| Author | Affiliation |
|---|---|
| Geoffrey Alexander, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
| Ryan Walsh, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
| Adam Nielsen, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
A 41-day-old girl presented to the emergency department with a new dark red mass protruding from the umbilicus noted 3.5 hours prior to presentation. The patient’s mother reported the umbilical stump fell off at 4 days of life, but the patient continued to have intermittent clear green drainage from a small mass at the base of the umbilicus. The patient was born full-term with an otherwise unremarkable medical history.
Physical exam revealed a small, moist, erythematous mass protruding from the umbilicus (Figure). The mass was removed with minimal bleeding and no pain while attempting silk ligation. The specimen was sent for pathology, which returned 3 days later with the diagnosis of umbilical granuloma.
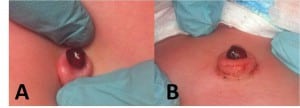
View from above (A) and from the side (B) with umbilicus retracted to demonstrate pedunculated stump of the umbilical granuloma.
An umbilical granuloma is a common benign abnormality in neonates that form from excess granulation tissue remaining at the base of the umbilicus after cord separation. It forms during the first few weeks of life and should not be present at birth. They typically are associated with persistent drainage involving the umbilicus after cord separation.1 It is a soft, round, moist, usually pink, friable, pedunculated mass, typically 3–10 mm in diameter. Umbilical polyps, urachal tract, and omphalomesenteric duct remnants must be considered.1,2
Multiple techniques are available to treat umbilical granulomas. Application of topical antibiotics, elimination of friction, air drying with alcohol wipes, and application of common table salt are conservative measures that may allow for epithelialization.3–5 Cauterization with silver nitrate is the most common treatment and generally requires multiple applications.1,6 Ligature, electrocautery, and cryosurgery are other treatment options. Further evaluation for other pathology is warranted if the lesion fails to resolve with silver nitrate and/or ligation.1,5,7
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted: August 2, 2012; Accepted August 3, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.8.13249
Address for Correspondence: Geoffrey Alexander, MD. Madigan Army Medical Center, Department of Emergency Medicine, Bldg 9040 Fitzsimmons Drive, Tacoma, WA 98431. Email: galexander703@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none. The opinions expressed in this article are those of the authors and do not reflect the official policy of the Department of the Army, Department of Defense, or the U.S. Government.
REFERENCES
1. Pomeranz A. Anomalies, abnormalities, and care of the umbilicus. Pediatr Clin North Am.2004;51:819–827. [PubMed]
2. Campbell J, Beasley SW, McMullin N, et al. Clinical diagnosis of umbilical swellings and discharges in children. Med J Aust. 1986;145:450–453. [PubMed]
3. Daniels J, Craig F, Wajed R, et al. Umbilical Granulomas: a randomised controlled trial [published correction appears in Arch Dis Child Fetal Neonatal Ed 2003;88:F446] Arch Dis Child Fetal Neonatal Ed. 2003;88:F257. [PMC free article] [PubMed]
4. Derakhshan MR. Curative effect of common salt on umbilical granuloma. Iran J Med Sci.1998;23:132–133.
5. Meltzer D. A newborn with an umbilical mass. Am Fam Physician. 2005;71:1590–1592. [PubMed]
6. Nagar H. Umbilical granuloma: a new approach to an old problem. Pediatr Surg Int. 2001;17:513–514. [PubMed]
7. Lotan G, Klin B, Efrati Y. Double-ligature: a treatment for pedunculated umbilical granulomas in children. Am Fam Physician. 2002;65:2067–2068. [PubMed]


