| Author | Affiliation |
|---|---|
| Nicholas E Kman, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| Aaron W Bernard, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| Daniel R Martin, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| David Bahner, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| Diane Gorgas, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| Rollin Nagel, PhD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
| Sorabh Khandelwal, MD | Ohio State University College of Medicine, Department of Emergency Medicine, Columbus, Ohio |
ABSTRACT
Introduction:
Emergency medicine (EM) is a young specialty and only recently has a recommended medical student curriculum been developed. Currently, many schools do not require students to complete a mandatory clerkship in EM, and if one is required, it is typically an overview of the specialty. We developed a 10-month longitudinal elective to teach subject matter and skills in EM to fourth-year medical students interested in the specialty. Our goal was producing EM residents with the knowledge and skills to excel at the onset of their residency. We hoped to prove that students participating in this rigorous 10-month longitudinal EM elective would feel well prepared for residency.
Methods:
We developed a 10-month longitudinal elective to teach subject matter and skills in EM to fourth-year medical students interested in the specialty. Our goal was producing EM residents with the knowledge and skills to excel at the onset of their residency. We hoped to prove that students participating in this rigorous 10-month longitudinal EM elective would feel well prepared for residency.
Results:
Graduates of this elective have reported feeling well prepared to start residency. The resident-led teaching shifts, Advanced Pediatric Life Support certification, Grand Rounds presentations, Advanced Cardiovascular Life Support proficiency testing, and ultrasound component, were found to be beneficial by all students.
Conclusion:
Our faculty believes that participating students will be better prepared for an EM residency than those students just completing a 1-month clerkship. Our data, although limited, lead us to believe that a longitudinal, immersion-type experience assists fourth-year medical students in preparation for residency.
INTRODUCTION
The constant upward trajectory of medical school education favors the use of specialized training before residency.1 Fourth-year honors electives give students a chance to push beyond the limits of standard medical education. As a young specialty, only recently has emergency medicine (EM) had a national voice for undergraduate education and with that a recommended curriculum for medical students.2,3 The EM clerkship offered at most medical schools is an overview of the specialty designed for students of all skill levels and career aspirations.
Medical student educators are challenged with the task of creating ways to improve upon the educational opportunities available to future EM residents. In the Society of Academic Emergency Medicine’s Medical Student Educator’s Handbook, Pacella4 offers many ideas to improve upon the traditional 1-month EM clerkship offered to many students. She explores the concept of a month-long EM elective, along with discussing toxicology, pediatric EM, and emergency medical service (EMS) opportunities. Recently, 23% of EM clerkship directors reported that their respective program offered an advanced EM experience such as a subinternship, advanced EM elective, or career tract.5Despite this response, no published curriculum exists explicitly for students wishing to enter an EM residency.
The fourth-year clerkship in EM provides a broad overview of the specialty, yet the specifics of EM typically cannot be experienced in 1 month. The reality is that most new EM interns have not had continued involvement with their specialty since the beginning of the fourth year. Thus, our faculty hoped to provide these students with a year-long, comprehensive EM experience to better prepare them for the start of their residency. In addition, we wanted to evaluate the students’ perceptions of how this curriculum prepared them for residency.
This educational resource provides a curriculum for clerkship directors and educators hoping to provide their students with additional skills to succeed in residency. Herein, EM educators will find objectives and educational strategies designed to help the most dedicated students further their understanding of EM. The course summary presented is intended to be modified and adapted for use in academic or community medical centers to fit the needs of the organizing faculty members.
DEVELOPMENT OF THE PROGRAM
In the past several years, the structure of the fourth year of medical school has been a topic of debate. At most medical schools, the fourth year consists of a few “required” rotations and several elective months. Secondary to the lack of a specialty-specific curriculum, most residency directors are likely to agree that students leave medical school with a “generalist” education, but they still require supplemental education to ensure competence in their specialty.1 Recently, fiscal pressure on postgraduate training has increased the importance of teaching and skills assessment in medical school, which was previously taught in residency.1 It is now becoming apparent that training for the basic skills necessary to practice medicine will shift from postgraduate training programs to the undergraduate arena.
We designed a 10-month longitudinal elective, Advanced Topics in Emergency Medicine (ATEM), which would expose the fourth-year student to EM throughout the year. This will allow these students to continue to take electives necessary for their broad development while still allowing for specialty-specific training.
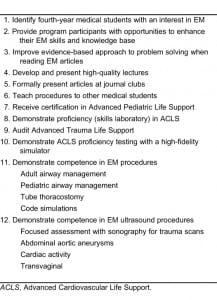
The chief objective of this program was to identify fourth-year medical students with an interest in EM and provide them with opportunities to enhance their skills and knowledge base. By the end of the elective, all participants were expected to fulfill the objectives listed in Table 1.
EDUCATIONAL STRATEGIES AND COURSE COMPONENTS
Clinical and Didactic Teaching
Resident-Led Teaching Shifts
This unique clinical opportunity provides benefit to both senior residents interested in teaching and to students enrolled in the elective. It is well known that residents can play an important role in medical student education. Mitchell and Pacella6describe residents as teachers of bedside medicine, role models, and advisors to students during the application process. Vertical teaching is encouraged throughout the ATEM curriculum. Vertical teaching is the concept of educators from various levels in a given discipline who work cooperatively to help students acquire the academic skills necessary for success. In this aspect of the longitudinal elective, we as faculty, used the help of senior residents who were interested in becoming more proficient teachers.
Case-based clinical teaching can be extremely effective as a bedside teaching tool.7,8 Ismach9reports that bedside, patient-centered teaching offers the best opportunities for evidence-based medicine. During a teaching shift, residents actively sought cases of high educational value. Teaching residents were solely responsible for teaching, mentorship, guidance, and evaluation.
Evidence-Based Medicine Journal Club
Evidence-based medicine (EBM) is essential to the practice of any good emergency clinician. Journal club provides a monthly lesson on literature review and evaluation. Journal club occurred in 2 ways at our institution. We previously had the students attend all residency journal clubs. However, as their numbers grew from 7 enrollees to 28 (in 2010), we now have a monthly journal club with the students presenting to the residents, and faculty as their audience. They are required to present an article at 2 journal clubs, using a strict EBM template. For the presentation that occurs at the residency journal club, they work with a senior resident in critiquing the article assigned to them. This offers another vertical teaching opportunity for both students and residents.
Enhancement of Student Teaching and Presentation Skills
EMS Lectures
Students were required to develop and teach at least 1 lecture for EMS continuing education. Lectures were prepared with the approval and guidance of our EMS director and given to local EMS providers.
Grand Rounds Presentation
Students were required to prepare 1 lecture for a Grand Rounds presentation. Topics are chosen from the teaching shifts that the students complete with senior residents. Students were paired with an attending physician who has an area of interest in the topic presented. The content and quality of the lecture is expected to be on par with the expectations of EM residents.
Leadership Training
Leadership Journal Club and Didactics
To help facilitate leadership growth, we provide students with a journal club on leadership, facilitated by academic leaders in our department. The focus of this journal club is to provide insights and a road map on increasing one’s leadership abilities. The leadership aspect of the course consists of a leadership-style assessment, conflict resolution, stress management, the art of negotiation, interpersonal skills, procedural teaching, interview skills, and tools for motivation.10 We focus our teaching on 4 skills thought to be crucial to success: communication, leadership, self-motivation, and management.11
Panel Discussion for Medical Students
ATEM students arrange a panel discussion for junior students interested in EM to prepare them for their rotations and future careers as emergency physicians. Topics covered by the panel discussion include preclinical years, maximizing the third and fourth year of medical school, acing your clerkship, residency selection, and interview tips.
Procedural Training
Airway Management
Students rotate with a pediatric and adult anesthesiologist in the operating room (OR) with the goal of completing as many intubations as possible. Students supplemented their OR experience with assigned readings as well as practice in the simulation center.
Clinical Skills Scenarios/Small-Group Topic Discussions
Small-group sessions allow attending physicians to teach students by using interactive discussion, lecture, and case-based presentations.8
Ultrasonography
Students were required to record and independently perform 15 abdominal aortic scans, 15 focused assessment with sonography for trauma (FAST) scans, and 15 scans for cardiac activity. Students typically obtained scans by a combination of emergency department patients and models. Performance of 15 transvaginal pelvic studies is also encouraged through use of simulators, live models, or real patients. The goal is to compile a digital portfolio of ultrasound activity for students to present to their respective residency programs.
Advanced Trauma Life Support Exposure
Students were required to audit the Advanced Trauma Life Support (ATLS) course. Although the American College of Surgeons dictates that medical students cannot hold a certification in ATLS, the experience of auditing the course gives students a stronger knowledge base for decision making in trauma scenarios and also enables the students to transition into a teaching role for ATLS sooner in their residencies.
Advanced Pediatric Life Support Certification
All students were required to become certified in Advanced Pediatric Life Support (APLS). Having an early view of advanced pediatric life support is invaluable for the student’s academic development.
Operating Room Procedural Experience
Students worked with a cardiothoracic surgeon in the operating room setting to become comfortable with tube thoracostomy. Students were required to successfully and independently place 2 chest tubes under supervision in the OR setting.
Simulation
ATEM stresses critical care as 1 of its clinical components. ATEM students help teach ACLS codes to third-year medical students on the iSTAN high-fidelity simulator (METI Learning, Sarasota, Florida) in addition to working to become more comfortable in handling ACLS and trauma resuscitations. Students are tested in ACLS and are expected to be competent before graduation. Students were expected to teach 1 procedure during a third year–required procedural course. They were encouraged to become an expert on the procedure while being able to teach the procedure, the indications, the contraindications, the complications, and alternate methods.
High-Acuity Patient Observation.
Students were expected to spend time in the hospital and respond to code blue situations, trauma pages, and anesthesiology pages. The overnight pager component is now offered as an elective in the curriculum, secondarily to inconsistency with experience.
COST AND IMPLEMENTATION
ATEM has been successful at our institution. As a longitudinal elective, the student receives credit for 1 elective month, but the course spans a 10-month period. These electives are becoming popular, as they allow students to be immersed in 1 learning experience for much of the year. Students must complete many of the longitudinal requirements while on elective time or less rigorous months.
We currently have been accepting all students interested in pursuing a career in EM. This year that number has expanded to 28 students. We have decided that going forward we will limit enrollment to 30 to maintain feasibility.
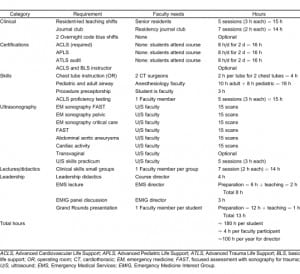
It does take time and money to get the program started (Table 2). The faculty must first agree with the concept and secondly, volunteer their time. The amount of time spent on the course may vary secondarily to the number of faculty participants. At our institution, the course director (N.E.K.) does most of the day-to-day operations. This includes the 2-hour orientation, all the mock ACLS code sessions (6 sessions, 3 hours each), and facilitating the Grand Rounds presentations (3 sessions, 2 hours each) for a total of 26 hours. The course director also attends every ATEM journal club (9 journal clubs, 2 hours each) and gives some of the didactic sessions. As you can see, this does require significant dedication and we would recommend protected time. The requirements for the rest of the faculty are less intensive. We have an ultrasound director (D.B.) who facilitates the ultrasound teaching and most of our other faculty members dedicate themselves to one 2-hour didactic session or journal club. For our faculty, we estimate this is about 1 hour of faculty time per student per year.
The course could be tailored to suit the resources of the implementing institution. For example, helicopter EMS, cadaver laboratories, toxicology, or pediatric EM could all be added on the basis of availability. Our partnership with the Department of Anesthesia has allowed us to send our students to the operating room to work on their adult and pediatric airway skills. The students work closely with a cardiothoracic surgeon who donates time during her cases to instruct our students on chest tube placement. At our institution, the students also spend time in the simulation laboratory, OR suite, emergency department, and with local EMS.
The total cost of the elective at our institution is approximately $4,000 per course per year. This money comes from our education budget from the College of Medicine. For the first 2 years, this worked out to about approximately $270.00 per student. This money is spent primarily on the ATLS class, resident reimbursement (could be gift or pay) for participating in the teaching shifts, and food for the meetings. The budget could be tailored significantly to meet the needs of each institution.
As we have moved forward, interest in the course has increased. At the time of writing (February 10, 2011) we currently have 28 students enrolled in this elective. The budget per student has gone down significantly ($140.00 per student per year) secondarily to increased enrollment. For this reason, we have made changes that are discussed in lessons learned.
EVALUATIONS AND METHODS
Measuring the success of any new curriculum can be a difficult endeavor. Student feedback of this curriculum is important to identify components that are effective and those in need of improvement. Our graduates were expected to complete an Internet-based comprehensive course evaluation at the end of this 10-month elective. Graduates rated each of the course components by using a 5-point Likert format from “strongly disagree” to “strongly agree,” either in terms of whether the component was beneficial to them or whether the course expectations were appropriate, or their perceptions related to the course. Finally, student comments were solicited for each course component. Our survey was based loosely on an evaluation developed by our colleagues in behavioral science.12 We hoped to prove that students participating in this rigorous 10-month longitudinal EM elective would feel well prepared for residency.
Student evaluation results were compiled with descriptive statistics calculated by using SPSS software (Chicago, Illinois).13 The Mann-Whitney U-test was used to compare student ratings of components between years (2007–2008 versus 2008–2009). The Wilcoxon Signed Ranks test was used to compare student ratings between components (across years when available). This study was Institutional Review Board exempt.
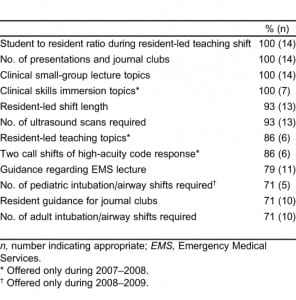
RESULTS
Fourteen students participated in the ATEM elective during our study period, 7 in 2007–2008 and 7 in 2008–2009. All of the graduates provided evaluation feedback for the various components of the course. Comparisons of student ratings between the 2 implementation years indicated only 1 difference: in 2007–2008 residents were perceived as more prepared to teach during the resident-led teaching shifts (z = 2.57, P < 0.02). Because there were no other rating differences between years, the ratings were combined across the 2 implementation years when available. The “strongly agree” and “agree” ratings were combined for summaries of the course component evaluations by using the percentage of respondents indicating whether the components were beneficial to them (Table 3), whether the course expectations were appropriate (Table 4), or their perceptions related to the course (Table 5). Most course components were rated as beneficial by students. The resident-led teaching shifts, APLS certification, Grand Rounds presentation, ACLS proficiency testing, and ultrasound components were universally viewed as beneficial by all students surveyed (100% of students ranked these highly beneficial). The monthly journal club and small-group lectures were also perceived as beneficial.
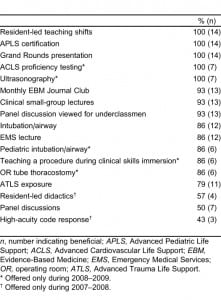
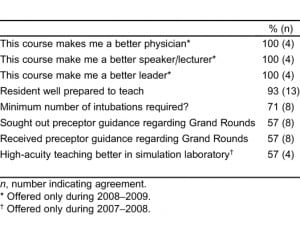
For the students who completed the elective in its first year in existence (2007–2008), the high-acuity code response and resident-led didactics were rated significantly lower (P < 0.05) than course components such as resident-led teaching shifts and the EMS lecture. Also, only 4 of 7 students indicated that the high-acuity teaching would be better if presented in the simulation laboratory. The panel discussion and ATLS exposure were also not as well rated by the students surveyed but have been retained in the curriculum.
DISCUSSION
Most course components for the ATEM, an honors elective in EM, were perceived as beneficial by the students. The resident-led teaching shifts, APLS certification, Grand Rounds presentation, ACLS proficiency testing, and ultrasound components were universally viewed as beneficial by all students surveyed (100% of students agreed). The monthly EBM Journal Club and small-group lectures were also evaluated highly.
Realizing the importance of mentorship and vertical teaching, we used the help of interested residents to lead “teaching shifts” with the students. The students enjoyed seeing patients in the ED with a dedicated teacher and none of the pressures of patient flow. In the Grand Rounds presentation, students are required to prepare 1 lecture on an interesting case or topic from 1 of the teaching shifts that the students complete with senior residents. Students also perceived this portion of the course as beneficial. In another example of resident and faculty teaching, the students were invited to attend all residency journal clubs. For their presentations, students worked with a senior resident and faculty member in critiquing the article assigned to them. Students reported that this experience was highly beneficial.
Students are required to record and independently perform abdominal aortic scans, FAST scans, and scans for cardiac activity. Students typically obtain scans by a combination of emergency department patients and models. Performance of transvaginal pelvic studies was encouraged through use of simulators, live models, or real patients. The ultimate goal is to compile a digital portfolio of ultrasound activity for students to present to respective residency programs as proof of experience.
LESSONS LEARNED AND LIMITATIONS
Lessons that we have learned during the implementation phase have led to improvements in the ATEM curriculum. For example, the students who completed the elective in its first year in existence (2007–2008) reported that the high-acuity code response and resident-led didactics were not as beneficial and have since been dropped from the course. We did this to improve the course to provide maximum benefit for students. The high-acuity code response was an experience designed for students to respond to actual trauma and medical codes. Unfortunately, this experience was inconsistent. Some students would get to help run a code overnight and some would not. For this reason, it currently exists as an optional experience.
The resident-led didactics were initially viewed by the course creators as an opportunity for students to have non-EM residents discuss EM implications from their specialty. Senior residents from various specialties helped generate discussion and learning for the classroom didactic series that met bimonthly. We encouraged students rotating on a service other than EM to become experts in the emergencies for that specialty. Unfortunately, arranging this experience was inconsistent and it was therefore dropped from the course.
The panel discussion and ATLS exposure were also not highly rated by the students surveyed. We believe that the panel discussion is an integral part of the course, not just for the experience it provides the ATEM students, but for the learning it provides underclassmen. Indeed, this was very highly regarded by the first-, second-, and third-year students who attended this discussion.
Finally, the ATLS experience was not viewed by the students as being as beneficial to them, as they have to audit the course and cannot become certified. This has been dropped from the course in lieu of a trauma simulation day. This simulation day is led by 1 of the authors (N.E.K.), who is a certified ATLS instructor, and includes a mix of lectures and simulation practice. At the conclusion of the day, students are required to pass a mega code. The other benefit to these changes is that the cost of ATLS was $125 per student per class. This has allowed us to accommodate more students while still maintaining our budget.
This study of the course is limited by its data and lack of a control group. Most students going into EM at our institution participate in this elective. The first and second year there were only 2 students from our institution who did not complete ATEM. Unfortunately, to prove that this course makes better residents, we would have to study ATEM graduates versus other graduates from our institution who go into EM but do not take the course. This is a very small number each year (less than 2 students/class). This is why we did not make this a comparison study.
FUTURE DIRECTIONS
During the course of the year, we seek the feedback of our students in order to make curriculum enhancements. This year we added a longitudinal project. This can be research, quality assurance, or curricular improvement.
Last year, we added professionalism to the curriculum. This aspect of the course will consist of dealing with difficult patients, dealing with consultants, the “problem resident,” and communication skills.
Our faculty believes that the dedicated students who complete this rigorous elective will be excellent residents in their respective programs. The initial impact of this elective may be recognized soon after our graduates arrive in their respective residency. As in other specialties, EM residency directors have specific expectations of their prospective residents. Their ability to complete specific skills upon arrival is expected, while other skills are anticipated to be learned during the course of the intern year.1 As Langdale et al1 concluded, “medical schools should consider the expectations of their students’ future residency directors when developing new curricula.” We agree with their sentiments and plan to evaluate our graduates’ residency preparation by sending a survey to the residency directors of the programs that matched our graduates. In addition, we plan to collect self-evaluations of the ATEM graduates to assess its impact on their preparation for residency as well as their participation in fellowships, academic positions, or leadership positions through postgraduation surveys.14
Most recently, we have started a mentorship program whereby students participating in ATEM mentor students from the Emergency Medicine Interest Group program. We currently have 115 students signed up for this “Tiered Mentorship Program in EM.” We hope to present this mentorship program as a future curricular advance.
CONCLUSION
We are now entering the fourth year for this longitudinal elective that serves to prepare EM candidates for residency. Survey data and anecdotal reports from students who completed the course in the first 2 years of its existence indicated the students felt better equipped for a residency in EM. Our data, although limited, leads us to believe that a longitudinal, immersion-type experience assists fourth-year medical students in preparation for residency.
Footnotes
Supervising Section Editor: Michael Epter, DO
Submission history: Submitted September 17, 2010; Revision received December 23, 2010; Accepted February 24, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.2.2095
Address for Correspondence: Nicholas E. Kman, MD
Ohio State University, Department of Emergency Medicine, 4813 Cramblett Hall, 456 W 10th Ave, Columbus, OH 43210
E-mail: nicholas.kman@osumc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Langdale LA, Schaad D, Wipf J, et al. Preparing graduates for the first year of residency: are medical schools meeting the need? Acad Med. 2003;;78:39–44. [PubMed]
2. Manthey DE, Coates WC, Ander DS, et al. Report of the task force on national fourth year medical student emergency medicine curriculum guide. Acad Emeg Med. 2006;;47:e1–e7.
3. Wald DA, Manthey DE, Lin MA, et al. Clerkship directors in EM: a statement of purpose. Acad Emerg Med. 2008;15:856–859. [PubMed]
4. Pacella CB. Advanced opportunities for student education in EM: SAEM Medical Student Educators’ Handbook. Society for Academic Emergency Medicine Web site. Available at:www.saem.org. Accessed July 9, 2007.
5. Wald DA, Manthey DE, Kruss L, et al. The state of the clerkship: a survey of EM clerkship directors.Acad Emerg Med. 2007;;14:629–634. [PubMed]
6. Mitchell E, Pacella CB. EM resident role in student education: SAEM Medical Student Educators’ Handbook. Society for Academic Emergency Medicine Web site; 2007. Available at: www.saem.org. Accessed July 9.
7. SAEM Undergraduate Education Committee. Teaching techniques in the clinical setting: “the emergency medicine perspective”—SAEM Medical Student Educators’ Handbook. Society for Academic Emergency Medicine Web site; 2007. Available at: www.saem.org. Accessed July 11.
8. Ander DS. Teaching in the classroom: teaching didactic material: SAEM Medical Student Educators’ Handbook. Society for Academic Emergency Medicine Web site; 2007. Available at:www.saem.org. Accessed July 9.
9. Ismach R. Teaching evidence based medicine to medical students: SAEM Medical Student Educators’ Handbook. Society for Academic Emergency Medicine Web site; 2007. Available at:www.saem.org. Accessed July 11.
10. Williams SJ. What skills do physician leaders need now and in the future? Physician Exec.2001;;27:46–48. [PubMed]
11. Gustafson RP, Schlosser JR. Who will lead? Physician Exec. 1997;;23:37–40. [PubMed]
12. Post DM, Stone LC, Knutson DJ, et al. Enhancing behavioral science education at the Ohio State University College of Medicine. Acad Med. 2008;;83:28–36. [PubMed]
13. SPSS Inc. Emergency Medicine Residency Review Committee: program requirements for residency training in emergency medicine. Accreditation Council for Graduate Medical Education Web site; 2007. Available at:http://www.acgme.org/acWebsite/downloads/RRC_progReq/110pr905.pdf. Accessed July 11.
14. Harris R, Kinsinger LS, Tolleson-Rinehart S, et al. The MD-MPH Program at the University of North Carolina at Chapel Hill. Acad Med. 2008;;83:371–377. [PubMed]


