| Author | Affiliation |
|---|---|
| Minal Jain, MBBS, MPH | Department of Neurosurgery, University of Rochester Medical Center, Rochester, New York |
| Dushyant Damania, MBBS | Department of Neurosurgery, University of Rochester Medical Center, Rochester, New York |
| Anunaya R. Jain, MBBS, MCEM | Department of Neurosurgery, University of Rochester Medical Center, Rochester, New York |
| Abhijit R. Kanthala, MD | Department of Neurosurgery, University of Rochester Medical Center, Rochester, New York |
| Latha Ganti, MD, MS, MBA | Departments of Emergency Medicine and Neurological Surgery, University of Florida College of Medicine, Gainesville, Florida |
| Babak S. Jahromi, MD, PhD, FRCSC | Department of Neurosurgery, University of Rochester Medical Center, Rochester, New York |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction: Conflicting data exist regarding the association between the length of stay (LOS) of critically ill patients in the emergency department (ED) and their subsequent outcome. However, such patients are an overall heterogeneous group, and we therefore sought to study the association between EDLOS and outcomes in a specific subgroup of critically ill patients, namely those with acute ischemic stroke/transient ischemic attack (AIS/TIA).
Methods: This was a retrospective review of adult patients with a discharge diagnosis of AIS/TIA presenting to an ED between July 2009 and February 2010. We collected demographics, EDLOS, arrival stroke severity (National Institutes of Health Stroke Scale – NIHSS), intravenous tissue plasminogen activator (IV tPA) use, functional outcome at discharge, discharge destination and hospital-LOS. We analyzed relationship between EDLOS, outcomes and discharge destination after controlling for confounders.
Results: 190 patients were included in the cohort. Median EDLOS was 332 minutes (Inter-Quartile Range -IQR: 250.3–557.8). There was a significant inverse linear association between EDLOS and hospital-LOS (p=0.049). Patients who received IV tPA had a shorter median EDLOS (238 minutes, IQR: 194–299) than patients who did not (median: 387 minutes, IQR: 285–588 minutes; p<0.0001). There was no significant association between EDLOS and poor outcome (p=0.40), discharge destination (p=0.20), or death (p=0.44). This remained true even after controlling for IV tPA use, NIHSS and hospital-LOS; and did not change even when analysis was restricted to AIS patients alone.
Conclusion: There was no significant association between prolonged EDLOS and outcome for AIS/TIA patients at our institution. We therefore suggest that EDLOS alone is an insufficient indicator of stroke care in the ED, and that the ED can provide appropriate acute care for AIS/TIA patients. [West J Emerg Med. 2014;15(3):267–275.]
INTRODUCTION
Acute ischemic stroke (AIS) is a clinical emergency that requires immediate and aggressive treatment, from prompt identification of symptoms in the emergency department (ED) through rapid investigations and treatment to hospital discharge. Bench-marked timelines have been mandated for every step in the process,1 leading to the creation of Primary Stroke Centers to standardize care delivery. In particular, as per the recommendations of the National Institute of Neurological Disorders and Stroke (NINDS) guidelines, transferring a stroke patient to an inpatient setting should be achieved within 3 hours of arrival.2 However, the limited availability of inpatient beds often results in access block, leading to an increase in the ED length of stay (EDLOS) for patients with stroke and transient ischemic attack (TIA).3–5 Studies have reported the median EDLOS for stroke patients to be approximately 5 hours.6,7 This can place an additional stress on the already overburdened ED, requiring personnel to not only provide emergent care but also devote time and resources for ongoing supportive care to stroke patients before transitioning to other areas of care within the hospital.
Numerous studies have evaluated the effects of prolonged LOS on the outcome of critically ill patients, with conflicting results.6,8–11 Rincon et al.6 reported that critically ill stroke subjects waiting to be transitioned to intensive care unit (ICU) had a worse outcome when the EDLOS was > 5 hrs. Contrary to this, Saukkonen and his colleagues in a similar study with a diverse population of 1,675 critically ill patients concluded that mortality rate for patients with EDLOS beyond 24 hours was not significantly different than those with a shorter EDLOS.10 Elmer et al7 found no association between EDLOS and functional outcome in patients with hemorrhagic stroke. However, the effect of EDLOS on outcome of patients with ischemic stroke or TIA (representing more than 85% of stroke patients)12 remains largely unexamined.
Rapid patient transfer from ED is believed to prevent crowding, provide more streamlined care to the patients, and promote efficient hospital operation and improved patient satisfaction.13 However, early discharge/transfer from the ED on the assumption that a prolonged LOS worsens outcome/mortality could promote inappropriately early transfers before the patient is stabilized and/or the recipient patient care unit is ready. Time criteria (such as that proposed by the NINDS) may be difficult to meet in busy tertiary care hospitals. Such perceived time pressures among providers can also lead to increased patient and family anxiety during this process.
Our aim in this study was to evaluate the effect of EDLOS on outcomes for patients presenting with AIS/TIA at our tertiary care academic center, after adjusting for common confounders such as initial stroke severity (National Institutes of Health Stroke Scale – NIHSS) and delivery of time-sensitive intravenous tissue plasminogen activator (IV tPA).
METHODS
Study Design and Data Sources
This was an institutional review board-approved retrospective record review of consecutive adult stroke/TIA patients presenting to our tertiary care center from July 2009 to February 2010. Our institution is a large academic primary stroke care center in upstate New York, with an annual turnover of nearly 600 acute ischemic stroke/TIA patients. Of these, approximately, half of them per year present within 12 hours of symptom onset. A flow chart is presented in Figure 1. Our protocol for management of AIS/TIA patients includes investigations (blood glucose, serum electrolytes, ECG, cardiac ischemia markers, PT, INR, aPTT, oxygen saturation) along with multi-modal CT imaging (plain CT, CT angiography & perfusion CT imaging). We reviewed medical records to identify all adult patients (>18 years age) with a final discharge diagnosis of AIS/TIA who presented within 12 hours since last seen normal and had documented completion of per-protocol multimodal CT, initial stroke severity, time of ED registration, and time of departure from the ED. We collected data on patient demographics, time since last seen normal, EDLOS, initial stroke severity (NIHSS), past medical history, hospital LOS, functional outcome as measured by modified Rankin scale (mRS) at discharge, discharge destination [home, home with services, skilled nursing facility (SNF), or acute rehabilitation unit (ARU)] and mortality at discharge. The EDLOS was documented from time of registration (time of arrival at ED) to time of departure from the ED. Functional outcome at discharge was dichotomized and mRS ≥3 was considered as poor outcome. To improve uniformity of the cohort under investigation, we excluded from this study pediatric patients, patients with hemorrhagic strokes, and patients who did not receive all protocol mandated investigations or imaging studies.
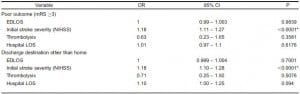
Figure 1. Flow chart indicating the final cohort of patients. This flow chart indicates that our hospital managed about 380 acute ischemic stroke (AIS) or transient ischemic stroke (TIA) patients from July 2009 to February 2010, of which 55% presented within 12 hours of symptom onset. Of these 209 patients, 19 (9%) patients were ineligible as they were either in hospital admissions/ did not have emergency department length of stay documented, leaving a final cohort of 190 patients).
Data Collection
To improve accuracy and reduce errors/inconsistencies in abstracted data, we followed the guidelines stated by Lowenstein et al.14 during data collection process. All records were reviewed by a trained ED physician and a research fellow. Variables were explicitly defined and data was extracted from a standardized electronic medical record system. We resolved any discrepancy in the data by a common consensus between the abstractors. We calculated modified Rankin score at discharge based on occupational therapy and physical therapy notes. Inter-rater agreement was assessed for this parameter by having a sample of charts independently reviewed by the 2 data abstractors. Data was collected in MS Excel, then re-reviewed and cleaned before transfer into JMP statistical software by SAS Institute, Inc, for further analysis.
Statistical Analysis
We reported median and inter-quartile range (IQR) of continuous variables. We performed a bivariate Spearman’s Rank correlation between EDLOS and age, time since last seen normal, initial stroke severity and hospital LOS. Spearman’s ρ, 95% CI (Fisher’s Z transformed) and p values were calculated for each correlation. We performed Wilcoxon/Kruskal Wallis tests to compare the association between EDLOS and administration of IV tPA and past history of comorbidities. A logistic fit was done to test the association between increasing EDLOS and poor outcome (mRS ≥3), death at discharge, discharge to SNF/death/ARU, and the association between hospital LOS and outcome. Finally, we performed a logistic regression to analyze the association between EDLOS on outcome, and discharge destination, after controlling for administration of IV tPA, initial stroke severity and hospital LOS. This was done because high initial stroke severity, non-thrombolysis and prolonged hospital LOS are usually associated with poor outcome.15–18 We repeated the above analysis for a sub cohort with only AIS patients, excluding patients with a final discharge diagnosis of TIA.
We performed all contingency analysis and multivariate analysis using JMP 9.0® and SAS 9.2® statistical software. The level of significant association was predetermined at p<0.05 for all analyses.
RESULTS
Patient Demographics
A total of 209 patients were eligible for this study. Complete data were available for 190 (91%) of these patients (Figure 1). Of these, 138 (72.6%) patients had a discharge diagnosis of AIS and the remaining 52 (27.4%) had a discharge diagnosis of TIA. The characteristics of patients are described in Table 1.
Table 1. Characteristics of patients presenting with acute ischemic stroke or transient ischemic attack.
AIS, acute ischemic stroke; TIA, transient ischemic attack; IQR, interquartile range; NIHSS, National Institutes of Health stroke scale; ED, emergency department; LOS, length of stay; mRS, modified Rankin score; SNF, skilled nursing facility; ARU, acute rehabilitation unit
EDLOS and Outcome in Patients with AIS or TIA
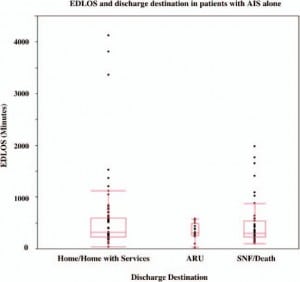
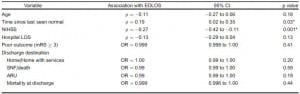
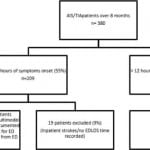
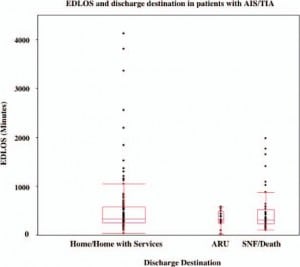
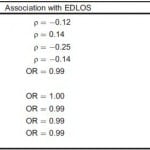
There were no statistically significant associations between EDLOS and age, time since last seen normal, or various stroke risk factors, such as past history of stroke/TIA (p=0.25), CAD (p=0.18), dyslipidemia (p=0.63), hypertension (p=0.85), diabetes mellitus (p=0.22), smoking (p=0.09) or atrial fibrillation (AF) (p=0.19) (Table 2). Lower EDLOS was associated with higher initial stroke severity (p=0.0005) and increased hospital LOS (p=0.0497). There was no significant association between EDLOS and functional outcome/mRS ≥3 (Figure 2) (p=0.40), discharge destination (Figure 3) (SNF/death/ARU, p=0.20) or death at discharge (p=0.44).
Figure 2. Emergency department length of stay and outcome in patients with acute ischemic stroke or transient ischemic attack. There was no significant difference in median emergency department length of stay of patients with poor outcome (modified Rankin score [mRS] ≥ 3) (307.5 min, interquartile range [IQR] 228.3.3–492.3) versus patients with good outcome (337 min, IQR 257.8–577.3; p=0.15).
Figure 3. Emergency department length of stay and discharge destination in patients with acute ischemic stroke (AIS) or transient ischemic attack (TIA). There was no significant association between EDLOS and discharge destination, with median EDLOS (IQR) of 337 (254–574), 312 (253.5–483.3), and 301 (228.3–519.3) minutes for discharge to home/home with services, acute rehabilitation unit (ARU) or skilled nursing facility (SNF)/death, respectively.
mRS, modified Rankin score, SNF, skilled nursing facility, ARU, acute rehabilitation unit, OR, odds ratio, CI, confidence intervals; q, Spearman’s correlation coefficient
*A statistically significant inverse correlation was found between EDLOS and only initial stroke severity (NIHSS) and hospital LOS for patients presenting with AIS or TIA.
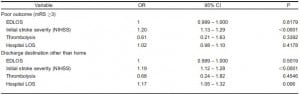
Patients with poor outcome had a significantly longer hospital LOS (median 6 days, IQR 4–9) as compared to those with a good outcome (median hospital LOS 2 days, IQR 1–4 days; p<0.0001). Patients who received IV tPA had a significantly lower median EDLOS (238 minutes, IQR 194 – 299) as compared to patients who did not receive IV tPA (median EDLOS 387 minutes, IQR 285 – 588; p<0.0001).
We performed a logistic regression to assess the effect of EDLOS on outcomes (mRS at discharge ≥3 and discharge destination other than home) after adjusting for the above confounders – IV tPA, initial stroke severity and hospital LOS. This odds ratio and 95% CI are shown in Table 3. After controlling for the above variables, the association between EDLOS and poor outcome (p=0.695), and discharge destination other than home (p=0. 5019) remained statistically insignificant.
mRS, modified Rankin score; NIHSS, National Institutes of Health stroke scale; OR, odds ratio; CI, confidence intervals
EDLOS and Outcome in Patients with AIS Alone
Restricting the analysis to only AIS patients revealed similar results, with no statistically significant associations between EDLOS and age, and stroke risk factors [past history of stroke/TIA (p=0.36), CAD (p=0.44), dyslipidemia (p=0.95), hypertension (p=0.46), diabetes mellitus (p=0.16), smoking (p=0.23) and AF (p=0.28)] (Table 4). There was a significant association between lower EDLOS and higher initial stroke severity (p=0.001). Although the trend between EDLOS and hospital LOS was similar as for all AIS/TIA patients, the association did not remain significant for the AIS-only cohort (p=0.13). There was no association between EDLOS and poor outcome or discharge destination in this more narrowly defined cohort (Figures 4–5). Specifically, we found no statistically significant association between EDLOS and poor outcome (mRS ≥3) (p=0.41), discharge to SNF/ARU/death (p=0.20) or death at discharge (p=0.44) in AIS patients.
Figure 4. Emergency department length of stay and outcome in patients with acute ischemic stroke (AIS) alone. There was no significant difference in median EDLOS of AIS patients with poor outcome (modified Rankin score [mRS] ≥ 3) (309 min, interquartile range [IQR] 229–499) versus patients with good outcome (316 min, IQR 233–592; p=0.38).
Figure 5. Emergency department length of stay (EDLOS) and discharge destination in patients with acute ischemic stroke (AIS) alone. There was no significant association between EDLOS and discharge destination, with median EDLOS (IQR) of 317.5 minutes (229–600.3), 312 minutes (253.5–483.3), and 301 (228.8–535.5) minutes for discharge to home/home with services, acute rehabilitation unit (ARU), or skilled nursing facility (SNF)/death, respectively.
Table 4. Emergency department length of stay and outcome in patients with acute ischemic stroke alone.
NIHSS, National Institutes of Health stroke scale; mRS, modified Rankin score; SNF, skilled nursing facility; ARU, acute rehabilitation unit; OR, odds ratio; CI, confidence intervals; q, Spearman’s correlation coefficient
*Considering the subgroup of patients presenting with AIS alone, a statistically significant inverse correlation was found between EDLOS
and only initial stroke severity (NIHSS).
Patients with a poor outcome had a significantly longer hospital LOS (median 6 days, IQR 4–9) as compared to patients with good outcome (median hospital LOS 3 days, IQR 2–5 days; p<0.0001). In the AIS group, patients who received IV tPA (n=33) had a significantly shorter median EDLOS (238 minutes, IQR 195.5 – 292) as compared to patients who did not receive IV tPA (median EDLOS 399 minutes, IQR 280.5 – 623; p<0.0001).
After adjusting for potential confounders (differences in IV tPA administration rates, initial stroke severity and hospital LOS), we did not find any statistically significant association between EDLOS and poor outcome (p=0.98), or discharge destination other than home (p=0.70) in patients with AIS alone. This is shown in Table 5.
mRS, modified Rankin score, NIHSS, National Institutes of Health stroke scale; SNF, skilled nursing facility, ARU, acute rehabilitation unit; OR, odds ratio; CI, confidence intervals
DISCUSSION
We chose to focus our study on patients with AIS/TIA because of strict guidelines and compliance mandated by the Joint Commission and the State Department of Health for Primary Stroke Centers with respect to this patient population. Our data suggest that there is no significant impact of increased EDLOS on outcome of AIS/TIA patients, even after controlling for presenting stroke severity, IV tPA delivery and total hospital LOS at our tertiary care academic center. In contrast, when examining all stroke subtypes, Rincon et al6 found that of 519 stroke patients, EDLOS adversely affected outcome in 75 patients who were admitted to a neurointensive care unit. Despite adjusting for presenting NIHSS, we did not find this association in our subpopulation of AIS/TIA patients. Our data parallel the findings by Elmer et al,7 which showed no association between EDLOS and functional outcome in patients with hemorrhagic stroke. In a broader population, Varon et al19 studied 50 consecutive patients admitted to ICU from the ED and found similar survival rates in patients who received critical care procedures in the ED versus patients who received similar interventions in an ICU setting.
We found no difference in mortality or discharge destination with respect to EDLOS in our patients. Similarly, Saukkonen et al10 looked at a broader critically ill patient population, including patients with neurological diseases, and reported that EDLOS (>24 hours) was not associated with hospital mortality or quality of life at 6 months post discharge. Using a similar >24 hour cut-off point for EDLOS, a study of 443 critically ill patients in 2001–2002 found that mortality rate for stroke patients was unaffected by EDLOS.11 However, at our institute (and many others in the U.S. today) patient stays in the ED>24 hours are considered as “sentinel events” (only 5.8% subjects in our study population had EDLOS>24 hours), with strict protocols designed to prevent such an occurrence. The results of prior studies may therefore be less applicable in the environment that exists today. Data from our study suggest that even with current protocols mandating early transfer to inpatient units or ICU, increased EDLOS does not affect functional outcomes or mortality in AIS/TIA patients.
With changing Medicare and Medicaid reimbursements, there has been an increasing focus on reduction of overall length of stay in the hospital. Studies have shown that prolonged EDLOS contributes to longer hospital LOS, which is considered a surrogate marker for poor outcome or inefficient care.20 In contrast, we found that a shorter EDLOS at our institution was paradoxically associated with increased hospital LOS, although this may be due to the association between shorter EDLOS and higher initial stroke severity in our cohort. Overall, we found no significant association between EDLOS and poor outcome, suggesting that delivery of care in the ED can be efficient and congruent with the care delivered in subsequent hospital settings for this patient subgroup.
Some authors have explained the association of long EDLOS to poor outcome by linking it to triage preferences, suggesting that patients with good prognosis might be treated, triaged and/or transferred early from the ED at the expense of patients with worse prognosis and/or comfort care order.9 By only analyzing AIS/TIA patients who had uniformly completed all investigations and imaging studies, as well as adjusting for time dependent IV tPA delivery and initial stroke severity, we attempted to avoid such limitations in our analysis.
Out data shows that EDLOS does not affect outcome, but does not indicate why. It is possible that outcome after AIS/TIA is mostly dependent upon factors such as initial stroke severity, thrombolysis and time from onset, none of which are affected by EDLOS. (Thrombolysis usually occurs within the ED setting). Yet even after adjusting for the above factors, there was no significant association between EDLOS and outcome. Differences in EDLOS may reflect practical availability of beds elsewhere in the hospital, and overall minor variations in EDLOS (measured in hours rather than days) may be unlikely to affect the overall outcome of AIS/TIA. This of course assumes that the ED is capable of providing the appropriate acute/critical care needed within the first few hours of AIS/TIA, which we believe holds at most institutions, including our own. The above reasons, while speculative, do call into question the focus on EDLOS as a measure of quality of care, if no direct correlation can be found between EDLOS and eventual patient outcomes.
We emphasize that our study does not provide data regarding the benefits of transferring AIS/TIA patients from ED to higher levels of care, and believe that transferring appropriate patients early helps operational efficiency in the ED by decreasing crowding and resource utilization. We only suggest that focusing on EDLOS as the sole or key indicator of quality of stroke care in the ED may be inaccurate, as increased EDLOS alone does not seem to bear upon outcomes of patients with AIS/TIA.
LIMITATIONS
There were several limitations identified during our study. The primary outcome was mRS at discharge. Some have argued that mRS and death may not be the best outcome measures to study the effect of EDLOS, and have proposed looking at other surrogate markers, such as quality adherence and time to antibiotics, as they are less patient specific.22,23 However, the inability of surrogate markers to produce consistent results is well documented, and we felt it more reasonable to use mRS, which is a routinely used functional outcome score for stroke patients.24,25 In addition to this, we reported outcomes at discharge. While prospective large-scale stroke trials have typically assessed outcome at 3 months, we were unable to do so due to the retrospective nature of our study and the availability of data within the existing records. We hope to address this limitation in a future prospective study.
We were also not able to do a formal power calculation for this study, since this was not a prospective comparison of 2 groups with a pre-specified EDLOS cutoff. Rather, our study retrospectively analyzed patient outcome in relation to EDLOS as a continuous variable, and used multivariate regression to adjust for confounders in this analysis.
Our study was conducted at a single center and the conclusions should be cautiously generalized to other hospitals due to variability in the geographic location, level of care offered, patient management and outcome metrics of other institutes. The study was conducted at a tertiary academic teaching center, which is a certified Primary Stroke Center, with a 24×7 availability of in-house neurologists/neurosurgeons providing immediate care to stroke patients. Thus, there is simultaneous involvement of multiple specialties – ED, Neurology, and Neurosurgery within the ED itself to coordinate and deliver care. This could also limit the generalizability of our results to other institutions without a similar structural and functional setup.
CONCLUSION
Our study concluded that there was no significant association between ED length of stay and mRS, mortality, or discharge destination for acute ischemic stroke or TIA patients presenting to a tertiary care academic ED.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Supervising Section Editor: John Sarko, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem




![Figure 2. Figure 2.Emergency department length of stay and outcome in patients with acute ischemic stroke or transient ischemic attack. There was no significant difference in median emergency department length of stay of patients with poor outcome (modified Rankin score [mRS] ≥ 3) (307.5 min, interquartile range [IQR] 228.3.3–492.3) versus patients with good outcome (337 min, IQR 257.8–577.3; p=0.15). Figure 2. Figure 2.Emergency department length of stay and outcome in patients with acute ischemic stroke or transient ischemic attack. There was no significant difference in median emergency department length of stay of patients with poor outcome (modified Rankin score [mRS] ≥ 3) (307.5 min, interquartile range [IQR] 228.3.3–492.3) versus patients with good outcome (337 min, IQR 257.8–577.3; p=0.15).](https://westjem.com/wp-content/uploads/2014/06/i1936-900X-15-3-267-f02-300x249.jpg)
![Figure 4. Emergency department length of stay and outcome in patients with acute ischemic stroke (AIS) alone. There was no significant difference in median EDLOS of AIS patients with poor outcome (modified Rankin score [mRS] ≥ 3) (309 min, interquartile range [IQR] 229–499) versus patients with good outcome (316 min, IQR 233–592; p=0.38). Figure 4. Emergency department length of stay and outcome in patients with acute ischemic stroke (AIS) alone. There was no significant difference in median EDLOS of AIS patients with poor outcome (modified Rankin score [mRS] ≥ 3) (309 min, interquartile range [IQR] 229–499) versus patients with good outcome (316 min, IQR 233–592; p=0.38).](https://westjem.com/wp-content/uploads/2014/06/i1936-900X-15-3-267-f04-300x264.jpg)