| Author | Affiliation |
| Ling Tiah, MBBS, MPH | Changi General Hospital, Accident and Emergency Department, Singapore |
| Kentaro Kajino, MD, PhD | Ministry of Health, Labour and Welfare, Government of Japan, Department of Acute Medicine & Critical Care Medical Center, Osaka National Hospital, Osaka, Japan |
| Omer Alsakaf, MD | Dubai Corporate for Ambulance Services, Dubai, United Arab Emirates |
| Dianne Carrol Tan Bautista, PhD | Duke-NUS Graduate Medical School, Center for Quantitative Medicine, Singapore |
| Marcus Eng Hock Ong, MBBS, MPH | Duke-NUS Graduate Medical School, Health Services and Systems Research, Singapore; Singapore General Hospital, Department of Emergency Medicine, Singapore |
| Desiree Lie, MD, MS.ED | Duke-NUS Graduate Medical School, Office of Clinical Sciences, Singapore |
| Ghulam Yasin Naroo, MBBS | Rashid Hospital, Department of Health & Medical Services, ED-Trauma centre, Dubai, United Arab Emirates |
| Nausheen Edwin Doctor, MBBS | Singapore General Hospital, Department of Emergency Medicine, Singapore |
| Michael YC Chia, MBBS | Emergency Department,Tan Tock Seng Hospital, Singapore |
| Han Nee Gan, MBBS | Changi General Hospital, Accident and Emergency Department, Singapore |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Endotracheal intubation (ETI) is currently considered superior to supraglottic airway devices (SGA) for survival and other outcomes among adults with non-traumatic out-of-hospital cardiac arrest (OHCA). We aimed to determine if the research supports this conclusion by conducting a systematic review.
Methods
We searched the MEDLINE, Scopus and CINAHL databases for studies published between January 1, 1980, and 30 April 30, 2013, which compared pre-hospital use of ETI with SGA for outcomes of return of spontaneous circulation (ROSC); survival to hospital admission; survival to hospital discharge; and favorable neurological or functional status. We selected studies using pre-specified criteria. Included studies were independently screened for quality using the Newcastle-Ottawa scale. We did not pool results because of study variability. Study outcomes were extracted and results presented as summed odds ratios with 95% CI.
Results
We identified five eligible studies: one quasi-randomized controlled trial and four cohort studies, involving 303,348 patients in total. Only three of the five studies reported a higher proportion of ROSC with ETI versus SGA with no difference reported in the remaining two. None found significant differences between ETI and SGA for survival to hospital admission or discharge. One study reported better functional status at discharge for ETI versus SGA. Two studies reported no significant difference for favorable neurological status between ETI and SGA.
Conclusion
Current evidence does not conclusively support the superiority of ETI over SGA for multiple outcomes among adults with OHCA.
INTRODUCTION
Timely establishment of a patent airway with adequate ventilation has long been regarded as a primary objective in the management of non-traumatic out-of-hospital cardiac arrest (OHCA). Advanced airway intervention by emergency medical services (EMS) personnel was first introduced in the 1970s as a superior alternative to basic airway control such as bag-mask-valve ventilation for pre-hospital resuscitation.1-3
Endotracheal intubation (ETI), the standard for securing a definitive airway in in-hospital resuscitation, has since gained widespread support as one of the advanced airway modalities for OHCA patients. Over the past four decades, EMS personnel in various parts of the world have been increasingly trained and certified to perform pre-hospital ETI as part of advanced cardiac life support care.1,4,5 Advocates maintain that with comprehensive and continuous training, ETI by field EMS personnel is safe and may be associated with improved outcomes in selected patient groups.6-9 Others remain concerned about the use of ETI in relatively unskilled hands in pre-hospital settings where infrequent exposure and limited experience may potentially lead to prolonged attempts, unrecognized complications and compromised patient care.10-12
Supraglottic airway devices (SGA) are inserted without laryngoscopy and provide ventilation by delivering oxygen above the level of glottic opening. As such, they are an attractive alternative to ETI due to their relative ease of insertion, better skill retention by users and comparable ventilation adequacy.13-16 The different types and models of SGA have evolved considerably over the years. Earlier generations, such as the esophageal obturator airway, the esophageal gastric tube airway and the pharyngeal tracheal lumen airway, have largely been abandoned due to questionable efficacy and associated serious complications.13,17-20 Nonetheless, there are still challenges associated with other SGA available for use by EMS personnel, such as esophageal perforations, tracheal injury and insufficient protection against pulmonary aspiration.21-24
Despite decades of advanced airway intervention by EMS in the field, there remains a lack of high-quality evidence supporting the use of ETI over SGA. The scarcity of true randomized controlled trials in this area reflects underlying ethical concerns and logistical challenges. Recent literature reviews suggest a need to re-evaluate the presumed benefits of pre-hospital ETI for selected study populations such as those with major trauma and pediatric patients.3,25-27 The objective of this systematic review is to determine whether ETI compared to SGA is associated with improved survival and other outcomes among adults with non-traumatic OHCA. We hypothesized that among these patients, ETI is superior to SGA for survival and other outcomes.
METHODS
Search Strategy
Three authors (KK, OA, TL) conducted a search of the MEDLINE, Scopus and CINAHL databases for eligible studies published in English between January 1, 1980, and April 30, 2013. The search strategy used relevant keywords as Medical Subject Headings terms in MEDLINE; and free-text words in the other two databases in the following combinations: (intubation or endotracheal or intratracheal or supraglottic or laryngeal mask or combitube or esophageal tracheal or esophageal tracheal) and [(out-of-hospital or pre-hospital) and (cardiac arrest or heart arrest)] and (emergency medical services or paramedic). Filters were applied to include only human studies and to exclude studies involving only children.
For the purpose of this review, we defined ETI as the placement of a secured cuffed tube in the trachea. SGA in this review refer to devices currently in use by most EMS systems, such as the laryngeal mask airway, the laryngeal tube and the esophageal-tracheal Combitube.13,28,29 We excluded use of now- obsolete, earlier generation devices.26
Study Eligibility Criteria and Data Extraction
We included randomized controlled trials and cohort studies with patient outcomes comparing the use of ETI and SGA in pre-hospital settings. We excluded studies that provided a comparison of either ETI with bag-valve-mask ventilation only or SGA with bag-valve-mask ventilation only. We also excluded reviews of studies, editorials and other papers without patient data.
We restricted our review to studies that involved adults 18 years or older with non-traumatic OHCA. We excluded studies with undifferentiated study populations of adults and pediatric patients (younger than 18 years) and those with undifferentiated causes of OHCA. EMS personnel involved in the advanced airway management could be physicians, nurses, paramedics, emergency medical technicians or basic-level emergency medical technicians. Studies that involved military medical and evacuation services were excluded.
Studies had to provide at least one of the following patient-based outcomes: (1) return of spontaneous circulation (ROSC), defined as the presence of a palpable pulse without cardiopulmonary resuscitation, which could be specified to be before or upon arrival in the emergency department or unspecified; (2) survival to hospital admission to an inpatient ward; (3) survival to hospital discharge, regardless of the length of hospital stay; and (4) favorable neurological or functional outcome with the use of validated measures, such as the Cerebral Performance Category Score, the Modified Rankin Scale or the Health Utilities Index.30-32 We excluded studies that reported only non-patient-centered outcome measures relating to personnel ease of use, device complications or effectiveness of ventilation in terms of biochemical or physiological markers.
Three authors (KK, OA, TL) screened titles and abstracts of studies generated from the search (KK, OA, TL). Full text articles were next obtained for studies eligible for inclusion. Only studies meeting the inclusion and exclusion criteria were then selected for final quality review.
Two reviewers (GHN, TL) then independently reviewed the included studies for assessment of methodological quality. None of the included studies were randomized trials, so we chose the Newcastle-Ottawa Scale (NOS) for rating study quality.33,34 The NOS assigns a minimum of zero and a maximum of four stars for three criteria (patient selection, comparability and outcome) based on a total of eight questions. The stars were then tallied to provide four categories of study quality (poor = 0 to 3 stars; fair = 4 to 5 stars; good = 6 to 7 stars and excellent = 8 to 9 stars).
We extracted information about study design, participants, sample size, airway modalities investigated (ETI versus SGA), patient outcome measures, key findings and authors’ conclusions or recommendations and collated it into a descriptive summary table. The results were not pooled into a meta-analysis because of variation across EMS systems among the included studies. Instead, two authors (DB, TL) extracted data pertaining to the effect size of respective outcome measures from each study (where provided or available). If the adjusted analysis was not available, we calculated the unadjusted odds ratios (OR) with 95% CI based on number of events in respective outcome measures for ETI versus SGA (if reported).
RESULTS
Search Results
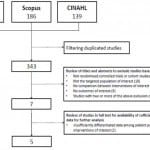
The electronic search yielded 490 studies of which 147 were duplicates (Figure 1), leaving 343 studies for title and abstract review. After title and abstract review, seven were found to meet eligibility criteria. After reviewing their full texts, two of the studies were further excluded. One study included patients aged 15 years and above with no further differentiation of its study population into adults and pediatric patients (younger than 18 years).35 The other study included patients of all ages receiving either ETI or laryngeal mask airway (LMA), similarly with no further subgroup analysis differentiated by adult and pediatric (younger than 18 years) population.36 Five studies were eventually included in the final analysis.
Figure 1. Search and selection process for comparison of endotracheal intubation (ETI) and supraglottic airways (SGA) patient outcomes, 2011 and 2013 updated search results.
CINAHL, Cumulative Index to Nursing and Allied Health Literature
Characteristics of Included Studies
The five included studies (Table 1) involved a total of 303,348 non-traumatic OHCA adult patients receiving pre-hospital advanced airway management in the form of either ETI or SGA. Mean patient age ranged from 55 years to 75 years; and two thirds of patients were male. Study size ranged from 172 to 281,522 patients and study duration from 12 months to eight years.
Table 1. Included studies comparing endotracheal intubation (ETI) with supraglottic airways (SGA): Summary of study characteristics.
EMS, emergency medical services; ETI, endotracheal intubation; ROSC, return of spontaneous circulation; SGA, supraglottic airways
*Although the original article compared bag-valve-mask ventilation with advanced airway management as a group, there were adequate differentiated information to allow comparison of outcomes between ETI and SGA.
One study was quasi-randomized,37 another was a secondary analysis of another study;38 and the remaining were prospective39,40 and retrospective41 cohort studies. Two studies were conducted in North America, two in Japan and one in Austria. Only one study had experienced physicians as part of their EMS teams, while the rest had paramedics and emergency medical technicians. Among the five studies, two compared ETI with esophageal-tracheal Combitube only (an SGA device) while the other three compared ETI with SGA as a combined group without differentiating among the particular SGA devices.
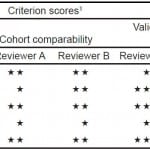
The quality of the studies was good to excellent (Table 2). Agreement for quality score was 100% between the two reviewers (GHN, TL).
Table 2. Summary of criterion scores and overall methodological quality (reviewers A and B) for five included studies comparing endotracheal intubation (ETI) and supraglottic airways (SGA) outcomes based on the Newcastle-Ottawa Scale (NOS) scores.
1. Star (*) indicates the score given to study according to the NOS quality assessment scale, with more stars reflecting better quality.
2. Determined by the total number of stars assigned to study: 0-3 Stars = Poor; 4-5 Stars = Fair; 6-7 Stars = Good; 8-9 Stars = Excellent
Comparison of Outcome Measures
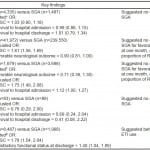
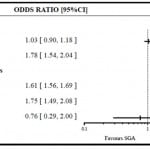
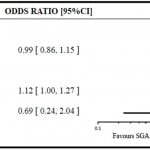
The results of the respective included studies were summarized in Table 3. All five studies addressed ROSC as one of the outcome measures, either as adjusted or unadjusted analysis, with varying results. Cady et al.41 and Rabitsch et al.37 compared the association of ROSC with ETI versus esophageal-tracheal Combitube (i.e. SGA) use and found no significant difference, with OR=1.03 (95% CI 0.90–1.18) and OR=0.76 (95% CI 0.29–2.00) respectively. The other three studies compared ETI with SGA and found a benefit in favor of ETI with higher proportion of ROSC associated with ETI use. The ORs were 1.61 (95% CI 1.56–1.69),39 1.75 (95% CI 1.49–2.08)40 and 1.78 (95% CI 1.54–2.04)38 (Figure 2a).
Table 3. Adjusted and unadjusted odds ratio (OR) comparing endotracheal intubation (ETI) and supraglottic airways (SGA) for outcome measures.
ETI, endotracheal intubation; OR, odds ratio; ROSC; return of spontaneous circulation; SGA, supraglottic airways
*Adjusted for: age, gender, bystander-witnessed arrest, bystander cardiopulmonary resuscitation (CPR), bystander use of automated external defibrillator and initial cardiac rhythm.
†Adjusted for: age, gender, bystander CPR, initial cardiac rhythm, duration of resuscitation, location of arrest, status of Emergency Life-Saving Technicians, epinephrine use and etiology.
‡Adjusted for: age, gender, bystander or emergency medical services witnessed arrest, bystander CPR, initial cardiac rhythm, trial site and trial arm of primary study.
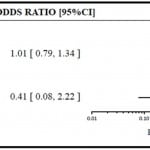
Survival to hospital admission was analyzed in three studies and all three suggested no significant difference in this outcome between ETI and SGA use. The ORs were 0.99 (95% CI 0.86–1.15)41, 1.12 (95% CI 1.00–1.27)40 and 0.69 (95% CI 0.24–2.04)37 (Figure 2b). Similarly, for the outcome of survival to hospital discharge, two studies comparing ETI with esophageal-tracheal Combitube (i.e. SGA) found no difference, with OR=1.01 (95% CI 0.79–1.34) by Cady et al.41 and OR=0.41 (95% CI 0.08–2.22) by Rabitsch et al.37 (Figure 2c).
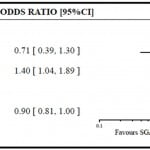
Three of the five studies evaluated neurological outcome or functional status as the primary outcome (Figure 2d). Kajino et al.40 compared the neurological status based on the Cerebral Performance Category Score for those treated with ETI versus SGA and the adjusted OR was 0.71 (95% CI 0.39–1.30) suggesting no significant difference between the two.40 In an unadjusted analysis of results from Hasegawa et al., there was also no significant difference in the neurological status based on the Cerebral Performance Category Score between patients who received ETI versus SGA, with OR=0.90 (95% CI 0.81–1.00).39 In both studies, however, the direction of results seemed to favor SGA. In the secondary analysis of the Resuscitation Outcomes Consortium Prehospital Resuscitation using an Impedance valve and an early versus delayed study by Wang et al., patients who received ETI compared with SGA were more likely to have satisfactory functional status based on the Modified Rankin Scale at discharge, with OR=1.40 (95% CI 1.04–1.89).38
Figure 2a. Associations of pre-hospital advanced airways [endotracheal intubation (ETI) versus supraglottic airways (SGA)] with return of spontaneous circulation.
Figure 2b. Associations of pre-hospital advanced airways [endotracheal intubation (ETI) versus supraglottic airways (SGA)] with survival to hospital admission.
Figure 2c. Associations of pre-hospital advanced airways [endotracheal intubations (ETI) versus supraglottic airways (SGA)] with survival to hospital discharge.
Figure 2d. Associations of pre-hospital advanced airways [endotracheal intubations (ETI) versus supraglottic airways (SGA)] with favorable neurological or functional outcome.
DISCUSSION
We conducted a systematic review to examine our initial hypothesis that ETI was superior to SGA for survival and other patient outcomes among adults with non-traumatic OHCA. The results of the review, however, do not conclusively support this hypothesis. There were no significant differences between ETI and SGA in terms of survival to hospital admission and survival to hospital discharge among the studies that analyzed these two outcomes.37,40,41 In terms of ROSC, there were conflicting results. Wang et al.,38 Hasegawa et al.39 and Kajino et al.40 suggested a benefit in favor of ETI with a higher proportion of ROSC associated with ETI use while Rabitsch et al.37 and Cady et al.41 suggested no difference between ETI and SGA.
For neurological or functional status, Hasegawa et al.39 and Kajino et al.40 found no significant difference between ETI and SGA for favorable neurological outcome at one month. Both the studies by Hasegawa et al. and Kajino et al. drew from the same country database with overlapping study periods and similar methodology. Hasegawa et al.39 was comparing bag-valve-mask ventilation with advanced airway management at a national level while Kajino et al.40 was specifically comparing ETI with SGA in one prefecture in Japan. Therefore, it was probable that the population enrolled by Kajino et al. was a subset of the population analyzed by Hasegawa et al. With the largest cohort comprising almost 90% of patients in this review and a sound methodology, the study by Hasegawa et al. could make for a compelling case against the superiority of ETI over SGA in terms of neurological outcome.39 Although it was an unadjusted analysis, the finding was congruent with the adjusted comparison between ETI and SGA for neurological status by Kajino et al.40 The study by Wang et al., involving EMS teams affiliated with universities and medical institutes across the United States of America and Canada, suggested otherwise.38 There was a higher proportion of satisfactory functional status at discharge among patients with ETI use based on an adjusted analysis, possibly supporting the hypothesis for superiority of ETI over SGA for this outcome in their study population. However, as the authors themselves had highlighted, this was a secondary analysis of another trial that had not been designed to compare advanced airway management.38 As such, their findings would have to be interpreted within the appropriate context and limitations.
Overall, there was no consistent trend demonstrating superiority of ETI over SGA for the five outcomes examined. Our finding is similar to other related studies and reviews examining the perceived benefits of pre-hospital ETI compared with alternative airway modalities among various study populations.27,42-44 Thus, the intended impact on relevant patient outcomes with ETI use in the field is still not convincingly demonstrated.3
The lack of a consistent positive association between ETI use and favorable patient outcomes when compared with SGA has been attributed to several factors. One is the relative complexity of the procedure itself. EMS personnel need to attain and maintain a certain level of competency to perform successful ETI.26,39 In addition, potential complications and pitfalls associated with ETI could negatively impact patient outcomes, such as esophageal tube placement, main bronchial intubation or barotrauma.45-47 Failure to gain mastery of the required skills and inability to address related complications or errors could offset the potential benefits of pre-hospital ETI use when compared with the lower skill requirements and lower complication rate of SGA.
The inconclusive evidence surrounding the role of pre-hospital ETI for OHCA has prompted calls for randomized controlled trials to optimally evaluate the hypothesized causal relationship between ETI use and survival outcomes.38-40 The potential value of such studies notwithstanding, it should be emphasized that the utility of ETI would be most relevant to the context in which it is being studied. Given the inherent differences in organizational structure, resources and geographical coverage of EMS systems in different regions and countries, the impact of ETI use in one system may not be reproducible in another system that is run and staffed differently.8,48-51 Even within the same EMS system, it may be prudent to identify certain selected groups of patients for whom ETI may be beneficial.39 As Eich et al.48 had responded to a comment about pre-hospital pediatric ETI use, perhaps the “question is not if but rather when, where and by whom.”
LIMITATIONS
Firstly, there were no true randomized controlled trials that fulfilled our inclusion criteria for this review. Instead, our search resulted in a small selection of quasi-randomized and observational studies, deemed to be relatively weaker in the hierarchy of evidence. Secondly, we considered the decision to use the NOS for methodological assessment of the included studies, which was based on its relevance to cohort studies and its simplicity in application. A comprehensive review by Deeks et al.33 evaluated the suitability of available tools for assessing non-randomized studies and found the NOS to be among those appropriate for use in terms of the domains covered but cautioned the lack of information about its reliability and validity. Therefore, although the overall methodological quality of included studies was deemed to be mostly “excellent” based on the NOS, results from these studies should be interpreted with appropriate caution. The concern about the inter-rater reliability between reviewers using the NOS has also been raised by others and highlighted the need for other alternatives.52,53 To address this concern, we evaluated the inter-rater agreement between the two independent reviewers and it was found to be high. While ongoing work is being done to further refine and develop better instruments for the assessment of non-randomized trials, the NOS remains listed as one of the useful tools in the last updated version of the Cochrane Handbook.54 Lastly, because we excluded studies with undifferentiated study population of adults and pediatric patients (younger than 18 years), our review is potentially missing the subgroup data from those studies. There were two such studies. One included patients aged 15 years or older and had about 138,000 cases.35 However, this study population was extracted from the same nationwide database with similar eligibility criteria over a period captured by Hasegawa et al., which was included in our review.39 The other study included patients of all ages with 641 of them receiving either ETI or LMA and our review might have missed some of them because of the exclusion criteria.36
CONCLUSION
The evidence presented in our review does not conclusively support the current practice assumption that pre-hospital ETI use, compared to SGA, improves survival among adult patients with non-traumatic OHCA. This concurs with other related work in the literature examining the benefits of ETI use in the field among various patient populations.
Footnotes
Supervising Section Editor: David Peak, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Tiah Ling, Accident and Emergency Department, Changi General Hospital Singapore, 2 Simei Street 3. Singapore, 529889. Email: ling_tiah@cgh.com.sg.
Submission history: Submitted November 13, 2013; Revision received September 4, 2014; Accepted July 31,2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- Pepe PE, Copass MK, Joyce TH. Prehospital endotracheal intubation: rationale for training emergency medical personnel. Ann Emerg Med. 1985;14:1085-92.
- Rumball CJ, MacDonald D. The PTL, Combitube, laryngeal mask, and oral airway: a randomized prehospital comparative study of ventilatory device effectiveness and cost-effectiveness in 470 cases of cardiorespiratory arrest. Prehosp Emerg Care. 1997;1:1-10.
- Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann of Emerg Med. 2006;47:532-41.
- Cummins RO. The ”chain of survival” concept: how it can save lives. Heart Dis Stroke. 1992;1:43-5.
- Iwami T, Nichol G, Hiraide A, et al. Continuous improvements in ”chain of survival” increased survival after out-of-hospital cardiac arrests: a large-scale population-based study. Circulation. 2009;119:728-34.
- Jacobs LM, Berrizbeitia LD, Bennett B, et al . Endotracheal intubation in the prehospital phase of emergency medical care. JAMA. 1983;250:2175-7.
- Sirbaugh PE, Pepe PE, Shook JE, et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest. Ann Emerg Med. 1999;33:174-84.
- Thomas JB, Abo BN, Wang HE. Paramedic perceptions of challenges in out-of-hospital endotracheal intubation. Prehosp Emerg Care. 2007;11:219-23.
- Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592-7.
- Deakin CD, King P, Thompson F. Prehospital advanced airway management by ambulance technicians and paramedics: is clinical practice sufficient to maintain skills? Emerg Med J. 2009;26:888-91.
- Nolan JD. Prehospital and resuscitative airway care: should the gold standard be reassessed? Curr Opin Crit Care. 2001;7:413-21.
- Wang HE, Kupas DF, Greenwood MJ, et al. An algorithmic approach to prehospital airway management. Prehosp Emerg Care. 2005;9:145-55.
- Lefrancois DP, Dufour DG. Use of the esophageal tracheal combitube by basic emergency medical technicians. Resuscitation. 2002;52:77-83.
- Reinhart DJ, Simmons G. Comparison of placement of the laryngeal mask airway with endotracheal tube by paramedics and respiratory therapists. Ann Emerg Med. 1994;24:260-3.
- Schofferman J, Oill P, Lewis AJ. The esophageal obturator airway. A clinical evaluation. Chest. 1976;69:67-71.
- Tanigawa K, Shigematsu A. Choice of airway devices for 12,020 cases of nontraumatic cardiac arrest in Japan. Prehosp Emerg Care. 1998;2:96-100.
- Auerbach PS, Geehr EC. Inadequate oxygenation and ventilation using the esophageal gastric tube airway in the prehospital setting. JAMA. 1983;250:3067-71.
- McCabe CJ, Browne BJ. Esophageal obturator airway, ET tube, and pharyngeal-tracheal lumen airway. Am J Emerg Med. 1986;4:64-71.
- Pons PT. Esophageal obturator airway. Emerg Med Clin North Am. 1988;6:693-8.
- Smith JP, Bodai BI, Seifkin A, et al. The esophageal obturator airway. A review. JAMA. 1983;250:1081-4.
- Agro F, Frass M, Benumof JL, et al. Current status of the Combitube: a review of the literature. J Clin Anesth. 2002;14:307-14.
- Asai T, Shingu K. The laryngeal tube. Br J Anaesth. 2005;95:729-36.
- Benumof JL. Laryngeal mask airway. Indications and contraindications. Anesthesiology. 1992;77:843-6.
- Vezina MC, Trepanier CA, Nicole PC, et al. Complications associated with the Esophageal-Tracheal Combitube in the pre-hospital setting. Can J Anaesth. 2007;54:124-8.
- Bukur M, Kurtovic S, Berry C, et al. Pre-hospital intubation is associated with increased mortality after traumatic brain injury. J surg Res. 2011;170:e117-21.
- Jensen JL, Cheung, KW, Tallon JM, et al. Comparison of tracheal intubation and alternative airway techniques performd in the prehospital setting by paramedics: a systematic review. CJEM. 2010;12:135-40.
- Lecky F, Bryden D, Little R, et al. Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev. 2008:CD001429.
- Wiese CH, Semmel T, Muller JU, et al. The use of the laryngeal tube disposable (LT-D) by paramedics during out-of-hospital resuscitation-an observational study concerning ERC guidelines 2005. Resuscitation. 2009;80:194-8.
- Yanagawa Y, Sakamoto T. Analysis of prehospital care for cardiac arrest in an urban setting in Japan. J Emerg Med. 2010;38:340-5.
- Raina KD, Callaway C, Rittenberger JC, Holm MB. Neurological and functional status following cardiac arrest: method and tool utility. Resuscitation. 2008;79:249-56.
- Rittenberger JC, Raina K, Holm MB, et al. Association between Cerebral Performance Category, Modified Rankin Scale, and discharge disposition after cardiac arrest. Resuscitation. 2011;82:1036-40.
- Stiell IG, Nesbitt LP, Nichol G, et al. Comparison of the Cerebral Performance Category score and the Health Utilities Index for survivors of cardiac arrest. Ann Emerg Med. 2009;53:241-8.
- Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Asses. 2003;7:iii-x, 1-173.
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp, Accessed April 2, 2012.
- Tanabe S, Ogawa T, Akahane M, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J of Emerg Med. 2013;44:389-97.
- Shin SD, Ahn KO, Song KJ, et al. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83:313-9.
- Rabitsch W, Schellongowski P, Staudinger T, et al. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Resuscitation. 2003;57:27-32.
- Wang HE, Szydlo D, Stouffer JA, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation. 2012;83:1061-6.
- Hasegawa K, Hiraide A, Chang Y, et al. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309:257-66.
- Kajino K, Iwami T, Kitamura T, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care. 2011;15:R236.
- Cady CE, Weaver MD, Pirrallo RG, et al. Effect of emergency medical technician-placed Combitubes on outcomes after out-of-hospital cardiopulmonary arrest. Prehosp Emerg Care. 2009;13:495-9.
- Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783-90.
- Stockinger ZT, McSwain NE, Jr. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56:531-6.
- Takei Y, Enami M, Yachida T, et al. Tracheal intubation by paramedics under limited indication criteria may improve the short-term outcome of out-of-hospital cardiac arrests with noncardiac origin. J Anesth. 2010;24:716-25.
- Dunford JV, Davis DP, Ochs M, et al. Incidence of transient hypoxia and pulse rate reactivity during paramedic rapid sequence intubation. Ann Emerg Med. 2003;42:721-8.
- Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32-7.
- von Goedecke A, Herff H, Paal P, et al. Field airway management disasters. Anesth Analg. 2007;104:481-3.
- Eich C, Roessler M, Nemeth M, et al. Characteristics and outcome of prehospital paediatric tracheal intubation attended by anaesthesia-trained emergency physicians. Resuscitation. 2009;80:1371-7.
- Lossius HM, Sollid SJ, Rehn M, et al. Revisiting the value of pre-hospital tracheal intubation: an all time systematic literature review extracting the Utstein airway core variables. Crit Care. 2011;15:R26.
- Martinon C, Duracher C, Blanot S, et al. Paediatric prehospital tracheal intubation: What makes different our practice across the Ocean? Resuscitation. 2010;81:634; author reply -5.
- Thomas MJ, Benger J. Prehospital intubation in cardiac arrest: the debate continues. Resuscitation. 2011;82:367-8.
- Hartling L, Hamm M, Milne A, et al. Validity and Inter-Rater Reliability Testing of Quality Assessment Instruments. Rockville, MD: Agency for Healthcare Research and Quality; 2012.
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-5.
- Reeves BC, Deeks JJ, Higgins, JPT, et al. Chapter 13: Including non-randomized studies. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. Available at: www.cochrane-handbook.org.