| Author | Affiliation |
|---|---|
| J. Scott Bomann, DO | Wellington Regional Hospital, Department of Emergency Medicine, Wellington, New Zealand |
| Michael Seman, BSc, MBBS | Wellington Regional Hospital, Department of Emergency Medicine, Wellington, New Zealand |
| Darrell Sutijono, MD | Kaiser Permanente Santa Clara Medical Center,Department of Emergency Medicine, Santa Clara, California |
| Bridget Rogers, MD | University of Colorado, Department of Radiology, Denver, Colorado |
INTRODUCTION
Approximately 1% of all emergency department (ED) visits are for treatment of urinary tract stone disease (renal colic, kidney stones, urolithiasis).1 Renal colic is a common condition affecting approximately 7–13% of the population during their lifetime and those who are afflicted are likely to have recurrent attacks throughout their lives.2, 3
Noncontrast computed tomography (CT) of the abdomen and pelvis (CT KUB) is the gold standard imaging modality for urolithiasis. CT, however, is costly and exposes patients to potentially dangerous amounts of ionizing radiation, especially when performed repeatedly over time. Ultrasound (US) has been studied extensively in urolithiasis, specifically with regard to the finding of hydronephrosis as a secondary sign. Mentions of sonographic bladder wall abnormalities in renal colic, however, are rare in the literature and limited exclusively to a few brief descriptions of impacted uretovesicle junction (UVJ) stones.4,5
Through the following case series, we present sonographic bladder wall findings in patients with renal colic. These similar appearing abnormalities, which we propose to uniformly name the “bladder bulge,” have not, to our knowledge, been previously discussed in the emergency medicine literature. One variant, in fact, may represent a novel sonographic description unto itself. The bladder bulge is easily obtained and can best be seen on axial views as a unilateral, inward bulging and/or focal thickening of the bladder wall on the symptomatic side, at the approximate level of the uretovesical junction (UVJ).
METHODS
We attempted to identify previous descriptions of bladder wall abnormalities in urolithiasis through a Medline search of English language journals using the following Medical Subject Heading (MeSH) terms and text words: Ureteral calculi or renal calculi orurolithiasis or renal colic or ureterolithiasis and combined with ultrasonography and bladder. Two hundred thirtysix articles were found. We then searched using only the keywordpseudoureterocele. Eight articles were found. We limited our search to English language, humans and adults. Of the first search, 2 articles briefly mentioned ureteral prolapse and edema as seen on US at the UVJ.4,5 The second search yielded a single sonographic description of a pseudoureterocele in a patient with tuberculosis of the bladder.6
The following 7 cases presented to 2 different ED’s between June 2011 and November 2011. These departments are part of general tertiary hospitals that include trainees in emergency medicine. The sonographers included 2 emergency medicine physicians who are fellowship-trained in emergency ultrasound and one emergency medicine trainee with limited formal training in ultrasound.
The patients were identified retrospectively through a search of the emergency department ultrasound (EDUS) logbook and image archive. All received both a bedside ultrasound performed by an emergency physician that included views of the bladder and affected kidney, and a CT KUB confirming the presence, location and size of the stone. We selected the axial US images most representative of the bladder bulge, together with the corresponding CT image, and presented them to a board certified radiologist for interpretation. The radiologist was blinded to the purpose of the project and given specific instructions to provide a highly detailed interpretation, describing as many aspects of the anatomy as possible, including elements that may not normally be mentioned in a standard reading. Only the portion of the reading relating to the bladder wall is included here. The radiologist also determined the presence or absence of hydronephrosis on EDUS.
Ultrasound Technique
Patients’ bladders were thoroughly interrogated transabdominally in the axial plane using a low frequency (1–4 MHz), curvilinear probe. There was no standardization of bladder volume.
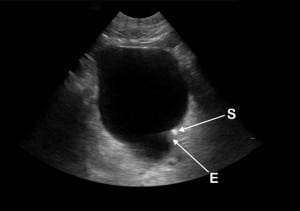
Cases
The following 7 patients, aged 28 to 58, presented with symptoms consistent with renal colic. The images show variations of the bladder bulge and are followed by our radiologist’s interpretation. CT images are included where they were felt to represent the bladder bulge. Table 1 contains additional clinical variables.
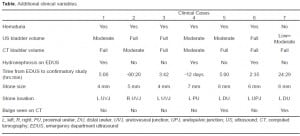
Case 1: A 33-year-old male with a left UVJ stone
Radiologist description: focal wall thickening and inward bulge along the left posterior wall, centered around a subcentimeter echogenic structure with shadowing, consistent with a distal ureteral calculus.
Emergency department ultrasound (EDUS). Direct stone visualization (S) with shadowing (Sh) and protrusion of the left posterior bladder wall.
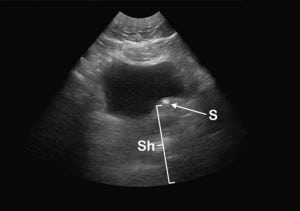
Case 2: A 33-year-old male with a right UVJ stone.
Radiologist description: focal thickening of the right posterior bladder wall, with slight inward protrusion of this portion of the wall. There is also the suggestion of a small cystic focus at the level of the right UVJ, which may represent dilation of the intramural portion of the distal ureter.
Emergency department ultrasound (EDUS). A pseudoureterocele (P) showing characteristic cystic appearance at the right posterior bladder wall.
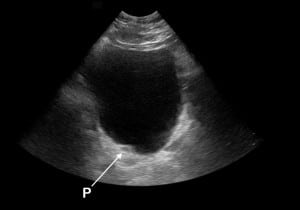
Case 3: A 38-year-old male with a left UVJ stone
Radiologist description: Focal wall thickening around an echogenic calculus along the left posterior wall, with protrusion of the thickened wall into the bladder lumen.
Emergency department ultrasound (EDUS). Direct stone visualization (S) with edema (E) and possible ureteric prolapse (P) at the left posterior bladder wall.
Case 4: A 44-year-old female with a left ureteric stone (likely UVJ)
Radiologist description: inward protrusion of the left posterior bladder wall into the lumen.
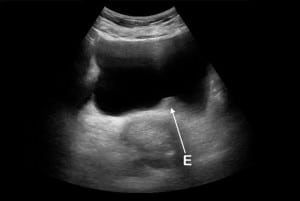
Emergency department ultrasound (EDUS). Inward protrusion from edema (E) without stone visualization at the left posterior bladder wall.
Case 5: A 58-year-old man with a left distal ureteric stone (not near the UVJ).
Radiologist description: focal wall thickening and inward protrusion of the left posterior bladder wall.
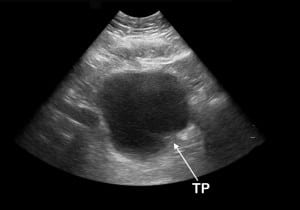
Emergency department ultrasound (EDUS). Thickening (T) and inward protrusion (P) at the left posterior bladder wall.
Radiologist description: minimal asymmetry along the posterior bladder wall, with an inward bulge along the left side.

Computed tomography (CT) of the abdomen and pelvis (CT KUB). Inward protrusion (P) of the left posterior bladder wall.
Case 6: A 28-year-old male with a left proximal ureteric stone.
Radiologist description: irregularity of the bladder wall, with focal inward bulge and apparent thickening of the left posterior wall.
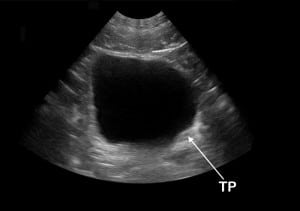
Emergency department ultrasound (EDUS). Thickening (T) and inward protrusion (P) of the left posterior bladder wall.
Case 7: A 44-year-old man with a left proximal ureteric stone
Radiologist description: minimal asymmetry along the posterior bladder wall, with flattening of the left side.
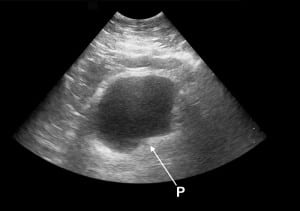
Emergency department ultrasound (EDUS). Inward protrusion (P) of the left posterior bladder wall.
Radiologist description: slight inward protrusion of the left posterior bladder wall.

Computed tomography (CT) of the abdomen and pelvis (CT KUB). Flattening (F) of the left posterior bladder wall.
All 7 patients in the case series had confirmed ureterolithiasis and an EDUS that showed a unilateral inward bulge of their bladder on the symptomatic side. Stone size and location varied (Table). In cases 5 and 7, there was the suggestion of a correlating bulge seen on CT (Figures 5a, ,7a), although this finding was subtler. The bladder bulge sign is therefore felt to be primarily, if not exclusively, a sonographic finding. Case 4 had the CT performed 12 days prior to the EDUS making it likely that her stone had migrated to the UVJ by the time of her EDUS. Four of our patients had no hydronephrosis. One patient had neither hydronephrosis nor hematuria.
DISCUSSION
Renal colic is a painful, but generally benign condition with a hospital admission rate of 6–10%.1,7 Fortunately, less than 10% of renal colic patients require intervention within 7 days and only 1–3% of patients undergoing CT KUB have an alternate diagnosis requiring emergent intervention.1,7–9 Broder showed that of 262 patients who received a CT KUB for suspected renal colic, 244 (93%) had neither a need for urologic intervention nor an emergent cause for their symptoms.7
It is estimated that 1 CT abdomen/pelvis contains the equivalent radiation dose of 1000 single-view (posterior-anterior) chest x-rays, conferring an estimated lifetime cancer risk of 6:1000 in a 20-year-old.10,11 Due to the nature of their disease, renal colic patients are likely to have multiple presentations to the ED and multiple CTs, as most emergency physicians, and even many radiologists, are not fully aware of the degree of radiation exposure.12 To decrease their radiation risks, urolithiasis patients need an imaging modality that is harmless and effective. Ultrasound is safe, and is now recommended by the European Association of Urology as the first-line imaging modality in suspected renal colic.13 Until American clinicians move away from CT and begin ordering formal US studies for these patients, emergency physicians will likely continue to perform most of the renal colic ultrasound studies.
Direct sonographic visualization of the ureters is extremely difficult. Hydronephrosis, therefore, is used as a surrogate finding in patients with suspected renal colic. The sensitivity and specificity of bedside ultrasound for the detection of hydronephrosis have been shown to be 87% and 83% respectively.14 However, hydronephrosis is not always present and mild hydronephrosis is a subtle finding. In addition, a recent study showed that bedside sonography looking for hydronephrosis had only a limited impact on the diagnostic impression of emergency physicians.15 Traditional EDUS renal colic studies do not include a search for bladder wall abnormalities and the concepts of looking for these findings and examining their diagnostic implications have not been previously discussed in the literature.
A pseudoureterocele is an obscure term defined as “a lesion causing similar [to a ureterocele] lucent-filling defect at the uretovesical junction on IVU (intravenous urogram).”16 This case series introduces the bladder bulge as a unifying sonographic description of bladder wall abnormalities seen in patients with ureterolithiasis that includes pseudoureteroceles, focal wall thickening, edema, ureteric prolapse and inward wall protrusion, all at the level of the UVJ. There may be some degree of overlap among the findings. Our cases suggest that the mechanism by which the bladder bulge occurs is not entirely explained by stone impaction at the UVJ. There may be additional unilateral detrusor hyperactivity from inflammatory mediators released during ureteral injury. Prostanoid and endothelin subtypes are known to directly contract human detrusor muscle.17 This would explain the inward wall protrusion seen in cases 5, 6 and 7. All of these patients first underwent EDUS then later had CTs confirming the presence of stonesconsiderably proximal to the UVJ. We believe that this particular finding has not been previously described in the literature.
LIMITATIONS
This report is a case series. All cases were identified retrospectively and some had incompletely filled bladders. Potential stone migration during the interval between US and CT makes exact stone location at the time of US difficult to assess. False positives could theoretically occur with partially filled or inadequately interrogated bladders, adjacent bowel or pelvic masses that may compress the bladder, ureteroceles, bladder malignancy, enlarged prostate, altered anatomy from previous surgery, or normal variance.
CONCLUSION
The bladder bulge is a novel sonographic term that describes focal bladder wall thickening or inward wall protrusion at the level of the UVJ in patients with ureterolithiasis. It may not be unique to impacted UVJ stones. We hypothesize that the bladder bulge is commonly present in patients with renal colic, and sonographic visualization of the bulge in patients with suspected renal colic will increase the likelihood of a ureteral stone being present. If so, this finding has the potential to curtail unnecessary CT, especially when used in the presence of hydronephrosis. Emergency physicians should begin to look for the bladder bulge sign when renal colic is suspected. Further studies need to be done to examine the sensitivity and specificity of the bladder bulge sign, both alone and with hydronephrosis and hematuria; the duration it remains visible after stone passage; the relationship of the sign to the stone location; and the ease or difficulty with which the bladder bulge is obtained at the bedside.
Footnotes
Supervising Section Editor: Rick A McPheeters, DO
Submission history: Submitted February 07, 2012; Revision received April 04, 2012; Accepted April 17, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.11960
Address for Correspondence: Scott Bomann, DO, Wellington Hospital, Department of Emergency Medicine, Wellington Regional Hospital, Wellington New Zealand
Email: sbomann@msn.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Brown J. Diagnostic and treatment patterns for renal colic in U.S. emergency departments. International Urology and Nephrology. 2006;38:87–92. [PubMed]
2. Pearle M, Calhoun E, Curhan G. Urologic diseases in America project: urolithiasis. The Journal of Urology. 2005;173:848–57. [PubMed]
3. Teichman JMH. Clinical practice. Acute renal colic from ureteral calculus. The New England Journal of Medicine. 2004;350:684–93. [PubMed]
4. Pavlica P, Gaudiano C, Barozzi L. Sonography of the bladder. World Journal of Urology.2004;22:328–34. [PubMed]
5. Moş C, Holt G, Iuhasz S, et al. The sensitivity of transabdominal ultrasound in the diagnosis of ureterolithiasis. Medical Ultrasonografie. 2010;12:188–97.
6. Rao A, Yvette K, Chacko N. Tuberculosis of urinary bladder presenting as pseudoureterocele. Indian Journal of Medical Sciences. 2005;59:272–3. [PubMed]
7. Broder J, Bowen J, Lohr J, et al. Cumulative CT exposures in emergency department patients evaluated for suspected renal colic. The Journal of Emergency Medicine.2007;33:161–8. [PubMed]
8. Katz DS, Scheer M, Lumerman JH, et al. Alternative or additional diagnoses on unenhanced helical computed tomography for suspected renal colic: experience with 1000 consecutive examinations. Urology. 2000;56:53–7. [PubMed]
9. Hoppe H, Studer R, Kessler TM, et al. Alternate or additional findings to stone disease on unenhanced computerized tomography for acute flank pain can impact management.The Journal of Urology. 2006;175:1725–30. [PubMed]
10. Brenner D, Hall E. Computed tomography–an increasing source of radiation exposure.The New England Journal of Medicine. 2007;357:2277–84. [PubMed]
11. Smith Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Archives of Internal Medicine. 2009;169:2078–86. [PubMed]
12. Lee C, Haims A, Monico E, et al. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231:393–8. [PubMed]
13. Turk C, Knoll T, Petrik A, et al. Guidelines on urolithiasis. European Association of Urology. Available at: http://www.uroweb.org/guidelines/online-guidelines2011. Accessed January 14, 2012.
14. Gaspari RJ, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Academic Emergency Medicine. 2005;12:1180–4. [PubMed]
15. Moak J, Lyons M, Lindsell C. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. The American Journal of Emergency Medicine. 2012;30:218–21.[PubMed]
16. Jung S, Cho J. Congenital anomalies of the upper urinary tract. In: Kim S, editor.Radiology Illustrated: Uroradiology. 2nd ed. London, New York: Springer Heidelberg Dortdrecht; 2012. p. 58.
17. Andersson KE. Urinary bladder contraction and relaxation: physiology and pathophysiology. Physiological reviews. 2004;84:935. [PubMed]