| Author | Affiliation |
|---|---|
| Sanjay Arora, MD | Department of Emergency Medicine, Keck/USC School of Medicine, Los Angeles, CA |
INTRODUCTION
Emergency physicians must be comfortable and confident in providing safe and effective procedural sedation and analgesia (PSA). Goals of PSA include providing an adequate level of sedation while minimizing pain and anxiety, maximizing amnesia, minimizing the potential for adverse drug-related events, controlling behavior, and maintaining a stable cardiovascular and respiratory status. The ideal pharmacologic agent for PSA would accomplish all of these goals, and would have a quick onset and offset, be safe in all age groups, be inexpensive, and be equally efficacious in multiple routes of administration. Unfortunately, at this time no single agent exists that has all of the aforementioned qualities, so physicians must use combinations of different drugs at varying does to achieve as many of the desired goals as possible. The most recent PSA combination to be described in the literature is that of low-dose ketamine and propofol (“ketofol”). In this article we attempt to describe the postulated benefits of using these two agents together and examine the safety and efficacy of the combination.
Background
Ketamine was developed in the 1960s as a safer and more predictable anesthetic than its precursor phencyclidine (PCP). It is a unique agent in procedural sedation and analgesia (PSA) in that it is a “dissociative” anesthetic that functions by blocking communication between the thalamic and limbic regions of the brain, thereby preventing the brain from processing external stimuli.1 It provides excellent amnesia and analgesia, and preserves muscle tone maintaining protective airway reflexes and spontaneous respiration.2,3Despite its obvious advantages over other agents, some practitioners are hesitant to use ketamine alone secondary to its propensity to cause vivid and frightening emergenct reactions.4 Additional significant adverse effects include sympathomimetic effects and vomiting when administered in sedating doses.5
Propofol is a non-barbiturate sedative hypnotic developed in Europe in the 1970s and was gradually utilized by anesthesiologists in the United States over the next two decades. Relatively recently its use has spread into the Emergency Department (ED) as a part of PSA. Its popularity as a PSA agent is growing rapidly due mainly to its favorable pharmacokinetic profile as the lipid solubility confers a quick onset and short recovery time.6 It also has the advantages of functioning as an antiemetic, an anticonvulsant, and an amnestic agent.7 Although extremely effective and potent, propofol use is limited by a relatively high incidence of dose-dependant hypotension and respiratory depression.7,8,9
It is postulated that combining these two agents for PSA may preserve sedation efficacy while minimizing their respective adverse effects. This is due partly to the fact that many of the aforementioned potential adverse effects are dose-dependant, and when used in combination the doses administered of each can be reduced.10 Also, the cardiovascular effects of each are opposing in action, thus theoretically balancing each other out when used together. This theoretical advantage of ketofol producing a more stable hemodynamic and respiratory profile was tested and found to be true in a group of healthy patients receiving general anesthesia.11 Although there is a significant amount of literature describing the use of ketofol in infusion form, in this article we attempt to review all the published literature describing the use of ketofol in bolus form as would be applicable for PSA in the ED.
METHODS
Both MEDLINE and Pubmed were searched using ketamine, propofol, ketofol, conscious sedation, and procedural sedation as search terms. This resulted in the identification of 31 abstracts. All abstracts were reviewed and those that described the use of the combination of ketamine and propofol in intravenous bolus form were included for review. Those that described studies in animals, in healthy volunteers, or that described the administration of propofol and ketamine either in isolation, in infusion form, or for general anesthesia were excluded. An ancestral search of the references of all included articles was performed using the same inclusion and exclusion criteria to ensure that no relevant articles were missed.
LITERATURE REVIEW
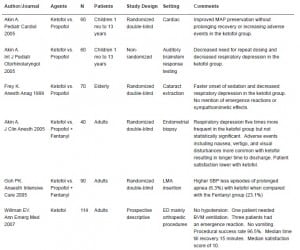
Six studies met inclusion criteria and are further discussed (Table).
Ketofol versus Propofol
There are two published trials in pediatric patients comparing propofol monotherapy to ketofol. The first is a randomized double-blind study in 60 patients between one month and 13 years of age undergoing cardiac catheterization who received sedation with propofol (1.5 mg/kg) monotherapy or propofol (1.5 mg/kg) plus ketamine (0.5 mg/kg).12Mean arterial pressure (MAP), heart rate, respiratory rate, and peripheral oxygen saturation were recorded at pre-determined time intervals. Time to recovery and adverse events were also noted. They found a significant (defined a priori as >20%) decrease in MAP in 11 patients in the propofol monotherapy group and three patients in the ketofol group. No other significant differences in recorded vital-sign measurements were found. Time to recovery was almost identical in the two groups, and the number of adverse events was not statistically different. These findings led the authors to conclude that the addition of low-dose ketamine to propofol preserved MAP without prolonging recovery or increasing the incidence of adverse events.
In the second pediatric study propofol (1.5 mg/kg) monotherapy was compared to propofol (1.5 mg/kg) plus ketamine (0.5 mg/kg) in a non-randomized trial in 60 patients between one and 13 years of age undergoing auditory brainstem response testing.13 Sedation was maintained with repeat boluses at half the original doses at the discretion of the treating physician. Blood pressure, respiratory rate, and peripheral oxygen saturation were recorded at pre-determined time intervals. Desaturation was defined as a 10% decrease in peripheral oxygen saturation when compared to baseline, and apnea was defined as cessation of respiration for 15 seconds or more. The investigators noted that a repeat dose of medication was needed in 21/30 patients in the propofol group and in 8/30 in the ketofol group. There were no cases of desaturation in the ketofol group, but in the propofol group 4/30 experienced desaturation and 6/30 had apnea. At both the three and five-minute time intervals blood pressure and heart rate were significantly lower in the propofol group than in the ketofol group. In summary, the authors concluded that the addition of low dose ketamine to propofol reduced the risk of respiratory depression and the need for repeat medication administration.
In adults there is only one study comparing propofol monotherapy to ketofol. In this randomized double-blind study, 70 elderly patients receiving retrobulbar nerve blocks for cataract extraction were assigned to receive either propofol in small boluses or propofol in small boluses with the addition of ketamine (30 mg) in the first bolus.14 They found that patients in the ketofol group had a significantly shorter time until sedation (164 +/− 67 s) when compared to the propofol group (235 +/− 137 s). Also, two patients in the propofol group needed ventilatory assistance compared to zero patients in the ketofol group. This led these researchers to conclude that adding ketamine to propofol resulted in faster onset of sedation while decreasing respiratory compromise. It is important to note that the authors did not assess other important adverse events including emergence reactions and sympathomimetic effects, which are of special importance in elderly patients.
Ketofol versus Propofol-Fentanyl
Another popular drug combination for PSA consists of propofol and fentanyl, and there are two studies that compare ketofol to this combination. In a randomized double-blind study performed in 40 adult patients undergoing endometrial biopsy, the combination of propofol (1 mg/kg) plus fentanyl (1 ug/kg) was compared to the combination of propofol (1 mg/kg) plus ketamine (0.5 mg/kg).15 Heart rate, systolic and diastolic blood pressure, respiratory rate, peripheral oxygen saturation, adverse events, time to recovery, and time to discharge were recorded. Although respiratory depression was five times more frequent in the ketofol group, neither this difference nor any other difference in vital signs was found to be statistically significant. Time to recovery was similar; however time to discharge was longer in the ketofol group secondary to the increased presence of adverse events including nausea, vertigo, and visual disturbances. In a post-procedure phone follow-up interview conducted 24 hours after discharge 95% of patients in the propofol plus fentanyl group stated they were satisfied and would like the same combination in the future, versus only 60% of patients in the ketofol group. These authors concluded that although both regimens seem safe, ketofol had more adverse events leading to a longer time until discharge and had a lower overall patient satisfaction.
The second is a randomized double-blind study, in which 90 total patients having a laryngeal mask airway (LMA) placed received propofol (2.5 mg/kg) with either ketamine (0.5 mg/kg), fentanyl (1 ug/kg), or placebo normal saline.16 When measured vital signs and pre-determined time points and ease of LMA insertion, they found the ketofol group had a significantly higher systolic blood pressure than the other two groups and the incidence of prolonged apnea (>120 s) was higher in the fentanyl group (23.1%) than in either the ketofol group (6.3%) or the normal saline group (3.3%). They concluded that ketofol provided equivalent LMA insertion conditions while maximizing hemodynamics and minimizing apnea. Even though efficacy was assessed in this study, no attempt was made to qualify important adverse events such as emergence reactions.
Ketofol in the Emergency Department
There is only one published prospective study using ketofol for PSA conducted in the ED setting. In this descriptive study 114 patients requiring PSA for mainly orthopedic procedures were given a 1:1 mixture of propofol (10 mg/ml) and ketamine (10 mg/ml) in 1 to 3 ml aliquots titrated at the discretion of the treating physician.17 They recorded dose administered, vital signs at pre-determined intervals, presence or absence of adverse events, procedural success, time until recovery, and physician, nurse and patient satisfaction. The mean dose of medication administered was 0.75 mg/kg of ketamine and 0.75 mg/kg of propofol. No patient became hypotensive or had evidence of poor perfusion. Transient hypoxia occurred in 2.6% of patients (95% CI 0.6 to 7.5%) and of these one (0.9%; 95% CI 0.02 to 4.8%) required bag valve mask ventilation. Three patients (2.6%; 95% CI 0.6–7.5%) had an emergence reaction, one of whom received midazolam. No patient had vomiting or aspiration. Procedural success rate in this study without the use of adjunctive medications was 96.5%. Median time until recovery was 15 minutes (range 5 to 45 minutes) and median physician, nurse, and patient satisfaction scores were 10 on a 1-to-10 scale.
DISCUSSION
The combination of ketamine and propofol has been used with great success in anesthesiology for many years, but only recently has it begun to spread into other fields of medicine. Because ketofol is a relatively new idea for most practitioners, there is very little in scientific literature on its use in bolus form for PSA. The studies that have been conducted are small in size and thus lack the power to detect significant differences in all of their stated endpoints. Although most studies do attempt to evaluate safety as measured by respiratory and cardiovascular status, very few look at the frequency of other adverse events such as emergence reactions which, if present, may cause practitioners to veer away from ketofol and use another regimen that is found to be equally efficacious. Additionally, in the reviewed literature several different dosing regimens are used, making it hard to reconcile the results of the various studies.
In the two pediatric studies discussed in this review the authors chose to compare ketofol to propofol monotherapy. It would have been more useful look for an efficacy difference between ketofol and ketamine monotherapy, which is used far more frequently than propofol monotherapy in children.12,13 Importantly, only one study was actually conducted in the ED setting with ED procedures using bolus dose ketofol.17 The authors found ketofol to be both safe and efficacious, but this study was purely descriptive and therefore cannot be used to conclude that the combination is better than either agent as monotherapy. It is unclear if the conclusions of the rest of the reviewed studies describing the use of ketofol in other clinical settings and types of procedures can be generalized to its use in the ED.
CONCLUSION
Although all but one of the published studies reviewed in this article conclude that the combination of ketamine and propofol in bolus form provides safer and more efficacious sedation, larger randomized, prospective studies conducted in the ED with sufficient power to use stability of vital signs and procedural success as endpoints are needed. From the literature reviewed one can conclude that ketofol appears to be safe and efficacious for use in the ED for PSA. However, as the reviewed studies are small, reporting of adverse events is often limited, and the only study conducted in the ED is not a randomized trial, the literature is not strong enough to definitively conclude that ketofol is better than either agent alone or than either agent used in combination with a different agent.
Footnotes
Submission history: Submitted May 24, 2007; Accepted November 1, 2007
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Sanjay Arora, MD, Department of Emergency Medicine, LAC + USC Medical Center, 1200 N. State Street, Room 1011, Los Angeles, CA 90033
Email: sanjayar@usc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Green SM, Krauss B. The semantics of ketamine [editorial] Ann Emerg Med.2000;39:480–482. [PubMed]
2. Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet.2006;367:766–780. [PubMed]
3. Warncke T, Stubhaug A, et al. Ketamine, an NMDA receptor antagonist, suppresses spatial and temporal properties of burn-induced secondary hyperalgesia in man: a double-blind, cross-over comparison with morphine or placebo. Pain. 1997;72:99–106.[PubMed]
4. Green SM, Rothrock SG, Lynch EL, et al. Intramuscular ketamine for pediatric sedation in the emergency department: safety profile in 1022 cases. Ann Emerg Med.1998;31:688–697. [PubMed]
5. Roback MG, Wathen JE, et al. Adverse events associated with procedural sedation and analgesia in a pediatric emergency department: a comparison of parenteral drugs. Acad Emerg Med. 2005;12:508–513. [PubMed]
6. McLeskey CH, Walawander CA, Nahrwold, et al. Adverse events in a multicenter phase IV study of propofol: evaluation by anesthesiologists and postanesthesia care unit nurses.Anesth Analg. 1993;77:S3–S9. [PubMed]
7. Short SM, Aun CS. Haemodynamic effects of propofol in children. Anaesthesia.1991;46:783–785. [PubMed]
8. Bassett KE, Anderson JL, et al. Propofol for procedural sedation in children in the emergency department. Ann Emerg Med. 2003;42:773–782. [PubMed]
9. Hig CC, Jr, McLeskey CH, Nahrwold ML, et al. Hemodynamic effects of propofol: data from over 25,000 patients. Anesth Analg. 1993;77:S21–S29. [PubMed]
10. Camu F, Vanlersberghe C. Pharmacology of systemic analgesics. Best Pract Res Clin Anaesthesiol. 2002;16:475–488. [PubMed]
11. Morse Z, Sano K, Kanri T. Effects of a propofol-ketamine admixture in human volunteers. Pac Health Dialog. 2003;10:51–54. [PubMed]
12. Akin A, Esmaoglu A, Guler G, et al. Propofol and propofol-ketamine in pediatric patients undergoing cardiac catheterization. Pediatr Cardiol. 2005;26:553–557.[PubMed]
13. Akin A, Esmaoglu A, Tosun Z, et al. Comparison of propofol with propofol-ketamine combination in pediatric patients undergoing auditory brainstem response testing. Int J Pediatr Otorhinolaryngol. 2005;69:1541–1545. [PubMed]
14. Frey K, Sukhani R, Pawlowski J, et al. Propofol versus propofol ketamine sedation for retrobulbar nerve block: comparison of sedation quality, intraocular pressure changes, and recovery profiles. Anesth Analg. 1999;89:317–321. [PubMed]
15. Akin A, Guler G, Esmaoglu A, et al. A comparison of fentanyl-propofol with a ketamine-propofol combination for sedation during endometrial biopsy. J Clin Anesth.2005;17:187–190. [PubMed]
16. Goh PK, Chiu CL, Wang CY, et al. Randomized double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care. 2005;33:223–228. [PubMed]
17. Willman EV, Andolfatto G. A prospective evaluation of “ketofol” (ketamine/propofol combination for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2007;49:23–30. [PubMed]