| Author | Affiliation |
|---|---|
| Wesley Eilbert, MD | University of Illinois at Chicago, Department of Emergency Medicine, Chicago, Illinois |
| Benjamin Hecht, DO | University of Illinois at Chicago, Department of Emergency Medicine, Chicago, Illinois |
| Loren Zuiderveld, MD | Advocate Illinois Masonic Medical Center, Chicago, Illinois |
Introduction
Case report
Discussion
ABSTRACT
Mesenteric venous thrombosis is a rare cause of abdominal pain, which if left untreated may result in bowel infarction, peritonitis and death. The majority of patients with this illness have a recognizable, predisposing prothrombotic condition. Oral contraceptives have been identified as a predisposing factor for mesenteric venous thrombosis in reproductive-aged women. In the last fifteen years new methods of hormonal birth control have been introduced, including a transdermal patch and an intravaginal ring. In this report, we describe a case of mesenteric venous thrombosis in a young woman caused by a vaginal contraceptive ring.
INTRODUCTION
Mesenteric venous thrombosis (MVT) is a well-described cause of intestinal ischemia, accounting for approximately 15% of all mesenteric ischemia cases.1 It is distinctly different from mesenteric arterial occlusion. A rare condition, MVT accounts for only 0.002% to 0.06% of all inpatient admissions and 0.01% of all emergency surgical admissions.2 Given its nonspecific initial symptoms, MVT is not an easy diagnosis to make. Patients often complain of vague abdominal pain and nausea for days to weeks before seeking medical attention.1,3
An etiologic factor causing a prothrombotic state can be found in approximately three-quarters of patients with MVT, with inherited or acquired disorders of coagulation, cancer, intra-abdominal inflammatory conditions, the postoperative state and portal hypertension being the most commonly reported causes.4 MVT can occur at any age, but is more common in the sixth and seventh decades of life.1 Oral contraceptive use accounts for 9% to 18% of the episodes of MVT in young women.4 In this case we describe a patient who developed MVT from the use of a vaginal contraceptive ring (NuvaRing ®).
CASE REPORT
A previously healthy 18-year-old woman presented to our emergency department (ED) with 5 days of worsening intermittent periumbilical, epigastric and right upper quadrant (RUQ) abdominal pain. She had nausea with the pain, though no vomiting or fever. The pain was crampy in nature and not exacerbated by eating. She was sexually active with one partner and had used the NuvaRing as contraception for the previous two years. She smoked approximately 5 cigarettes per day and denied any family history of coagulation disorders. On physical examination she was afebrile, with tenderness in the periumbilical, epigastric and right upper quadrant (RUQ) areas of her abdomen. She had no rigidity, guarding, or other peritoneal signs.
Laboratory examinations sent from the ED included: a complete blood count, renal profile including electrolytes, liver function tests, serum lipase, urinalysis and a urine pregnancy test. The only abnormality noted was a mildly elevated serum alanine-amino transferase (ALT) level of 46 IU/L. A RUQ ultrasound of the abdomen was ordered to evaluate for cholelithiasis. While no abnormalities of the biliary tract were seen, splenomegaly was noted as an incidental finding. Because of the patient’s ongoing and unexplained pain, a computerized tomographic (CT) scan with intravenous (IV) contrast of the abdomen and pelvis was performed. A large superior mesenteric vein thrombosis was identified with enlargement of the liver and spleen.
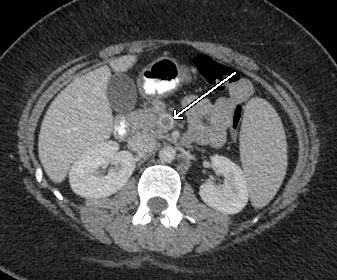
Figure
Computed tomography of the abdomen showing a large filling defect in the superior mesenteric vein (arrow) indicating the presence of thrombus.
The patient was anticoagulated with IV heparin and admitted to the hospital with surgical and hematologic consultants. The NuvaRing was removed at the time of admission. Evaluations for prothrombotic conditions including: protein C, protein S and antithrombin III deficiency; factor V, prothrombin and MTHFR gene mutation; lupus anticoagulant, cardiolipin IgA and IgG antibodies were all negative. The patient’s hospital course progressed without complication as she was bridged to anticoagulation with warfarin sodium, and she was discharged on day 5 with instructions to refrain from using hormonal birth control in the future.
DISCUSSION
Mesenteric venous thrombosis was first recognized as a distinct clinical entity by Warren and Eberhard in 1935.5 The superior mesenteric vein is involved the majority of the time, with inferior mesenteric vein thrombosis representing only 0% to 11% of cases.6 Several predisposing factors have been identified for the development of MVT (Table).1,2,4,6 Impairment of venous return from the bowel by MVT results in venous engorgement and eventually ischemia. Unlike mesenteric arterial occlusion, the transition from normal to ischemic bowel is typically gradual with MVT. In those cases with rapid and complete occlusion of mesenteric veins, there is insufficient time for development of collateral circulation and transmural bowel infarction may occur.
Table. Reported predisposing conditions for mesenteric vein thrombosis.
| Predisposing conditions |
|---|
| Prothrombotic states |
| Protein C or S deficiency |
| Factor V Leiden deficiency |
| Antithrombin III deficiency |
| Prothrombin gene mutation G20210A |
| Hyperhomocysteinemia |
| Antiphospholipid antibodies |
| Polycythemia vera |
| Nephrotic syndrome |
| Essential thrombocythemia |
| Paroxysmal nocturnal hemoglobinuria |
| Pregnancy |
| Oral contraceptive use |
| Malignancy |
| Intra-abdominal causes |
| Cirrhosis and portal hypertension |
| Inflammatory bowel disease |
| Intra-abdominal infection |
| Pancreatitis |
| Intra-abdominal surgery |
| Other causes |
| Blunt abdominal trauma |
| Congestive heart failure |
Abdominal pain and anorexia are the most consistent symptoms of MVT, though patients often complain of other nonspecific symptoms such as diarrhea, nausea and vomiting.3,7 Seventy-five percent of patients are symptomatic for more than 48 hours at time of presentation, with the mean duration of symptoms varying from 6 to 14 days.6 The pain associated with MVT is classically described as a colicky, mid-abdominal pain which, early on, is out of proportion to the abdominal findings on physical exam. Approximately one-third of patients will have blood noted on rectal exam.3 Those patients with transmural bowel infarction will have physical findings consistent with peritonitis.
Routine laboratory evaluations are rarely helpful in the diagnosis of MVT, though lactic acidosis is a late finding and predicts a poor outcome.6 Recent improvements in imaging techniques have allowed for earlier diagnosis and treatment of MVT.8 CT with IV contrast is the current diagnostic test of choice for MVT with an accuracy of approximately 90%.2,4,6,9–11 Magnetic resonance angiography has also been found to have excellent sensitivity and specificity.8,12 Doppler ultrasound is of limited value in the evaluation for MVT due to operator dependency and its inability to image vascular anatomy in the presence of overlying bowel gas.12
Immediate anticoagulation with heparin is the standard initial treatment of MVT, with the presence of gastrointestinal bleeding rarely a contraindication to its use.2,4,6,11 Transcatheter thrombolytic therapy and thrombectomy have both been used with success in small case series.13,14 Those patients with signs of peritonitis require emergent resection of the infarcted bowel. Mortality rates with MVT range from 11% to 33% in the most recently published studies.8,15,16
MVT associated with hormonal contraception was first described in 1963, three years after the approval of the first oral contraceptive pill in the United States (U.S.).17 Since then, several other cases have been reported.18 Since 2002, a contraceptive transdermal patch (Ortho Evra ®) and a contraceptive vaginal ring (NuvaRing) have been available in the U.S., each offering some advantages over oral contraceptives. A study conducted by the U.S. Food and Drug Administration concluded the transdermal patch and the vaginal ring were associated with an increased risk of venous thromboembolism similar to that of oral contraceptives.19 Other reported thrombotic complications of the vaginal contraceptive ring have included cerebral venous sinus thrombosis, axillary vein thrombosis and aortic thrombosis.20–23 We are aware of only one other reported case of MVT associated with a vaginal contraceptive ring, this having been reported in the hematology literature.24
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Author, Titles, Address. Email: Wesley Eilbert, MD. Department of Emergency Medicine, University of Illinois, College of Medicine, 1819 West Polk St. CME Rm 469, Chicago, IL 60612. 7 / 2014; 15:395 – 397
Submission history: Revision received January 28, 2014; Submitted April 13, 2014; Accepted April 29, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Abdu RA, Zakhour BJ, Dallis DJ Mesenteric venous thrombosis – 1911 to 1984. Surgery. 1987; 101:383-88
2 Harnik IG, Brandt LJ Mesenteric venous thrombosis. Vasc Med. 2010; 15:407-18
3 Rhee RY, Gloviczki P, Mendonca CT Mesenteric venous thrombosis: still a lethal disease in the 1990s. J Vasc Surg. 1994; 20:688-97
4 Kumar S, Sarr MG, Kamath PS Mesenteric venous thrombosis. N Engl J Med. 2001; 345:1683-88
5 Warren S, Eberhard TP Mesenteric venous thrombosis. Surg Gynecol Obstet. 1935; 61:102-21
6 Singla AK, Kamath PS, Tefferi A Mesenteric venous thrombosis. Mayo Clin Proc. 2013; 88:285-94
7 Harward TRS, Green D, Bergan JJ Mesenteric venous thrombosis. J Vasc Surg. 1989; 9:328-33
8 Zhang J, Duan ZQ, Song QB Acute mesenteric venous thrombosis: a better outcome achieved through improved imaging and a changed policy of clinical management. Eur J Endovasc. 2004; 28:329-34
9 Grisham A, Lohr J, Guenther JM Deciphering mesenteric thrombosis: imaging and treatment. Vasc Endovasc Surg. 2005; 39:473-9
10 Acosta S, Alhadad A, Ekberg O Findings in multi-detector row CT with portal phase enhancement in patients with mesenteric venous thrombosis. Emerg Radiol. 2009; 16:477-82
11 Rhee RY, Gloviczki P Mesenteric venous thrombosis. Surg Clin North Am. 1997; 77:327-38
12 Bradbury MS, Kavanaugh PV, Bechtold RE Mesenteric venous thrombosis: diagnosis and noninvasive imaging. Radiographics. 2002; 22:527-41
13 Hollingshead M, Burke CT, Mauro MA Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005; 16:651-61
14 Kim HS, Patra A, Khan J Transhepatic catheter-directed thrombectomy and thrombolysis of acute superior mesenteric venous thrombosis. J Vasc Interv Radiol. 2005; 16:1685-91
15 Brunaud L, Antunes L, Collinet-Adler Acute mesenteric venous thrombosis: case for nonoperative management. J Vasc Surg. 2001; 34:673-9
16 Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M Mesenteric venous thrombosis. Associated systemic disorders and hypercoagulability status of 21 surgical patients. Hepatogastroenterology. 2007; 54:1080-4
17 Reed DL, Coon WW Thromboembolism in patients receiving progestational drugs. N Engl J Med. 1963; 269:622-4
18 Gubitosi A, Docimo G, Avenia N Thrombosis of the superior mesenteric vein in association with hormonal contraceptive use. A case report and review of the literature. Ann Ital Chir. 2011; 82:69-74
19 Ouellet-Hellstrom R, Graham DJ, Staffa JA . Combined hormonal contraceptives and the risk of cardiovascular disease endpoints. ;
20 Dunne C, Malyuk D, Firoz T Cerebral venous sinus thrombosis in a woman using the etonogestrel-ethinyl estradiol vaginal contraceptive ring: a case report. J Obstet Gynaecol Can. 2010; 32:270-3
21 Kolacki C, Rocco V The combined vaginal contraceptive ring, nuvaring, and cerebral venous sinus thrombosis: a case report and review of the literature. J Emerg Med. 2012; 42:413-6
22 Samuelsson E, Hultdin J, Groth K . Lakartidningen. 2007; 104:32-4
23 . Canadian Adverse Drug Reaction Newsletter. 2008; :18
24 Voora D, Vijayan A Mesenteric vein thrombosis associated with intravaginal contraceptives: a case report and review of the literature. J Thromb Thrombolysis. 2003; 15:105-8


