| Author | Affiliation |
|---|---|
| John E. Hipskind, MD | Kaweah Delta Medical Center, Department of Emergency Medicine, Visalia, California |
| Michael D. Burg, MD | Kaweah Delta Medical Center, Department of Emergency Medicine, Visalia, California |
A 77-year-old male presented to our emergency department (ED) with a 3-hour history of acute severe lower abdominal pain, inability to void, a swollen scrotum, and one episode of vomiting. His relevant past medical history included: hypertension, diabetes mellitus, and distant right inguinal hernia repair. Vital signs were: 96.4° F, 101, 22, and 205/90. Examination revealed a normal abdomen and an irreducible left inguinal hernia. Foley catheter placement yielded a scant amount of infected urine that stopped flowing almost immediately and did not resume despite catheter flushing and repositioning. Additional laboratory data did not identify the cause of the patient’s symptoms. An abdominopelvic computed tomography (CT) was performed (Figures 1 and and2)2) after which the patient underwent emergent operative reduction of his incarcerated scrotal cystocele.
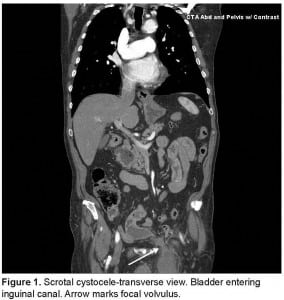
Scrotal cystocele-transverse view. Bladder entering inguinal canal. Arrow marks focal volvulus.
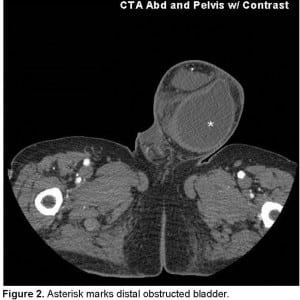
Asterisk marks distal obstructed bladder.
Complete bladder herniation into an inguinal hernia sac is referred to as a scrotal cystocele. This very rare condition is previously unreported in the emergency medicine literature. Some bladder involvement occurs in 1 – 4% of all inguinal hernias1 and is often an incidental (generally benign) operative finding. Patients with partial bladder herniation may report “double phase micturition.” This occurs when the patient voids then passes more urine by applying pressure to their hernia.2
Scrotal cystocele can be associated with bilateral hydronephrosis, acute renal failure, bladder lithiasis and necrosis, vesicoureteral reflux, and scrotal abscess.1 This inherently serious condition mimics the far more common inguinal hernia containing fat or bowel. Risk factors include: patients over 50 years of age, males, and obesity. ED ultrasound may strongly suggest or confirm the diagnosis. CT is definitive.
Due to its associated morbidity, emergency physicians should consider scrotal cystocele in males with obstructive uropathy and an associated inguinal hernia.
Footnotes
Aaron Berkey, MD, Department of Radiology Jason Hulsey, PACS Network Coordinator
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted April 6, 2012; Accepted April 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.12319
Address for Correspondence: John E. Hipskind MD, Department of Emergency Medicine, Kaweah Delta Medical Center, 400 West Mineral King Ave, Visalia, CA 93291
E-mail: johnhipskind@sbcglobal.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bisharat M, O’Donnell ME, Thompson T, et al. Complications of inguinoscrotal bladder hernias: a case series. Hernia. 2009;13:81–4. [PubMed]
2. Papadimitriou SH, Chlepas MA, Kokinacos CP, et al. Massive scrotal cystocele with bladder cancer. Br J Urol. 1991;67:330–331. [PubMed]


