| Author | Affiliation |
|---|---|
| Kris Chiles, MD | Alameda County Medical Center, Department of Emergency Medicine, Oakland, CA |
| Arun Nagdev, MD | Alameda County Medical Center, Department of Emergency Medicine, Oakland, CA |
ABSTRACT
This report highlights the importance of using bedside ultrasound in the emergency department to confirm guide-wire placement when performing central venous catheter placement prior to dilating and cannulating the vessel.
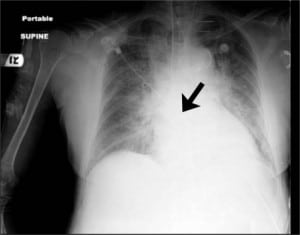
A 73-year-old female was brought to the emergency department for altered level of consciousness. Her blood pressure was 81/50 mmHg, which did not respond to fluid hydration. The right internal jugular (IJ) vein was cannulated with ultrasound guidance for vasoactive administration. A flash-back of dark non-pulsatile blood was obtained before vessel dilation and catheter placement. A portable chest radiograph was performed and read by the staff radiologist as “left IJ catheter is seen overlying the mediastinum likely within the left innominate vein” (Figure 1). Prior to the use of the catheter, the nursing team noted abnormal pulsations from the distal port of central venous catheter (CVC), prompting a bedside ultrasound by the clinician to ensure proper placement (Figure 2). Differentiation of the carotid artery and IJ vein was difficult secondary to the patient’s severe volume depletion, but doppler showed pulsatile flow in the cannulated vessel confirming inadvertent arterial placement.
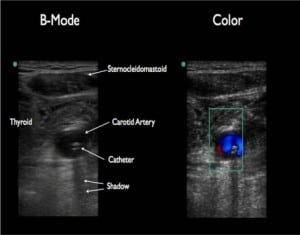
This report highlights the use of using ultrasound to confirm proper placement of a central venous catheters. The IJ vein overlies the carotid artery, making chest radiograph an unreliable test to ensure venous placement. Central venous pressure (CVP) monitoring can confirm venous cannulation, but can be difficult to obtain in many emergency departments. Classic teaching of looking for dark non-pulsatile blood can be inaccurate in hypotensive and hypoxic patients. Also when a collapsible vein overlies the carotid artery, a through puncture can occur.1 A prior study demonstrated the use of guidewire visualization with bedside ultrasound as a useful technique to confirm venous placement prior to dilation.2 We feel that with the fair amount of literature demonstrating improved safety of ultrasound-guidance in CVC, confirming venous placement of either the guidewire or catheter can be a simple addition in hypotensive patients or those that uncertainty exists regarding arterial cannulation.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted: August 18, 2010; Accepted September 13, 2010.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Dr. Kris Chiles, MD, Department of Emergency Medicine, Alameda County Medical Center, 1411 East 31st Street, Oakland, CA 94602
Email chiles.kris@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Blaivas M. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med.2009;37(8)
2. Stone M. Ultrasound detection of guidewire position during central venous catheterization. AM J Emerg Med. 2009;27(4):516. [PubMed]


