| Author | Affiliation |
|---|---|
| Trissy Chun, MD | Maimonides Medical Center, Department of Emergency Medicine, Brooklyn, NY |
| Eitan Dickman, MD | Maimonides Medical Center, Department of Emergency Medicine, Brooklyn, NY |
A 15-year-old Hispanic primigravid female at 12 weeks gestation presented to the Emergency Department (ED) complaining of vaginal bleeding for two days. The patient denied any abdominal pain, nausea, vomiting, or fever. On physical examination, she was well-appearing with stable vital signs. Her abdomen was nontender and nondistended. The pelvic exam revealed a small amount of dark blood without signs of active bleeding, an anteverted uterus of nine-weeks size and a closed cervix. Laboratory results revealed a quantitative beta-human chorionic gonadotropin level (beta-hCG) of 59,540 mIU/mL. A transabdominal ultrasound of the pelvis was performed, which revealed a uterus with multiple cystic areas within an enlarged echogenic endometrial cavity (Figure). The patient was thought to have a molar pregnancy (MP) and the Obstetrics team was consulted. As the patient was stable, she was scheduled for an outpatient dilatation and curettage. The subsequent pathology report described placental tissue with hydropic villi and no fetal tissue, consistent with a complete mole.
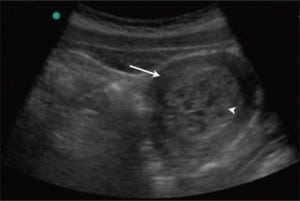
A complete mole is a type of hydatidiform mole in which there is a chromosomal abnormality, where all genetic material is usually paternal in origin. Patients commonly present with vaginal bleeding, uterine size that is larger than expected for gestational dates, hyperemesis, and pregnancy-induced hypertension in the first trimester.1 Diagnosis involves a beta-hCG level above what would be expected for the patient’s gestational age and a pelvic ultrasound that reveals a uterus with characteristic cystic areas and no evidence of a developing fetus.2 Although our patient did not have many of the classic symptoms, the sonographic findings were concerning for a MP. Bedside ultrasonography in the ED can help expedite the diagnosis and treatment. Admission is warranted if the MP is greater than 14 weeks gestation due to an increased risk of pulmonary embolism and respiratory distress.3
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted February 16, 2009; Revision Received April 3, 2009; Accepted April 15, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Eitan Dickman, MD, FACEP, RDMS, Department of Emergency Medicine, Maimonides, Medical Center, 4802 10th Ave., Brooklyn, NY 11219
Email: EDickman@maimonidesmed.org
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Houry DE, Abbott JT. Acute complications of pregnancy Marx J, editor. Rosen’s Emergency Medicine: Concepts and Clinical Practice 6th edSt Philadelphia, Pa: Mosby Elsevier; 2006:cha 177.
2. Eyvazzadeh AD, Levine D. Imaging of pelvic pain in the first trimester of pregnancy. Ultrasound Clinics. 2006;1:257–271.
3. Soper J. Gestational trophoblastic disease. Obstetrics Gynecology. 2006;108:176–187. [PubMed]


