabinoids (SC).
Methods:
A self-administered internet-based survey of resident and attending EPs at a large urban emergency department (ED) was administered to assess familiarity with the terms Spice or K2 and basic knowledge of SC, and to describe some practice patterns when managing SC intoxication in the ED.
Results:
Of the 83 physicians invited to participate, 73 (88%) completed surveys. The terms “Spice” and “K2” for SC were known to 25/73 (34%) and 36/73 (49%) of respondents. Knowledge of SC came most commonly (72%) from non-medical sources, with lay publications and the internet providing most respondents with information. Among those with previous knowledge of synthetic cannabinoids, 25% were not aware that SC are synthetic drugs, and 17% did not know they are chemically most similar to marijuana. Among all participants, 80% felt unprepared caring for a patient in the ED who had used synthetic cannabinoids.
Conclusion:
Clinically active EPs are unfamiliar with synthetic cannabinoids. Even those who stated they had heard of synthetic cannabinoids answered poorly on basic knowledge questions. More education is needed among EPs of all ages and levels of training on synthetic cannabinoids.
INTRODUCTION
In March 2011, the United States Drug Enforcement Administration (DEA) temporarily placed 5 synthetic cannabinoids (SC) into Schedule 1 of the Controlled Substances Act “to avoid imminent hazard to the public safety.”1 These SC products have received substantial media attention for being sold as “legal highs” that have names such as “Spice” and “K2” and are packaged as “incense.” Complications from SC use have resulted in increasing numbers of hospital visits.2 Currently, additional media and legislative attention is being paid to the difficulty of enforcing such a ban, since producers of SC products have a myriad of additional cannabinoid compounds to use besides the 5 restricted by the DEA.3
The initial growth of SC use in the United States (U.S.) was sparked by reports that they had effects similar to marijuana, but with the advantages that they are undetectable on routine urine drug screens and were widely legally available on the internet, in “head shops” and in gas stations. A report by the 2011 “Monitoring the Future” study quantified the popularity of SC, particularly among adolescents, with 11.4% of high school seniors admitting to having used SC within the previous 12 months.4 However, reports of such adverse effects as psychosis, seizures, myocardial infarction, dysrhythmias, and metabolic derangements, show that although these substances are cannabinoids with physiologic activity at cannabinoids receptors, their clinical effects are quite different from those caused by smoking marijuana.5–9 Researchers have voiced further concern about the potential long-term immunologic, neurologic, and psychiatric complications specifically in adolescent patients.10
It has been well described that people with drug-related complications often seek care in the emergency department (ED).11 When the use of new synthetic drugs becomes popular, emergency physicians (EPs) are in a particularly difficult position, often treating patients while having relatively little knowledge of the substance the patient has taken. Using SC as a convenient example of an emerging drug of abuse, we investigated EP knowledge of SC and potential practice patterns for managing patients presenting after ingestion of SC.
METHODS
We performed a self-administered, anonymous, voluntary, internet-based survey in December 2010 of resident and attending EPs at a large academic urban ED with an annual volume of approximately 85,000 visits. The survey was pre-tested among a group of students, was revised for study performance, and then was piloted among a small group of volunteer physicians not participating in the survey study. Given the subject of the survey, the questions were all original. The survey instrument used closed-format questions to assess familiarity with the substances Spice and K2, basic knowledge of SC, and potential practice patterns when managing intoxication with SC in the ED. Responses were categorical, binary, or on a four-point Likert scale. The local institutional review board exempted the project from review.
All statistical calculations were performed using R, version 2.14.0. All percentages are displayed with their associated confidence intervals (CI). Comparisons between groups were performed using chi-square or Fisher’s exact test where appropriate. Level of significance was P<0.05, and statistical tests were two-sided.
RESULTS
Out of 83 invited participants, 73 EPs completed the survey (88%): 47 were residents and 26 were attending physicians (Table 1). There were no differences in familiarity, knowledge, or management of SC when comparing age of the respondent, level of training (resident or attending), or years of experience. A majority of EPs had never heard of the recreational drugs Spice (48 of 73 [66%; 95% CI, 54%–76%]) or K2 (37 of 73 [51%; 95% CI, 39%–62%]). At the time of the survey, few EPs had ever discussed SC use with a patient (4 of 73 [5.5%; 95% CI, 0.3%–10.7%]), and few had taken care of a patient who used Spice or K2 (3 of 73 [4.1%; 95% CI, −0.4%–8.7%]). Of all respondents, 14% (95% CI, 7%–24%) believed SC were most commonly obtained either from a pharmacy or by physician prescription.
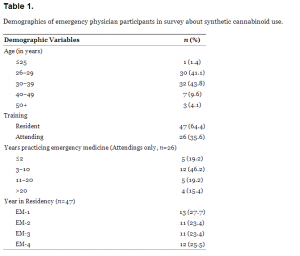
Demographics of emergency physician participants in survey about synthetic cannabinoid use.
Among physicians familiar with SC, 25% (95% CI, 13%–43%) were not aware they are synthetic drugs. While most physicians who were familiar with SC were aware SC are most similar to marijuana, 17% (95% CI, 7%–33%) believed they are more similar to gamma-hydroxybutyrate (GHB), diazepam, or cocaine. When asked about symptoms, 47% (95% CI, 31%–64%) would not expect to see anxiety, sedation, or psychosis in a patient who had used SC. Physicians obtained their information about SC from sources other than medical publications or lectures 72% of the time (95% CI, 55%–85%), citing lay publications, patients, colleagues, and the internet most commonly (Figure).
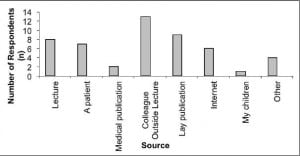
Sources of physician knowledge about synthetic cannabinoids.
Those physicians who had never heard of Spice or K2 were more likely to order additional testing, with 65% ordering urine drug screens, as opposed to 39% of those who were familiar with SC (P < 0.05). A higher proportion of physicians unfamiliar with SC were more likely to admit an SC user to the hospital (39% vs. 3%, P < 0.005). Of all participants, 80% (95% CI, 69%–88%) did not feel “prepared” caring for a patient in the ED who has used SC, and 92% (95% CI, 82%–97%) felt they need more education on such emerging drugs of abuse (Table 2).
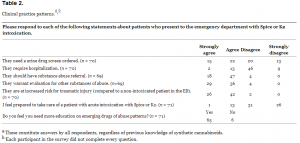
Clinical practice patterns.
DISCUSSION
This study showed unfamiliarity and inexperience with SC among EPs during a time when their use was growing in popularity. Even among those familiar with SC, there were many misconceptions about SC and their clinical effects, with most physicians obtaining their information from non-medical sources.
This study brings to light the problems physicians face when treating patients who are using new drugs of abuse. Specifically, it became clear that there is an inherent difficulty in treating patients using a new drug of abuse because of a lack of available medical literature on the substance.12 Further confounding the issue, the medical literature that is available constantly changes with reports of novel side effects and complications.
These facts also made studying physician knowledge of new drugs of abuse particularly challenging. Questions initially included in the survey, including some questions on availability and legality, had to later be excluded because of multiple changes occurring throughout the survey and data analysis period. This ever-changing aspect of “designer drug” investigation is mirrored in the clinical setting with adjustments for rapidly growing medical knowledge.
In the few hospitals with medical toxicologists on staff, it is largely accepted that one of the roles of the medical toxicologist is to educate other healthcare providers on new developments in the field of toxicology. The very large majority of hospitals without a medical toxicologist may instead rely on information provided by their regional poison center. With the seemingly limitless designer drug compounds available for use and with no information on relative toxicity of each compound, this connection to toxicologists, poison centers, or other experts in emerging drugs of abuse will be crucial to EPs dealing with the constantly changing world of designer drugs.
LIMITATIONS
This survey study is limited by having a small sample size and being performed in a single study center. Despite these limitations, this study provides useful information that may help focus the education of emergency physicians during future outbreaks of new drugs of abuse.
CONCLUSION
In the last few years, the use of synthetic drugs of abuse has grown, with little information available on healthcare provider knowledge about these drugs and how they are treating patients using them.13 This study focused on synthetic cannabinoids, showing that during this period of growth, EPs were unfamiliar with synthetic cannabinoids and felt they needed more education.
Footnotes
Address for Correspondence: Patrick M. Lank, MD, Northwestern University Feinberg School of Medicine, 211 E Ontario Street, Room 200, Chicago, IL 60611. Email: patrick.lank@gmail.com.
Submission history: Revision received August 24, 2012; Submitted November 1, 2012; Accepted January 28, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Schedules of Controlled Substances: Temporary Placement of Five Synthetic Cannabinoids Into Schedule I [FR Doc No: 11075-11078]. Drug Enforcement Administration (DEA). U.S. Department of Justice. 2011. Available at: http://www.deadiversion.usdoj.gov/fed_regs/rules/2011/fr0301.htm. Accessed August 23, 2012.
2 Forrester MB, Kleinschmidt K, Schwarz E Synthetic cannabinoid exposures reported to Texas poison centers. J Addict Dis. 2011; 30:351-358
3 Carroll FI, Lewin AH, Mascarella SW Designer drugs: a medicinal chemistry perspective. Ann N Y Acad Sci. 2012; 1248:18-38
4 Johnston LD, O’Malley PM, Bachman JG . Marijuana use continues to rise among US teens, while alcohol use hits historic lows. 2011;
5 Schneir AB, Cullen J, Ly BT “Spice” girls: synthetic cannabinoid intoxication. J Emerg Med. 2011; 40:296-269
6 Vardakou I, Pistos C, Spiliopoulou C Spice drugs as a new trend: mode of action, identification and legislation. Toxicol Lett. 2010; 197:157-162
7 Lapoint J, James LP, Moran CL Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol (Phila). 2011; 49:760-4
8 Mir A, Obafemi A, Young A Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011; 128:e1622-1627
9 Schneir AB, Baumbacher T Convulsions associated with the use of a synthetic cannabinoid product. J Med Toxicol. 2012; 8:62-64
10 Cohen J, Morrison S, Greenberg J Clinical presentation of intoxication due to synthetic cannabinoids. Pediatrics. 2012; 129:e1064-1067
11 Magill M, Barnett NP, Apodaca TR The role of marijuana use in brief motivational intervention with young adult drinkers treated in an emergency department. J Stud Alcohol Drugs. 2009; 70:409-413
12 Mycyk MB Emerging drugs of abuse: what was new yesterday is NEW today. J Med Toxicol. 2012; 8:1-2
13 Bronstein AC, Spyker DA, Cantilena LR 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila). 2011; 49:910-941


