| Author | Affiliation |
|---|---|
| Nickolas Nahm, MD | Case Western Reserve University, School of Medicine, Cleveland, Ohio |
| Jill Lubin, MEd | John Carroll University, Department of Education and Allied Studies, University Heights, Ohio |
| Jeffrey Lubin, MD, MPH | Penn State Milton S. Hershey Medical Center, Department of Emergency Medicine, Hershey, Pennsylvania |
| Blake K. Bankwitz | Case Western Reserve University, College of Arts and Sciences, Cleveland, Ohio |
| McAllister Castelaz | Case Western Reserve University, College of Arts and Sciences, Cleveland, Ohio |
| Xin Chen,BA | Case Western Reserve University, Biology Department, Cleveland, Ohio |
| Joel C. Shackson | Case Western Reserve University, College of Arts and Sciences, Cleveland, Ohio |
| Manik N. Aggarwal, BA, MPH | Texas A&M University, School of Medicine, College Station, Texas |
| Vicken Y. Totten, MD, MS | University Hospitals Case Medical Center, Department of Emergency Medicine, Cleveland, Ohio |
ABSTRACT
Introduction:
This study examined acceptance by staff and patients of a therapy dog (TD) in the emergency department (ED).
Methods:
Immediately after TD visits to a University Hospital ED, all available ED staff, patients, and their visitors were invited to complete a survey.
Results:
Of 125 “patient” and 105 staff responses, most were favorable. Ninety-three percent of patients and 95% of staff agreed that TDs should visit EDs; 87.8% of patients and 92% of staff approved of TDs for both adult and pediatric patients. Fewer than 5% of either patients or staff were afraid of the TDs. Fewer than 10% of patients and staff thought the TDs posed a sanitary risk or interfered with staff work.
Conclusion:
Both patients and staff approve of TDs in an ED. The benefits of animal-assisted therapy should be further explored in the ED setting.
INTRODUCTION
Animal-assisted therapy (AAT) is a therapeutic patient interaction with a domestic “pet-type” animal that is not one’s own pet.1 The documented benefits of AAT include improved physical, emotional, cognitive, and social functioning; reduced blood pressure and triglyceride levels; and even reduced cardiovascular morbidity and mortality.2–4 Psychiatric patients benefit by reduced stress.5 Patients with heart failure have lower epinephrine and norepinephrine levels, with systolic pulmonary artery and pulmonary capillary wedge pressure reductions after AAT.6
Potential hazards of AAT may include animal bites, allergies, and zoonotic infections.7,8 Animal-assisted therapy programs minimize these hazards by vaccinating and washing the animals, special training, and the continuous presence of handlers.4,7 Adverse events are very rare when AAT protocols are followed.9,10
There are no reports of AAT in an emergency department (ED). Although there is no reason to suppose that emergency patients would not accrue the usual benefits, the acceptance of AAT in EDs has not been examined.
METHODS
This study was approval by the local institutional review committee.
A survey was offered to each person in the ED immediately after a therapy dog (TD) had left each of 4 adult ED hallways. Therapy dogs visited the ED 6 times between July 2008 and November 2008. The survey asked about the respondent’s attitudes toward dogs in general, and about dogs in the ED. A research assistant stayed with the respondent until the survey was collected. This minimized loss due to incomplete responses, but conversely, no data were collected on those who declined to participate.
Settings
The setting was the ED of a large, Midwest, urban teaching hospital. The dog-handler teams were certified by Therapy Dogs International and certified by the hospital’s Pet Therapy Program. The 2 TDs in this study were a mixed-breed Labrador Retriever (Quincy) and a Burmese Mountain Dog (Brinkley).
Participants
We obtained a convenience sample of 125 patients and 105 staff members. For analysis, patients included both patients and their visitors; ED staff included physicians, nurses, and others. All were older than 18 years and capable of completing the survey; completion constituted consent. Staff respondents may have completed a survey at more than 1 visit, but because the TDs visit the ED only every 2 to 4 weeks, it is unlikely that many patients had completed more than 1 survey. (One patient was known to be present twice and completed 2 surveys.)
Circumstances
The hospital already had an AAT program, and the ED was part of the TDs rounds. During TD visits, certified TD handlers introduced themselves and the dogs to patients and their visitors, asking those present if they would like a visit from the therapy dog. The handlers and dog entered the room only with the approval of everyone present in the room. During the visit, patients and visitors could interact with the TD. The extent of interactions was dictated by the visit recipients. People could pet the dog, have the dog do tricks, talk about the dog, and sometimes throw a treat to the dog.
RESULTS
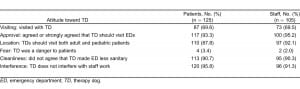
Most patients visited with the TD. Most staff (69.5%) observed the dog with a patient. The vast majority of patients and staff (93% and 95%, respectively) thought that TDs should visit the ED. Both patients and staff approved of having a TD in both the adult and pediatric sections of the ED. Only a few respondents felt the TD was dangerous: 4 (3.3%) patients and 1 (1%) staff member. Eleven patients (9.2%) and 11 staff members (10.6%) strongly agreed or agreed that TDs made the ED less sanitary. Few staff (8.6%) and fewer patients (4.2%) worried that the TD interfered with the work of the ED. The 125 patient responses and 105 staff responses are compared in the Table.
DISCUSSION
Therapy dogs are uncommon in EDs. The ED is a more chaotic environment than hospital floors, and ED-visiting animals may require additional training before entering this environment. Although developing a new AAT program can be burdensome, in hospitals where AAT is already present, consideration should be given to including the ED in AAT rounds.
There are reasons to think AAT would be particularly advantageous for ED patients, who are often highly stressed by their unexpected illness and long waits. Animal-assisted therapy may improve patient satisfaction by decreasing perceived waiting time.
One example may illustrate how a TD helped in a pediatric ED. A 4-year-old child with a head injury was frightened and refused to hold still for a computed tomography scan. When the child saw how still the TD could be after a “Down, Stay” command, he exclaimed, “If Quincy [the TD] can lay still like that, I can, too!” In this instance, TD interaction obviated the need for chemical sedation with its attendant risks.
LIMITATIONS
Our study suffered from a number of limitations: potential survey duplicates, Hawthorne effect, animal bias, immediacy, scheduling, and the individual dogs’ personalities. The TD did not visit with any critically ill patients. We had not instructed respondents to fill out a survey only once, and at least 1 patient and an unknown number of staff may have completed more than 1 survey. We did not collect data to correct for this limitation. Because 1 of the TD handlers was an emergency physician, the Hawthorne effect was unavoidable. Staff members were aware that these TD visits would be followed by an attitude survey. Most adults have already established their biases about animals. It is possible that people who liked dogs completed more surveys than dog haters. Anecdotally, it seemed that patients who refused a TD visit were also more likely to refuse to answer the survey. We did not collect data on refusers. The short time between the TD visit and the survey may have positively biased responders who were still excited by the TD visit. Staff who disapproved of AAT may have been underrepresented because of patient care duties. Responses may have been different at another time of day. The dogs were both large, weighing more than 65 lb. Attitudes toward smaller dogs or dogs of other breeds may have been different.
CONCLUSION
This is the first study of AAT in an ED. Acceptance by patients and staff was excellent. The specific benefits of AAT in EDs should be further studied.
Footnotes
Supervising Section Editor: Scott E. Rudkin, MD, MBA
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence
Vicken Y. Totten, MD, MS
University Hospitals Case Medical Center, Wearn B-17/HMP 5099, 11100 Euclid Ave, Cleveland, OH 44106.
E-mail: Vicken.Totten@UHhospitals.org.
REFERENCES
1. Gammonley J. Pet projects. J Gerontol Nurs. 1991;17:12–15. [PubMed]
2. Wisdom JP, Saedi GA, Green CA. Another breed of “service” animals: STARS study findings about pet ownership and recovery from serious mental illness. Am J Orthopsychiatry. 2009;79:430–436.[PMC free article] [PubMed]
3. Anderson WP. Pet ownership and risk factors for cardiovascular disease. Med J Aust. 1992;157:298–301. [PubMed]
4. Friedmann E, Katcher AH, Lynch JJ, et al. Animal companions and one-year survival of patients after discharge from a coronary care unit. Public Health Rep. 1980;95:307–312. [PMC free article][PubMed]
5. Lefebvre SL, Gola GC, Christensen E, et al. Guidelines for animal-assisted interventions in health care facilities. Am J Infect Control. 2008;36:78–85. [PubMed]
6. Barker SB, Dawson KS. The effects of animal-assisted therapy on anxiety ratings of hospitalized psychiatric patients. Psychiatr Serv. 1998;49:797–801. [PubMed]
7. Cole KM, Gawlinski A, Steers N, et al. Animal-assisted therapy in patients hospitalized with heart failure. Am J Crit Care. 2007;16:575–585. [PubMed]
8. Lerner-DurJawa L. Pet visitation: is it an infection control issue? Am J Infect Control. 1994;22:112.
9. Khan MA, Farrag N. Animal-assisted activity and infection control implications in a healthcare setting. J Hosp Infect. 2000;46:4–11. [PubMed]
10. Jorgenson J. Therapeutic uses of companion animals in health care. Image J Nurs Sch.1997;29:219–254.


