| Author | Affiliation |
|---|---|
| Jeffery C. Ashburn, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
| Tamara Harrison, BS | University of Washington Medical Center, Department of Medicine, Seattle, Washington |
| James J. Ham, MD | Madigan Army Medical Center, Department of Emergency Medicine, Tacoma, Washington |
| Jared Strote, MD, MS | University of Washington Medical Center, Division of Emergency Medicine, Seattle, Washington |
ABSTRACT
Introduction:
Emergency physicians (EP) frequently estimate blood loss, which can have implications for clinical care. The objectives of this study were to examine EP accuracy in estimating blood loss on different surfaces and compare attending physician and resident performance.
Methods:
A sample of 56 emergency department (ED) physicians (30 attending physicians and 26 residents) were asked to estimate the amount of moulage blood present in 4 scenarios: 500 mL spilled onto an ED cot; 25 mL spilled onto a 10-pack of 4 × 4-inch gauze; 100 mL on a T-shirt; and 150 mL in a commode filled with water. Standard estimate error (the absolute value of (estimated volume − actual volume)/actual volume × 100) was calculated for each estimate.
Results:
The mean standard error for all estimates was 116% with a range of 0% to 1233%. Only 8% of estimates were within 20% of the true value. Estimates were most accurate for the sheet scenario and worst for the commode scenario. Residents and attending physicians did not perform significantly differently (P > 0.05).
Conclusion:
Emergency department physicians do not estimate blood loss well in a variety of scenarios. Such estimates could potentially be misleading if used in clinical decision making. Clinical experience does not appear to improve estimation ability in this limited study.
INTRODUCTION
Blood loss in the emergency department (ED) is common. Physicians are frequently required to estimate the loss from hemoptysis, epistaxis, rectal bleeding, vaginal bleeding, and traumatic injury as part of their physical examination and ongoing evaluation. Initial bedside hematocrit can often be a poor indicator of acute blood loss: children have a high physiologic reserve, and many cardiac medications, such as β-blockers and calcium channel blockers, affect the normal response to blood loss. These examples are just a few in which estimation of blood loss can alter the assessment of volume status.
Most prior research on blood loss estimation has evaluated practitioners from other specialties. Obstetricians, general surgeons, trauma surgeons, nurses, and paramedics have all been found to be neither precise nor accurate.1–6 In a recent study, emergency physicians (EP) and paramedics were given vital signs and mechanism of injury then asked to visually estimate blood loss in trauma scenarios. As in other studies, estimations were again found to be both inaccurate and affected by the patient’s presentation.7
The objective of our study was two-fold: (1) to examine ED physicians’ accuracy when estimating blood loss on different surfaces in a broad and general set of clinically encountered situations; and (2) to perform a pilot study to compare the accuracy of attending and resident physicians in these tasks.
METHODS
Study Design and Population
A prospective, single-blinded, observational design was used. Participants were emergency physician attending physicians and residents from a single residency program, working in academic hospitals in both urban and suburban settings. Participation was voluntary and a convenience sample of participants was chosen over 4 separate academic meetings.
Study Protocol
Moulage blood was used for all estimations (Ben Nye Stage Blood, Los Angeles, California). Four estimation stations were created: (1) 500 mL of blood spilled onto a standard, white bed sheet, which was spread over an ED bed; (2) 25 mL of blood spilled onto ten 4 × 4-inch gauze sponges; (3) 100 mL of blood spilled on a T-shirt and allowed to dry; and (4) 150 mL of blood added to a commode with 3 L of water. Volumes were chosen to represent a common range of blood loss seen in the ED. Data were collected on 4 separate occasions (grand rounds and faculty meetings) at varying times in order to maximize the number of participating physicians. There was no fundamental difference about the events or the participants at each event.
Physicians were asked to assess each blood loss scenario and estimate the amount of blood loss in milliliters. The same T-shirt and gauze were used for all days. The bed sheet and commode stations were made with fresh blood for each participation group. Subjects were aware of the amount of water that had been in the commode before blood addition. The first bed sheet station created was measured and photographed and subsequent stations were recreated to be as consistent as possible. One researcher interviewed all participants; he presented the scenarios and asked for estimates in the same way for each participant.
Demographic data on gender and years of clinical experience post-MD were also collected.
Verbal consent was obtained; the study was approved by the human subjects division and qualified for exemption from federal regulations for the protection of human subjects at all participating institutions.
Data Analysis
Estimate error for each group was standardized by converting to percentage error (ie, the absolute value of: estimated volume − actual volume/actual volume × 100). Attending physicians’ and residents’ performances were compared by using the unpaired student t test (IBM SPSS Statistics, version 18, Chicago, Illinois).
RESULTS
A total of 56 subjects participated; all verbally consented and completed all 4 stations.
Of the participants, 64% were male (2 did not choose a gender). The median experience among the 30 attending physicians (54%) who participated was 8 years (first/third quartile = 6/21; 3 did not respond) and the median experience among the 26 residents was 2 years (first/third quartile = 0.5/2.5; 7 did not respond).
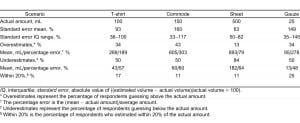
Overall standard error averages and interquartile ranges for each scenario are listed in Table 1. For all scenarios combined, mean standard error was 116% with a range from the rare correct answer to 1,233%. Only 8% of estimates were within 20% of the correct answer, while 70% of estimates were within 100% of the correct answer.
Other than for the sheet station, there was not a strong trend toward underestimation or overestimation; underestimates were 50% for the T-shirt station, 50% for the commode station, 84% for the sheet station, and 50% for the gauze station. Only 16% of all estimates were within 20% of the true value.
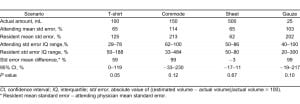
Table 2 compares attending physician and resident performance for each scenario. In general, attending physicians had less mean error and less extremes of error. Although no significant difference was found, trends toward superior attending physician accuracy were seen in each scenario except the sheet station.
DISCUSSION
This study adds to the literature showing that ED physicians, like other specialists,1–7 do not estimate blood loss well on a variety of surfaces. The large range of answers seen suggests that physicians are imprecise in addition to being inaccurate. This is consistent with prior studies that have examined other specialties’ estimates of blood loss in a variety of scenarios, including active patient blood loss,1–3, 6blood spilled on the ground,5 blood spilled onto drapes and sponges,4 blood placed in a commode,8 and blood loss estimated at the scene of trauma.7
Estimates ranged widely, averaging more than 100% off from the actual amounts. Prior studies have suggested that health professionals tend to overestimate small losses (<150 mL) and underestimate large ones (>150 mL).3,5–8 Our study found similar results. Comparing the larger blood loss on the bed sheet scenario (500 mL) to the smaller blood loss in the T-shirt scenario (100 mL), there were considerably more underestimates with the larger loss.
The commode and gauze scenarios present an additional challenge of estimating blood in a larger body of fluid and in a very small quantity, respectively; this led to a greater range of answers and more evenly distributed overestimates and underestimates. Patients with complaints of heavy vaginal bleeding or rectal bleeding frequently report blood loss while on the commode and occasionally ask physicians to evaluate losses. This may have clinical relevance because physicians may be just as inaccurate when making estimations in this scenario. Also, EPs are poor at estimating small losses and gauze saturation. Gauze is frequently used to absorb blood during epistaxis, and we observe that ongoing losses could significantly affect the estimation of cumulative loss. It is worthwhile for practitioners to be aware of the further decreased precision and accuracy in these types of situations.
The present study had similarities to a prior study that examined estimations of blood loss made by ED patients.9 Nearly identical commode, T-shirt, and gauze scenarios were presented. It is notable that resident and attending EPs had approximately one half and one quarter, respectively, of the average and standard deviation of standard error demonstrated by the patients. This difference makes intuitive sense, as making clinically relevant estimates and observing known quantities of various liquids is part of the day-to-day practice of the emergency physician; it is notably different from a prior study that showed no significant difference between physicians and patients estimating blood in a commode.8
No significant difference was found between resident and attending physician performance on each test, consistent with a prior study looking at paramedics with different levels of experience.5 There was, however, a strong trend toward superior attending physician performance, with residents demonstrating approximately double the mean error in all scenarios but the bed sheet. Also, there was no significant difference when comparing gender within the scenarios, although the small numbers used likely did not have the power to show a difference; other studies have not found a gender difference.9 Whether there would be utility in instituting some form of training is unclear. In the study by Moscati et al5, the blood loss was revealed to the subjects in the study, then slide show presentations were used to train subjects on the appearance of various amounts of blood loss. The subjects were retested at a later date and found to have significantly improved. Given that small effort may lead to large estimation improvement, further research should consider training programs for physicians and how to incorporate these into emergency medicine (EM) or advanced trauma life support training.
The potential clinical relevance of misusing estimations of blood does exist, especially in early evaluation when the hematocrit is unreliable, when multiple different observers are making continued mistakes, in children whose total body blood volume is lower, and for the elderly or those taking medications that may change the physiologic response to blood loss. Given these situations, we feel that there is value in creating awareness about common conditions causing overestimates and underestimates and the overall inaccuracy of EPs in making and using such estimates in clinical care.
LIMITATIONS
Our study has numerous limitations. Our results may not accurately reflect estimations of actual blood loss in the clinical setting. The study also does not reflect real-life situations in which mechanism of injury and vital signs can influence estimates. However, a prior study has shown physicians are no better when given this information.7
Because our study was unblinded to the investigators, bias could have been introduced in the way the study was presented to each patient. Also, physicians could not spread the blood or use other hands-on techniques for estimating blood loss because this would affect the scenario for other subjects. Scenarios that were created each day may have had small but important differences, affecting estimates in some way.
The physicians in this study came from 1 residency program in 1 geographic location in the United States; the study may not reflect the estimation skills of physicians in other academic programs, community settings, or other geographic areas.
Finally, this pilot study was not prospectively powered and the sample sizes used may not have been large enough to show a difference between attending physicians and residents.
CONCLUSION
Blood loss estimates are frequently made by EPs. Like all historical findings, such estimates could potentially be useful as 1 piece in an array of historical points, physical examination findings, and laboratory data results, in an effort to create a complete picture of the severity of the process. This and prior studies suggest that blood loss estimates are difficult for patients and healthcare providers alike, and interpretation of these numbers should therefore be made with extreme caution, if used at all. Further study may be warranted on the effect of blood estimation in clinical decision making, as well as the value of adding estimation skills to EM training.
Footnotes
Supervising Section Editor: H. Bryant Nguyen, MD, MS
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence
Jared Strote, MD, MS
University of Washington Medical Center, Division of Emergency Medicine, Box 356123, 1959 NE Pacific St, Seattle, WA 98195
E-mail: strote@u.washington.edu.
REFERENCES
1. Brant HA. Precise estimation of postpartum haemorrhage: difficulties and importance. Br Med J.1967;1:398–400. [PMC free article] [PubMed]
2. Duthie SJ, Ven D, Yung GL, et al. Discrepancy between laboratory determination and visual estimation of blood loss during normal delivery. Eur J Obstet Gynecol Reprod Biol. 1991;38:119–124.[PubMed]
3. Larsson C, Saltvedt S, Wiklund I, et al. Estimation of blood loss after cesarean section and vaginal delivery has low validity with a tendency to exaggeration. Acta Obstet Gynecol Scand. 2006;85:1448–1452. [PubMed]
4. Meiser A, Casagranda O, Skipka G, et al. Quantification of blood loss. How precise is visual estimation and what does its accuracy depend on. Anaesthesist. 2001;50:13–20. [article in German]? [PubMed]
5. Moscati R, Billittier AJ, Marshall B, et al. Blood loss estimation by out-of-hospital emergency care providers. Prehosp Emerg Care. 1999;3:239–242. [PubMed]
6. Razvi K, Chua S, Arulkumaran S, et al. A comparison between visual estimation and laboratory determination of blood loss during the third stage of labour. Aust N Z J Obstet Gynaecol. 1996;36:152–154. [PubMed]
7. Frank M, Schmucker U, Stengel D, et al. Proper estimation of blood loss on scene of trauma: tool or tale? J Trauma. 2010;69:1191–1195. [PubMed]
8. Simpson RR, Kennedy ML, Chew SB, et al. Do patients assess rectal bleeding accurately? ANZ J Surg.2001;71:650–651. [PubMed]
9. Strote J, Mayo M, Townes D. ED patient estimation of blood loss. Am J Emerg Med. 2009;27:709–711. [PubMed]


