| Author | Affiliation |
|---|---|
| Shadi Lahham, MS | University of California, Irvine, School of Medicine, Irvine, CA |
| Khoa Tu, BS | University of California, Irvine, School of Medicine, Irvine, CA |
| Mickey Ni, BS | University of California, Irvine, School of Medicine, Irvine, CA |
| Viet Tran, BS | University of California, Irvine, School of Medicine, Irvine, CA |
| Shahram Lotfipour, MD, MPH | University of California, Irvine Medical Center, Department of Emergency Medicine, Orange, CA |
| Craig L. Anderson, MPH, PhD | University of California, Irvine Medical Center, Department of Emergency Medicine, Orange, CA |
| J Christian Fox, MD | University of California, Irvine Medical Center, Department of Emergency Medicine, Orange, CA |
ABSTRACT
Introduction:
Digital tourniquets used in the emergency department have been scrutinized due to complications associated with their use, including neurovascular injury secondary to excessive tourniquet pressure and digital ischemia caused by a forgotten tourniquet. To minimize these risks, a conspicuous tourniquet that applies the least amount of pressure necessary to maintain hemostasis is recommended. To evaluate the commonly used tourniquet methods, the Penrose drain, rolled glove, the Tourni-cot and the T-Ring, to determine which applies the lowest pressure while consistently preventing digital perfusion.
Methods:
We measured the circumference of selected digits of 200 adult males and 200 adult females to determine the adult finger size range. We then measured the pressure applied to four representative finger sizes using a pressure monitor and assessed the ability of each method to prevent digital blood flow with a pulse oximeter.
Results:
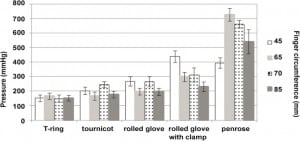
We selected four representative finger sizes: 45mm, 65mm, 70mm, and 85mm to test the different tourniquet methods. All methods consistently prevented digital perfusion. The highest pressure recorded for the Penrose drain was 727 mmHg, the clamped rolled glove 439, the unclamped rolled glove 267, Tourni-cot 246, while the T-Ring had the lowest at 151 mmHg and least variable pressures of all methods.
Conclusion:
All tested methods provided adequate hemostasis. Only the Tourni-cot and T-Ring provided hemostasis at safe pressures across all digit sizes with the T-Ring having a lower overall average pressure.
INTRODUCTION
Finger injuries alone account for approximately 3% of all emergency department (ED) visits, resulting in greater than 3.5 million ED visits in the U.S. annually.1,2 Over 75% of these visits involve soft tissue injury that may require hemostasis, and a significant number will involve injury to deep structures.3,4 To minimize morbidity associated with these injuries, digital tourniquets are necessary to provide a bloodless environment to facilitate the identification of deep tissue injuries and foreign bodies.5
While current digital tourniquet methods effectively achieve hemostasis, they have well documented complications associated with their use. Necrosis of a digit due to a forgotten tourniquet is an uncommon but catastrophic complication most associated with the methods that are the least conspicuous on the digit.6–15 Several recommendations in the literature advise against using the rolled glove finger and commercial band tourniquets due to this risk.6,9,10,15–16 This is highlighted by the recent ban in the United Kingdom (U.K.) of one of the most commonly used digital tourniquets, the surgical glove, due to 31 reported cases of digital injury and necrosis from August 2005 through November 2009.17 The more common complications related to digital tourniquets include damage to the underlying neurovascular structures secondary to excessive pressure.18–24These injuries, ranging from a transient loss of function to permanent damage, were reported to occur in a high percentage of patients undergoing limb surgery prior to the use of modern, automated pneumatic tourniquet systems.25 This is due to the inability to monitor or effectively control the pressure applied by non-pneumatic digital tourniquets, resulting in an even greater risk of injury when compared to their pneumatic tourniquet counterparts.26–29
While an ideal digital tourniquet would apply a consistently safe and effective pressure, regardless of the size of the digit or the method of application, none of the currently used methods have been proven to do this. The rolled surgical glove, elastic catheters (Penrose drain) and commercial silicon band tourniquets all have shown pressures that exceed the level known to cause nerve injury.22,30However, these methods continue to be used due to lack of a better alternative. To minimize the risk of tourniquet-related injury, current recommendations advise using the least amount of tourniquet pressure necessary to maintain hemostasis.26,31–34
In this research study, we had the following aims: 1) determine the pressure applied by each method using a modern pressure transducer; 2) determine the ability of each method to prevent blood flow into the digit; and 3) determine which method applied the least amount of pressure to the digit while preventing digital perfusion.
METHODS
Study Design
This was a single-center, prospective observational study designed to assess the ability of various digital tourniquet methods to prevent digital blood flow while measuring the pressure applied to selected digits representing the adult finger size range. The study received approval from the institutional review board. All patients gave verbal consent prior to enrollment in the study. None of the authors have any proprietary interest in any of the devices. Funding for the project was through internal research funds from the Department of Emergency Medicine at the University of California, Irvine.
Study Setting and Population
Data collection regarding finger circumferences was done in an urban university hospital ED that supports a residency program and has an annual patient census of 36,000. We enrolled a convenience sample of adult patients between July 16, 2009, and September 14, 2009, using research assistants on staff in the ED seven days a week from 8am to 12am. Inclusion criteria were age 18 years and older and presentation to the ED without a history of finger trauma, surgery or deformity. From the finger circumference data, we selected four representative finger sizes, measuring 45mm, 65mm, 70mm and 85mm, to test the different tourniquet methods.
Study Protocol
For the first part of the study, we measured the circumference of the proximal phalanx of the thumb, third and fifth digits with a standard ring-sizer placed equidistant between the metacarpophalangeal joint and the proximal interphalangeal joint of the fingers and between the metacarpophalangeal joint and the interphalangeal joint of the thumb. This site is the primary location for digital tourniquets. Using the data collected, we determined average digit circumference and the 95% range of digit circumferences of the adult population.
For the second part of the study, we measured the pressure of each digital tourniquet method across the newly established range of the digit circumferences. We found four volunteers with the following digit sizes: the smallest (45mm), largest (85mm) and mean (65mm) digit circumferences, as well as the most commonly injured digit in the adult male, the third digit (70mm).35 These subjects were four healthy males between the ages of 23–45 with digits representing these circumferences. We measured the pressure applied to these digits by each tourniquet method. Subjects were excluded from the study if they had a previous history of peripheral vascular disease, finger surgery or finger deformities. We tested in a controlled laboratory setting where data collection could be accurately assessed.
From these subjects, we used the fifth digit to represent the 45mm size, the second digit to represent the 65mm size, the third digit to represent the 70mm size, and the first digit to represent the 85mm size. All patients used their right hand for measurements to maintain consistency and uniformity during the evaluation of the various tourniquet methods. The pressure applied by each method to each digit size was recorded as well as the ability to prevent blood flow into the digit as measured by pulse oximetry. A consistent pulse waveform with a pulse oximeter value in the normal range (96–100%) indicated normal blood flow, complete loss of the pulse waveform and no reading for the pulse oximeter value indicated no digital blood flow.
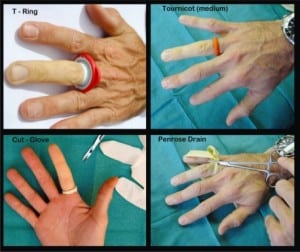
We evaluated four different tourniquet devices: the ¼-inch Penrose drain, the rolled surgical glove finger (with and without clamp), the commercially available silicon band “Tourni-cot” and the “T-Ring” digital tourniquet (Figure 1). The Penrose drain was applied as recommended by Lubahn et al.36 We made marks on the Penrose drain 26mm apart and wrapped around the digit until the marks touched, then clamped with a hemostat. We applied the rolled surgical glove according to the method of Salem, using Microdex latex gloves.37 We determined the appropriate glove size by doubling the mid-palmar width in inches.19 The glove finger that corresponded to the digit being measured was cut off just proximal to the point where the rounded tip joined the uniform width portion of the glove and at its base. We avoided cutting the glove finger anywhere across the rounded tip.22 We then slid the glove finger onto the digit and rolled proximally to form a constricting band at the appropriate location.1 The glove was applied to the digit in the same fashion when evaluating the rolled glove finger with a clamp. Once the band was in place at the base of the digit, we clamped a hemostat lengthwise onto the band. We then gave the hemostat a one-half turn (180°), the amount that may be required to rotate the handle of the hemostat out of the operative field. The Tourni-cot was applied per manufacturer’s guidelines for the four sizes. Their instructions state that small fits smaller digits and toes, medium fits digits of women and children, large fits digits of adults and extra large fits the big toe or larger thumb. To evaluate all available sizes we chose the small size on the 45mm digit, the medium size on the 65mm digit, the large size on the 70mm digit and the extra-large size for the 85mm digit. The T-Ring is one size for all digits and was slid onto each of the representative digits in accordance with the manufacturer’s recommendation.
We determined the pressure applied to the representative digit by each of the various tourniquet methods to evaluate for safety. We measured the pressure of the various tourniquet methods using the FlexiForce B201 pressure sensor, a flexible, wafer thin (0.005”) 10mm diameter disk-shaped sensor designed specifically to measure the force between two surfaces without disturbing the dynamics of the test (Figure 2). The sensor was placed in a standardized location on the dorsum of each digit equidistant from the metacarpophalangeal joint and proximal phalangeal joint. We calibrated the pressure sensor to measure pressures in the range of 0 to 1000 millimeters of mercury gathered through the Economical Load and Force (ELF) software program at a refresh rate of 200Hz. After calibrations, we applied the various digital tourniquet methods directly over the pressure sensor, on each of the representative digits. For each representative digit and digital tourniquet method, we collected 30 pressure readings in a one-minute time period over three separate trials. Prior to the application of each digital tourniquet method on the representative digits, a pulse oximeter was applied to verify digital blood flow. Values greater than 96% with consistent pulse wave form were considered normal blood flow, loss of the pulse oximeter reading and loss of pulse waveform indicated cessation of digital blood flow. The pulse oximeter was removed while each digital tourniquet method was applied, and reapplied to determine the presence or absence of blood flow. Between readings, subjects were allowed to rest for 30 minutes and digital perfusion confirmed with pulse oximetry. We monitored pulse oximetry using a commercially available pulse oximeter (Masimo, Irvine, CA). Previous studies have demonstrated pulse oximeters to be an accurate, non-invasive method to detect tissue perfusion and digital blood flow, and pulse oximetry has been used in prior tourniquet pressure studies as the monitor for pulse cessation.34,

Data Analysis
To determine the range of adult digit sizes, we enlisted 200 adult male and 200 adult female volunteers to guard against potential data losses. A sample of 174 subjects is necessary to assure a margin of error of 1.5% of the mean (at the 95% confidence level) if the standard deviation is 10% of the mean. We calculated means and 95% prediction intervals for pressure in each finger tested with various tourniquets. The 95% prediction intervals are based on the standard deviation rather than the standard error, and include 95% of individual observations, assuming the measurements are normally distributed.
RESULTS
For males, the average circumference of the thumb was 72.2mm with a standard deviation of 6.6mm, the average circumference of the third digit was 70.4 with a standard deviation of 6.4, and the average circumference of the fifth digit was 60.2mm with a standard deviation of 6.0mm. The respective values for women were 62.6mm, standard deviation of 5.0mm; 60.8mm, standard deviation of 5.1mm; and 52.1mm, standard deviation of 4.8mm.
From this data, we selected four finger circumference values to represent the adult finger size range. These included the smallest (45mm), largest (85mm), mean (65mm), and most commonly injured (70mm) finger sizes. Measurements were obtained on four subjects, each with a finger circumference that exactly matched one of the finger sizes. All tourniquet methods tested prevented digital perfusion, as assessed by pulse oximetry, on all finger sizes. The Penrose drain resulted in the highest pressure readings (394–727mmHg). The clamped rolled glove resulted in pressures between 229–440 mmHg. The unclamped rolled glove resulted in pressures between 196–268 mmHg. The Tourni-cot resulted in pressures between 176–246 mmHg. The T-Ring resulted in pressures between 149–165 mmHg. All pressure readings and standard deviations for the selected finger sizes can be seen in Table 1 and Figure 3.

DISCUSSION
Our study showed that each tourniquet method consistently prevented blood flow into the digit as evidenced by complete loss of pulse signal on the pulse oximeter; however, there was a significant difference in the amount of pressure applied to the digits by the various methods. The Penrose drain created the highest and most variable pressures of any device, in each case exceeding the recommended maximum pressure for upper extremity tourniquets (300 mmHg) and also exceeding the level known to cause injury (500 mmHg) on 75% of the digits.30,49 The clamped rolled glove finger created the next highest and most variable pressures, exceeding the recommended maximum pressure on 75% of the finger sizes. The Tourni-cot and rolled glove did not exceed the recommended maximum pressure of 300 mmHg, but we used specific guidelines to select the correct size for each digit to minimize the chance of excessive pressure. The T-Ring was applied to all digit sizes and found to produce the lowest and the least variable pressures. These devices were studied over a wide range of digit sizes. We selected one standard deviation below the lowest average finger size for females and one standard deviation above the largest average finger size for males to obtain greater than 95% of the population.
Complications related to excessive tourniquet pressures have been well documented in the literature for decades.32 Two prospective randomized studies performed in the 1980s, when less sophisticated pneumatic tourniquets and the nonpneumatic elastic bands, rolls and straps similar to current digital tourniquets were more commonly used on limbs, reported nerve injury in 71% and 77% of patients.41,42 Flatt43 reported an incidence of severe nerve palsy to occur in 0.13% of cases (1/767) of pneumatic tourniquet use. Additionally, the use of a blood pressure cuff as a pneumatic tourniquet has been shown in the literature to be problematic. This can be attributed to ischemia-reperfusion injury, as well as delayed recovery, compression neuropraxia, vascular injury of the entire upper extremity and risk of compartment syndrome.46 While advances in technology and the reduction of tourniquet pressures have significantly reduced the incidence of complications associated with the use of pneumatic tourniquets on limbs, little has changed to reduce the risks associated with digital tourniquets.43
These risks have again been highlighted by recent warnings in the literature. McEwen and Casey29note that elastic bands, elastic rolls and straps apply substantially higher pressures than pneumatic tourniquets and warn that their use may increase the incidence of tourniquet related injury and unnecessarily expose the user to potential legal liability. The U.K.’s National Patient Safety Agency released a report in December 2009 recommending the immediate discontinuation of the use of surgical gloves as tourniquets due to numerous cases of gloves being left on a digit. The NPHA review found 31 reported cases of digital injury and necrosis that occurred over the previous five years, with at least ten of these resulting in partial or complete amputation of the digit. The report notes that while the number of cases is relatively small, the degree of harm requiring amputation is great and the number of case studies reported is not an indication of the incidence of tourniquets left on digits.17
While digital necrosis from a forgotten tourniquet is the most severe complication related to digital tourniquet use, most complications are related to excessive tourniquet pressure.30,45–49 Vascular complications related to excessive pressures include intimal damage and vascular thrombosis, potentially leading to digital ischemia and necrosis.22,26,50 Persistent ischemia secondary to excessive digital tourniquet pressure has been reported after only 20 minutes of tourniquet use.26Injuries to the digital nerves may range from temporary paresthesias and weakness to permanent sensory loss and paralysis.23,51 Pressures in excess of 500mmHg have been demonstrated to cause nerve injury.30 Additionally, a safe pressure below this level that completely avoids injury has not been clearly identified.24,33 Because the risk of tourniquet-related injury increases with the use of higher pressures, it is recommended to use the lowest tourniquet pressure that effectively maintains hemostasis.26,31–34,49
The current pressure recommendation for an upper extremity pneumatic tourniquet is 200 mmHg, and it is advised not to exceed a maximum pressure of 300 mmHg.32,49 Pressures of this magnitude are unnecessary when using digital tourniquets, largely because digital artery pressures are significantly lower than arterial pressures in the arm. Mendlowitz56 reported the mean digital arterial systolic blood pressure in adults to be 100mmHg, with a pressure range of 84 to 120mmHg. Based on their experience with using digital tourniquets on patients in the clinical setting, Shaw et al19 reported that pressures of 150 mmHg to be “very adequate” to maintain hemostasis. Tuncali et al34 reported a method to estimate the arterial occlusion pressure; according to these principles the pressure necessary to prevent digital blood flow ranges from 110 to 130 mmHg.
Several previous studies have evaluated the pressures applied by the commonly used digital tourniquet methods: the Penrose drain (elastic catheter), the rolled glove finger, and a commercial silicon band.19–22 Investigators made efforts to apply the tourniquets in a standard fashion using techniques that would minimize the risk of excessive pressures. The elastic catheters (Penrose or other) were marked at specific lengths to avoid over tightening. When applying the rolled surgical glove, a subject’s hand size was first measured to estimate the appropriate size, and the commercial bands were applied per the manufacturer’s recommended technique. Despite these efforts, they recorded a wide range of pressures for each tourniquet method and found all methods frequently exerted pressures that exceed the level known to cause nerve injury (500 mmHg). The elastic catheters consistently applied the highest pressures, often in excess of 800 mmHg, leading two studies to conclude that their use should be avoided.19,21 When orthopedic attending physicians applied the Penrose drain in their usual manner, the average pressure recorded was 875 mmHg.21The rolled glove method applied pressures exceeding 500 mmHg in three out of four studies.20–22Most recently, Naim and Srinivasan22 reported the following pressures: elastic catheter (834 mmHg), the rolled glove finger (561 mmHg), and the commercial silicon band (636 mmHg). In this study, the mean pressure applied by each method exceeded not only the maximum recommended tourniquet pressure (300 mmHg), but also the level considered to be safe (500 mmHg). Similarly, we found the Penrose drain to consistently apply excessive pressures, exceeding the level known to cause injury (500 mmHg) on 75% of the digits.(30)
We also found the clamped rolled glove method to apply excessive pressures on 75% of the digit sizes. However, our data demonstrated significantly lower pressures than previous studies for the rolled surgical glove method and a commercial silicon band (Tourni-cot). While the mean pressure for the appropriate size rolled glove finger (unclamped) exceeded the recommended pressure on 50% of the digits, we did not obtain any measurements for this method that exceeded 300 mmHg. A possible explanation for the higher pressures in previous studies is removal of the tip of the glove finger anywhere across the tapering portion of the glove finger. This detail was not specified in their methods. To minimize the pressure variation that would occur with differing size holes in the glove tip, we chose to remove the glove tip just proximal to the point where the rounded tip joined the uniform width portion of the glove. While this resulted in less pressure variation than previous studies, it also results in the lowest pressure for a given glove size and potentially underestimates the pressures that will be applied when using this method in the clinical setting. Our pressures were also lower than those recorded by Naim et al.22 (561 mmHg). As in our study, they removed the glove tip at the portion of the glove just proximal to the tapered end. Potential explanations for the differences in measured pressures include using a glove with variable thickness and material properties, using a greater length of the glove finger, or by the differing methods used to measure the pressure.
Our data also showed that the appropriate size Tourni-cot exceeded the recommended pressure on 50% of the digits, but no readings exceeded the maximum recommended pressure. The one prior study that utilized a non-specified commercially available silicon band recorded a mean pressure of 636 mmHg, which is more than double our recorded pressure. There are several commercially available silicon band tourniquets; the prior study may have used a different manufacturer that varies in size or material properties compared to the one we used. The difference in pressure may also be in part due to the differing methods of measurement. While we found the Tourni-cot and unclamped rolled glove finger methods to apply pressures considered to be safe the majority of the time, this occurred after we determined the appropriate size tourniquet for a given finger size. Previous studies have noted that any variation in application techniques or errors in selecting the correct size may lead to highly variable and excessive pressures.19,21 Additionally, recent recommendations to avoid the use of low profile tourniquets due to their association with forgotten tourniquets must be considered.17
The T-Ring applied the lowest pressures of all methods on each digit size while in each case equaling or exceeding the pressure found by previous authors to adequately maintain hemostasis in the clinical setting. Of the methods tested, the T-Ring also demonstrated the least variation in pressure readings over the range of measured finger sizes, and none of the pressures exerted by the T-Ring exceeded the recommended range. When the T-Ring was placed onto successively larger digits, it applied essentially the same pressure regardless of the digit size.
LIMITATIONS
Limitations to this study are as follows: we took finger circumferences of 400 volunteers in a convenience sample to assess the finger circumference of the general population. These measurements may not be representative of the entire population due to variations in finger size. Additionally, we measured the pressures generated by several digital tourniquet methods on four different finger volunteers. According to our data on adult finger circumferences the four chosen finger circumferences represented not only the most commonly injured finger but also the 95% range of digit circumferences of the adult population. However, there is a 5% chance that a patient may have a circumference outside this range. In addition, we generated all of our pressure data on the various digital tourniquet methods using four healthy subjects in a laboratory setting. An ideal study would evaluate all of the different tourniquet methods on patients with digital injuries to assess ability to provide hemostasis. This expanded assessment would be difficult for an institutional review board to approve due to potential risks of injury and vascular compromise while waiting for results. While previous authors report tourniquet pressures of 150 mmHg to be very adequate to maintain hemostasis in patients in the clinical setting, it is possible that pressures in this range would not prevent bleeding in extremely hypertensive patients. Also the use of four standard subjects does not account for particularity of a given digit. Patients with underlying medical conditions such as finger trauma or hypertension may yield results that are different than our own.
CONCLUSION
To achieve hemostasis, a tourniquet must apply sufficient pressure to overcome the arterial blood pressure and the padding effect of the tissue between the tourniquet and the artery.52–55 The use of traditional digital tourniquet methods has been advised against due to the complications associated with their use, including injury secondary to excessive tourniquet pressures and potential for digital necrosis due to a forgotten tourniquet. Further complicating their use is the multiple sizes of tourniquets, a wide range of finger sizes, non-uniform methods of application and the inability to effectively monitor or accurately control the pressure they apply. To minimize the risk of excessive tourniquet pressure, current recommendations advise using the lowest pressure necessary to maintain hemostasis. According to our data the Penrose drain and rolled glove with clamp methods exerted high pressures in excess of 300 mmHg. The unclamped rolled glove, Tourni-cot and T-Ring methods prevented digital perfusion across the adult finger size range at significantly lower pressures. Of these three methods, the T-Ring consistently applied the lowest and least variable pressure over all tested digit sizes while maintaining hemostasis.
Footnotes
The authors would like to thank the Emergency Medicine Research Associates Program (EMRAP) and the Department of Emergency Medicine at the University of California Irvine for screening and enrolling patient volunteers to collect finger circumference measurements for our study. We would also like to acknowledge the Beckman Laser institute for providing us with the FlexiForce B201 pressure sensor and the Economical Load and Force (ELF) software program, as well as Precision Medical Devices LLC (San Clemente, CA) for providing us with the T-Ring. We deeply appreciate the assistance of June Casey and Suleman Ahmed with copy editing of the manuscript.
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted August 12, 2010; Revision received October 18, 2010; Accepted November 22, 2010
Reprints available through open access at http://escholarship.org/uc/uciem_westjem.
Address for Correspondence: J Christian Fox, Department of Emergency Ultrasound, University of California, Irvine, 101 The City Drive, Building 200 Suite 710, Orange, CA 92868
Email: jchristianfox@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Conn JM, Annest JL, Ryan GW, et al. Non–work-related finger amputations in the United States. Ann 2001–2002. Ann Emerg Med. 2005;45:630–5. [PubMed]
2. Hart RG. Hand injury prevention. Ann Emerg Med. 2005;45:636–8. [PubMed]
3. Sorok G, Lombardi D, Hauser R, et al. Acute traumatic occupational hand injuries: type, location, and severity. J Occ and Envir Med. 2002;44:345–51.
4. Frazier WH, Miller M, Fox R, et al. Hand injuries: incidence and epidemiology in an emergency service. Ann Emerg Med. 1978;7:265–8.
5. Hollander JE, Singer AJ. Laceration management. Ann Emerg Med. 1999 Sep;34:356–67.[PubMed]
6. de Boer HL, Houpt P. Rubber glove tourniquet: perhaps not so simple or safe. Eur J Plast Surg.2007;30:91–2.
7. Avci G, Akan M, Yildirim S. Digital neurovascular compression due to a forgotten tourniquet.Hand Surgery. 2003;8:133–6. [PubMed]
8. Durrant C. Forgotten digital tourniquet: salvage of an ischaemic finger by application of medicinal leeches. Ann R Coll Surg Engl. 2006;88:462–4. [PMC free article] [PubMed]
9. Hoare EM. Simple Finger Tourniquet (letter) Br Med J. 1973;3:293.
10. Chen S. Ring tourniquets for fingers. Br Med J. 1973;4:174. [PMC free article] [PubMed]
11. Hou SM, Liu TK. Salvage of tourniquet-induced thumb necrosis by a modified wrap around procedure. J Trauma. 1987;27:803. [PubMed]
12. Haas F, Moshammer H, Schwarzl F. Latrogenic necrosis of the big toe caused by left tourniquet: Clinical course and reconstruction. Chirurg. 1999;70:608. [PubMed]
13. Karabagli Y, Kose A, Cetin C. Toe necrosis due to a neglected tourniquet. Plastic and Reconstructive Surg. 2005;116(7):2036–7.
14. Bickel KD. The safety of rolled penrose digital tourniquets for use in local procedures. Plastic and Reconstructive Surgery. 2004 Mar;:1094. [PubMed]
15. Smellie G. Exsanguinating digital tourniquet. British Med J. 1973 Dec;:667.
16. Hart W, Wagner W. Letters to the Editor. J Hand Surg Eur. 2003;28:190.
17. National Patient Safety Agency, United Kingdom Reducing risks of tourniquets left on after finger and toe surgery. Dec, 2009.
18. Klenerman L. Tourniquet Time: How Long? The Hand. 1980;12(3):231–4. [PubMed]
19. Shaw JA, Demuth WW, Gillespy AW. Guidelines for the use of digital tourniquets based on physiologic pressure measurements. J of Bone and Joint Surg. 1985;67A:1086–90. [PubMed]
20. Lubahn JD, Koeneman J, Kosar K. The digital tourniquet: how safe is it? J Hand Surg.1985;10(5):664–9.
21. Hixson P, Shafiroff B, Werner F, et al. Digital tourniquets: a pressure study with clinical relevance.J Hand Surg. 1986;11(6):865–8.
22. Naim S, Srinivasan M. Digital tourniquets: a comparative analysis of pressures and pain. Acta Orthop. Belg. 2008;74:195–9. [PubMed]
23. Bruner JM. Safety factors in the use of the pneumatic tourniquet for hemostasis in the surgery of the hand. J Bone Joint Surg Am. 1951;33:221–4. [PubMed]
24. Fletcher IR, Healey TE. The arterial tourniquet. Ann R Coll Surg Engl. 1983;65B:374–5.
25. Weingarden SI, Louis DL, Waylonis GW. Electromyographic changes in post-meniscectomy patients. Role of the pneumatic tourniquet. JAMA. 1979;241:1248–50. [PubMed]
26. Dove A, Clifford R. Ischemia after use of finger tourniquet. British Med Journal. 1982;284:1162–3.
27. Aslan G, Sarifakioglu N, Bingul F. Simple and effective device for finger tourniquet: a rolled Penrose drain. Plast Reconstr Surg. 2003;111(5):1758–9. [PubMed]
28. Cheema M, Ali SN, Chukwulobelu R, et al. Investigation of safety and efficacy of pneumatic finger tourniquet. Hand Surg. 2008;13(2):55–9. [PubMed]
29. McEwen J, Casey V. Measurement of hazardous pressure levels and gradients produced on human limbs by non-pneumatic tourniquets. Proceedings of the 32nd Conference of the Canadian Medical and Biological Engineering Society 2009; Calgary, Canada. 2009. May 20–22, pp. 1–4.
30. Ochoa J, Fowler TJ, Gilliatt RW. Anatomical changes in peripheral nerves compressed by a pneumatic tourniquet. J Anat. 1972;113(Pt 3):433–55. [PMC free article] [PubMed]
31. Harrington AC, Cheyney J, Kinsley-Scott T, et al. A novel digital tourniquet using a sterile glove and hemostat. Dermatol Surg. 2004;30:1065–7. [PubMed]
32. Tejwani N, Immerman I, Achan P, et al. Tourniquet pressure: the gulf between science and Practice. J of Trauma. 2006;61:1415–8. [PubMed]
33. Newman RJ, Muirhead A. A safe and effective low pressure tourniquet. J of Bone and Joint Surg.1986 Aug;68(4)
34. Tuncali B, Karci A, Tuncali BE, et al. A new method for estimation arterial occlusion pressure in optimizing pneumatic tourniquet inflation pressure. Anesth Analg. 2006 Jun;102(6):1752–7.[PubMed]
35. Lex J. Common Problems in the ED. Audio Digest Em Med. 2007 Jun;24(11)
36. Lubahn JD, Koeneman J, Kosar K. The digital tourniquet: how safe is it. J Hand Surg. 1985 Sep;10(5):664–9.
37. Salem M. Simple finger tourniquet. Br Med J. 1973;2:779. [PMC free article] [PubMed]
38. Graham R. Pulse oximetry for vascular monitoring in upper extremity reimplantaion surgery. J Hand Surg Am. 1986;11:687–92. [PubMed]
39. Colwell A, Buntic R, Brooks D, et al. Detection of perfusion disturbances in digit reimplantation using near-infrared spectroscopy and serial quantitative flouroscopy. J Hand Surg. 31(3):456–62.
40. Skeen J, Backus W, Hovagim A, et al. Intraoperative pulse oximetry in peripheral revascularization in an infant. J of Clinical Monitoring and Computing. 1987;4:4.
41. Dobner JJ, Nitz AJ. Postmeniscectomy tourniquet palsy and functional sequelae. Am J Sports Med. 1982;10:211–4. [PubMed]
42. Nitz AJ, Dobner JJ. Upper extremity tourniquet effects in carpal tunnel release. J Hand Surg Am.1989;14:499–504. [PubMed]
43. Flatt AE. Tourniquet time in hand surgery. Archives of Surg. 1972;104:190–2.
44. Noordin S, McEwen JA, Kragh JF, et al. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91:2958–67. [PubMed]
45. Gilliatt R, Ochoa J. The cause of nerve damage in acute compression. Trans Am Neurol Ass.1974;99:71–4. [PubMed]
46. Graham B, Breault MJ, McEwen JA, et al. Perineural pressures under the pneumatic tourniquet in the upper and lower extremity. J Hand Surg. 1992;17B:262–6.
47. Love BR. The tourniquet and its complications. J Bone and Joint Surg. 1979;61-B:239.
48. Sanders R. The tourniquet, instrument or weapon? Hand. 1973;5(2):119–23. [PubMed]
49. Giannestras NJ, Cranley JJ, Lentz M. Occlusion of the tibial artery after a foot operation under tourniquet. J Bone Joint Surg. 1977;59A:682–3. [PubMed]
50. Aho K, Sainio K, Kianta M, et al. Pneumatic tourniquet paralysis: case report. J Bone Joint Surg Br. 1983;65:441–3. [PubMed]
51. Van Roekel HE, Thurston AJ. Tourniquet pressure: the effect of limb circumference and systolic blood pressure. J Hand Surg Br. 1985;10:142–4. [PubMed]
52. Levy O, David Y, Heim M, et al. Minimal tourniquet pressure to maintain arterial closure in upper limb surgery. J Hand Surg Br. 1993;18:204–6. [PubMed]
53. Reid HS, Camp RA, Jacob WH. Tourniquet hemostasis: a clinical study. Clin Orthop. 1983:230–4.[PubMed]
54. Shaw JA, Murray DG. The relationship between tourniquet pressure and underlying soft-tissue pressure in the thigh. J Bone Joint Surg Am. 1982;64:1148–52. [PubMed]
55. Mendlowitz M. Measurements of blood flow and blood pressure in clubbed fingers. J Clinical Investigation. 1940 Jul;:113–7.


