| Author | Affiliation |
|---|---|
| Andrew C. Miller, MD | State University of New York Downstate Medical Center and Kings County Hospital Center, Brooklyn, NY University of Pittsburgh Medical Center, Pittsburgh, PA National Institutes of Health, Bethesda, MD |
| Diane Scheer, MD | University of Pittsburgh Medical Center, Pittsburgh, PA |
| Mark Silverberg, MD | National Institutes of Health, Bethesda, MD |
A 38-year-old woman with insulin-dependent diabetes reported four-days of flank pain, dysuria, polyuria and urinary urgency. Vital signs included blood pressure 113/70mmHg, heart rate 135/min, respiratory rate 24/min, and temperature 102.5°F. Exam revealed right cerebral vascular accident and suprapubic tenderness without guarding or rebound. Significant laboratory evaluations included a leukocyte count of 19.5×10−3/microlitre with 46% bands and toxic granulations. Hematocrit measured 30.9g/dL and platelets were 92×10−3/microlitre. Serum chemistries were significant for blood urea nitrogen 103mg/dL, creatinine 3.9mg/dL and lactate 7.8mmol/L. Urinalysis was nitrite positive, leukocyte esterase moderate, 8–12 leukocytes/hpf, and moderate bacteria. Urine and blood cultures were positive for pan-sensitive Escherichia coli. A non-contrast computed tomography (CT) abdomen image is depicted (Figure 1 and and2).2). The patient was treated with IV crystalloid, piperacillin/tazobactam and gentamycin, underwent percutaneous drainage, and was admitted to the intensive care unit where she suffered a prolonged course but survived to hospital discharge.

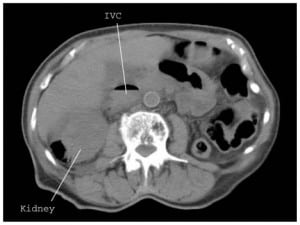
The patient has emphysematous pyelonephritis (EPN) with pneumo-vena cava. EPN is a life-threatening, necrotizing infection of the renal parenchyma, collecting system, or perinephric tissue by gas-forming uropathogens (eg. E. coli, Klebsiella, Proteus).1 Risk factors include diabetes (>90% of patients), female gender, immunosuppression, renal disease or genitourinary obstruction.1Symptoms include fever, flank/back pain, dysuria, nausea/vomiting, renal failure or hyperglycemia. Disturbed consciousness, thrombocytopenia and sepsis are associated with increased mortality.1,2CT is the preferred imaging modality. Class I contains gas within the collecting system.1,2 Class II contains intraparechymal gas.1,2 In class IIIa, gas or abscess extends into the perinephric space, and in IIIb into the pararenal space. Class IV signifies bilateral or solitary kidney involvement.1,2Treat EPN with aggressive fluid resuscitation, broad-spectrum antibiotics targeting gram-negative bacteria, glycemic control and electrolyte maintenance. Additionally, treat class I or II disease with percutaneous drainage and class III and IV disease with percutaneous catheter placement. Nephrectomy is reserved for severe or refractory cases.1
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted March 22, 2010; Revision Received May 18, 2010; Accepted May 24, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Andrew C Miller MD. Division of Pulmonary, Allergy, & Critical Care Medicine. NW 628 MUH. 3459 Fifth Ave. Pittsburgh, PA. 15213
Email: taqwa1@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Pontin AR, Barnes RD. Current management of emphysematous pyelonephritis. Nat Rev Urol.2009 May;6(5):272–9. [PubMed]
2. Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Inter Med. 2000;160:797–805.


