| Author | Affiliation |
|---|---|
| Landon A. Jones, MD | Department of Emergency Medicine, Cox South Emergency and Trauma Center, Springfield, Missouri |
| Mathew J. Sarsfield, MD | Department of Emergency Medicine, State University of New York Upstate Medical University, Syracuse, New York |
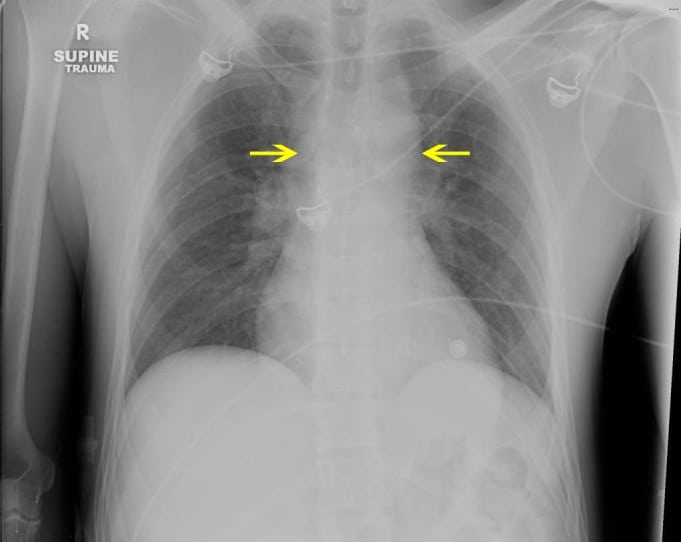
A 37 year-old male presented after an altercation in which he was dragged by a vehicle. The patient was intoxicated and asking repetitive questions. He demonstrated significant facial trauma—including frank bloody discharge from both ears and dental trauma. His vitals signs were as follows: Temperature 36.8 C; Blood pressure: 125/88; Heart rate: 90; Respiratory rate: 24; O2 sat: 100% room air. His portable chest x-ray can be seen below (Figure 1).
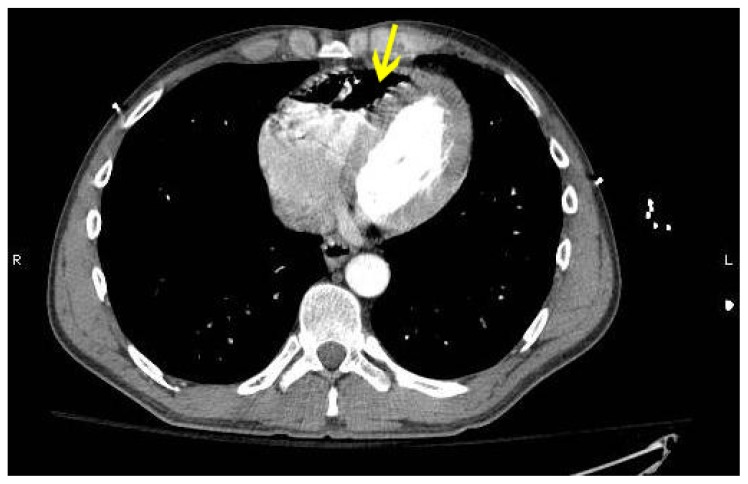
Secondary to his mechanism, intoxication, and chest radiograph results, he was sent for computed tomography (CT) imaging. Immediately post CT, his imaging was reviewed (Figure 2). Shortly thereafter, the patient’s altered mentation worsened and he acutely decompensated.
DIAGNOSIS
Iatrogenic air embolism
Iatrogenic air embolism is a rare side-effect of invasive and surgical procedures. While rare, retrospective studies demonstrate mortality up to 23% and recent prospective literature demonstrates a 1-year mortality of 21%. Morbidity is higher.1–5 Iatrogenic air emboli can be either arterial or venous. Arterial gas emboli (AGE) can manifest as chest pain, transient ischemic attack, stroke, or shock.3,5–7 While most are asymptomatic, venous gas emboli (VGE) more commonly present as shortness of breath.5, 6
It is important, though, to recognize that VGE can readily convert to AGE via right-to-left shunting mechanisms such as pulmonary arterial-venous malformations and patent foramen ovale (PFO). A PFO is present in approximately 26–39% of the general population.8–11 Additionally, it is important to remember that iatrogenic air emboli can occur secondary to procedures that we often consider routine in the emergency department, i.e., central line placement or—like our patient—CT with intravenous contrast.
In our case the patient acutely decompensated, was intubated, and received hyperbaric oxygen therapy. After hyperbarics, the patient’s status improved and he was extubated in the intensive care unit and later discharged without complications.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Landon Jones, MD. 1950 S. Scenic Ave., Apt F108, Springfield, MO 65807. Email: Landon.JonesEM@gmail.com. 7 / 2014; 15:352 – 353
Submission history: Revision received November 18, 2013; Submitted December 4, 2013; Accepted January 6, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Murphy BP, Harford FJ, Cramer FS Cerebral air embolism resulting from invasive medical precedures: treatment with hyperbaric oxygen. Ann Surg. 1985; 201:242-245
2 Massey EW, Moon RE, Shelton D Hyperbaric oxygen therapy of iatrogenic air embolism. J Hyperbaric Med. 1990; 5:15-21
3 Blanc P, Boussuges A, Henriette K Iatrogenic cerebral air embolism: importance of an early hyperbaric oxygenation. Intensive Care Med. 2002; 28:559-563
4 Bessereau J, Genotelle N, Chabbaut C Long-term outcome of iatrogenic gas embolism. Intensive Care Med. 2010; 36:1180-1187
5 Scruggs JE, Joffe A, Wood KE Paradoxical air embolism successfully treated with hyperbaric oxygen. J Intensive Care Med. 2008; 23:204-209
6 Jorgensen TB, Sorensen AM, Jansen EC Iatrogenic systemic air embolism treated with hyperbaric oxygen therapy. Acta Anaesthesiol Scand. 2008; 52:566-568
7 Ie SR, Rozans MH, Szerlip HM Air embolism after intravenous injection of contrast material. South Med J. 1999; 92:930-933
8 Kerut EK, Norfleet WT, Plotnick GD Patent foramen ovale: a review of associated conditions and the impact of physiological size. J Am Coll Cardiol. 2001; 38:613-623
9 Hara H, Virmani R, Ladich E Patent foramen ovale: current pathology, pathophysiology, and clinical status. J Am Coll Cardiol. 2005; 46:1768-1776
10 Kerr AJ, Buck T, Chia K Transmitral doppler: a new transthoracic contrast method for patent foramen ovale detection and quantification. J Am Coll Cardiol. 2000; 36:1959-1966
11 Hagen PT, Scholz DG, Edwards WD Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984; 59:17-20