| Author | Affiliation |
|---|---|
| Hassan Soleimanpour, MD | Cardiovascular Research Center, Tabriz University of Medical Sciences, Tabriz, Iran |
| Ali Taghizadieh, MD | Tuberculosis and Lung Disease Research Center, Tabriz University of Medical Sciences, Tabriz, Iran |
| Mitra Niafar, MD | Bone Research Center, Endocrine Section, Imam Reza Medical Research & Training Hospital, Tabriz, Iran |
| Farzad Rahmani, MD | Students’ Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran |
| Samad EJ Golzari, MD | Physical Medicine and Rehabilitation Research Center, Tabriz University of Medical Sciences, Tabriz, Iran |
| Robab Mehdizadeh Esfanjani, MSc | Neurosciences Research Center, Tabriz University of Medical Sciences, Tabriz, Iran |
Introduction
Methods
Results
Discussion
Limitation
Conclusion
ABSTRACT
Introduction:
Metabolic acidosis confirmed by arterial blood gas (ABG) analysis is one of the diagnostic criteria for diabetic ketoacidosis (DKA). Given the direct relationship between end-tidal carbon dioxide (ETCO2), arterial carbon dioxide (PaCO2), and metabolic acidosis, measuring ETCO2 may serve as a surrogate for ABG in the assessment of possible DKA. The current study focuses on the predictive value of capnography in diagnosing DKA in patients referring to the emergency department (ED) with increased blood sugar levels and probable diagnosis of DKA.
Methods:
In a cross-sectional prospective descriptive-analytic study carried out in an ED, we studied 181 patients older than 18 years old with blood sugar levels of higher than 250 mg/dl and probable DKA. ABG and capnography were obtained from all patients. To determine predictive value, sensitivity, specificity and cut-off points, we developed receiver operating characteristic curves.
Results:
Sixty-two of 181 patients suffered from DKA. We observed significant differences between both groups (DKA and non-DKA) regarding age, pH, blood bicarbonate, PaCO2 and ETco2 values (p≤0.001). Finally, capnography values more than 24.5 mmHg could rule out the DKA diagnosis with a sensitivity and specificity of 0.90.
Conclusion:
Capnography values greater than 24.5 mmHg accurately allow the exclusion of DKA in ED patients suspected of that diagnosis. Capnography levels lower that 24.5 mmHg were unable to differentiate between DKA and other disease entities.
INTRODUCTION
Diabetes mellitus, defined by high levels of glucose and impaired carbohydrate and lipid metabolism, is the most common endocrine disorder and includes a wide group of metabolic diseases whose major characteristic is hyperglycemia caused by impaired insulin secretion and/or function.1 Patients with diabetes mellitus are prone to important and disabling complications. One of the most important complications of the diabetes is diabetic ketoacidosis (DKA).2 DKA mostly occurs in patients with type I diabetes; however, patients with type II diabetes are also prone to DKA at early ages under stress conditions including trauma, surgery, or infection.3
DKA is defined as blood sugar levels ≥250 mg/dl, ketonuria, ketonemia, and metabolic acidosis (pH<7.3 or blood bicarbonate levels <15 meq/dl).4 Blood sugar measurement can be quickly performed using glucometry devices widely available in emergency departments (ED). Ketones in urine could be assessed rapidly using urine dipsticks. However, measurement of the acid-base levels is more challenging. Commonly, arterial blood gas (ABG), pH, and bicarbonate levels are used to diagnose acidosis and evaluate its severity. Yet, obtaining ABG samples can be a painful and time-consuming procedure.5
Alternatively, capnography may be used as an alternative, non-invasive and inexpensive (in comparison with ABG) method of assessing ventilatory response to typical metabolic acidosis of DKA.5–10 In our center, the cost of capnography is 1 United States Dollar (USD) whereas each ABG costs 2.5 USD (1 USD for blood sampling and 1.5 for the analysis).
Numerous studies have evaluated the relationship between acidosis and ETCO2, most of which are in the pediatric patients or the patients without DKA.11–15 In the current study, we aimed to evaluate the relationship between blood bicarbonate and end-tidal carbon dioxide (ETCO2) values and the predictive value of ETCO2 in DKA diagnosis in adult patients with increased blood sugar levels referred to the ED.
METHODS
We carried out a prospective cohort study of a convenience sample of patients in the ED of Imam Reza Medical Research and Training Hospital, Tabriz, East Azarbaijan, Iran, 110,000 admission per year, during a 4-month period (December 2011–March 2012).16 Sample size determination was based on the previous studies (11) in which capnography sensitivity in diagnosing DKA was reported to be 83%. Considering α=0.05, power of 80% and 6 units acceptable absolute difference in the reported sensitivity, we selected 176 people which was later increased to 181 people to compensate for expected dropouts or missing data. Patient collection was performed from 8am until 4pm seven days a week, while no sample collection was performed in the evening or night shifts.
Inclusion criteria for the study: All adult patients older than 18 years old with suspected DKA by an attending emergency physician in charge of the shift and blood sugar levels of higher than 250 mg/dl referred to our ED.
Patients likely to have metabolic disturbances from other causes were excluded from the study, including:
Gastroenteritis
Chronic renal failure
Patients unable to tolerate capnography
Respiratory diseases
Impaired consciousness
This study was approved by the Ethics Committee of “Tabriz University of Medical Sciences” and registered under the Code Number 90104.
On arrival vital signs of all patients were checked and blood sugar levels were measured by glucometer (Clever check, model TD 4209, San Chung, Taipei). Complete blood count, serum levels of sodium, potassium, urea and creatinine, urine ketone levels, and ABG were measured. Patients with blood sugar levels higher than 250 mg/dl, probable DKA diagnosis, and symptoms including nausea, vomiting, abdominal pain, and fatigue were further evaluated. ABG samples were taken for all patients by the same person, and in order to avoid human error in registering ETCO2 values by different people, capnography values were recorded by one person simultaneously using a RESPIRONICS device (model number: 7100, RESPIRONICS California Inc, California).
Capnography was performed for 1 minute at the same time the ABG sample was taken, and the total number of the registered ETCO2 in every breath in 1 minute was divided by the respiratory rate per minute; the calculated mean was considered as the ETCO2 value of each patient.
At the time of discharge, patients were divided into 2 groups, DKA and non-DKA, based on clinical consensus of their course and other supporting data.
DKA patients were hospitalized after consultation with the internal medicine service whereas non-DKA patients, after calculation of their serum osmolarity, were hospitalized in case of having hyperosmolar sera or discharged from the ED. We analyzed the results using SPSS (model number: 17.0.1, SPSS Inc, Chicago). We used descriptive statistical approaches (domains, frequency, percentage, mean ± SD and variance). To compare the qualitative data, chi-square test was used. To compare quantitative data, we used t-test and, if required, Non-Parametric Mann-Whitney U tests.
We studied normal distribution of the data using Kolmogrov-Smirnov test. Non-Parametric Mann Whitney U test was used in case of non-normal distribution of the data. To evaluate the relation between ETCO2 and ABG findings (pH, arterial carbon dioxide [PaCO2] and HCO3) in patients with increased levels of blood sugar, we used the Spearman correlation coefficient and regression curves. To define ETCO2 cut off point in diagnosing DKA, we used receiver operating characteristic curve analysis ROC). In all cases, we considered p-value less than 0.05 significant. A flow diagram of our study is presented in Figure 1.
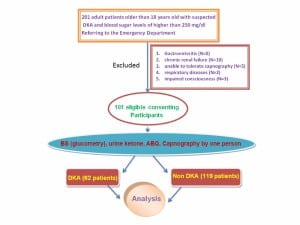
Flow diagram of study involving patients with suspected diabetic ketoacidosis.
RESULTS
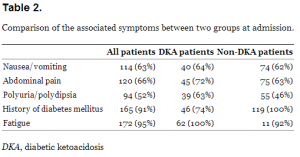
In the current study, 181 patients including 107 females were studied. The mean age was 57.9 ± 17.8 years. Sixty-two patients had DKA (%) while 119 had other conditions associated with metabolic acidosis. Table 1 shows a statistically significant difference between the 2 groups (DKA and non-DKA) regarding age, blood pH, bicarbonate, PaCO2, blood sugar and ETCO2. Table 2 presents the difference between groups for associated symptoms at admission. Spearman test revealed a significant linear correlation between pH and ETCO2 (p>0.0001, r=0.253)(Figure 2), PaCO2 and ETCO2 (p>0.0001, r=0.572) (Figure 3) and HCO3 and ETCO2 (p>0.0001, r=0.730) (Figure 4).
![Figure 2. The correlation between pH and ETCO2 levels in 2 groups (diabetic ketoacidosis [blue], non-DKA [green]).](https://westjem.com/wp-content/uploads/2014/01/wjem-14-590-g002-300x234.jpg)
The correlation between pH and ETCO2 levels in 2 groups (diabetic ketoacidosis [blue], non-DKA [green]).
![Figure 3. The correlation between PaCO2 and ETco2 levels in two groups (diabetic ketoacidosis (DKA) [blue], non-DKA [green]).](https://westjem.com/wp-content/uploads/2014/01/wjem-14-590-g003-300x249.jpg)
The correlation between PaCO2 and ETco2 levels in two groups (diabetic ketoacidosis (DKA) [blue], non-DKA [green]).
![Figure 4. The correlation between HCO3 and ETco2 levels in two groups (diabetic ketoacidosis (DKA) [blue], non-DKA [green]).](https://westjem.com/wp-content/uploads/2014/01/wjem-14-590-g004-300x250.jpg)
The correlation between HCO3 and ETco2 levels in two groups (diabetic ketoacidosis (DKA) [blue], non-DKA [green]).
![Demographics characteristics and laboratory findings of both groups (diabetic ketoacidosis [DKA] and non-DKA).](https://westjem.com/wp-content/uploads/2014/01/590-t1-300x113.png)
To study the sensitivity and specificity of capnography in diagnosing DKA patients with increased blood sugar levels, we used ROC curves. The surface area under the curve is 0.037. Given the low surface area and low sensitivity and specificity of the ETCO2 test, a determination of the cut-off point was not possible. ROC curves were also used to evaluate the sensitivity and specificity of capnography in ruling out DKA in patients with increased blood sugar levels. In Figure 5, the area under the curve is 0.963. Using this curve, a cut-off point of 24.5 with a sensitivity of 0.90 and specificity of 0.90 was achieved for ETCO2 revealing that ETCO2 >24.5 mmHg rules out DKA with a moderate confidence (Figure 5).
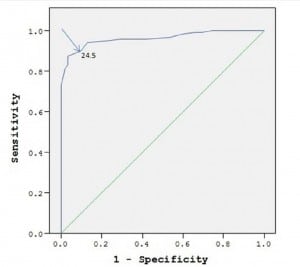
Receiver operating characteristic curve for sensitivity and specificity of capnography for diagnosis of diabetic ketoacidosis (DKA). ETCO2>24.5 mmHg with sensitivity and specificity of 0.90 rules out DKA .
DISCUSSION
Numerous factors are used to diagnose DKA, including blood sugar levels higher than 250 mg/dL, ketones in urine and metabolic acidosis.3 A conventional method of determining metabolic acidosis is to use ABG, which can be a painful, time-intensive and expensive procedure with undesirable complications. Venous blood gases have been shown to closely approximate arterial for DKA.4 An alternative method suggested by our study is to replace ABG with noninvasive capnography for determining ETCO2 and severity of metabolic acidosis.11–15
Numerous studies have been performed on the association of metabolic acidosis and capnography; these, however, have been of small sample sizes mostly focusing on either pediatric patients or other metabolic acidosis disorders. Diedre et al11, in a study of 42 pediatric patients, concluded that ETCO2 values have a direct linear relation with blood bicarbonate levels being at their low levels in DKA patients. Patients with ETCO2 values less than 29 suffered from DKA (sensitivity of 83% and specificity of 100%), whereas patients with ETCO2 values more than 36 did not have DKA (specificity of 100%). Further, Mutlu et al12, in a study on 240 non-intubated patients with metabolic disorders, suggested that a significant relationship existed between ETCO2 values and blood bicarbonate levels (r=0.506); ETCO2 values less than 25 and more than 36 were respectively suggestive of metabolic acidosis with a specificity of 83.8% and lack of metabolic acidosis with a sensitivity of 98%. Additionally, normal values of capnography closely correlated with a normal metabolic status. Agus et al13 conducted a study on 72 patients (1–21 year-olds) with DKA; significant relationships between ETCO2 values and blood bicarbonate and PaCO2 levels were found (r=0.84 and r=0.79 respectively). Moreover, Gilhorta et al14 conducted a study on 58 pediatric patients (1–18 year-olds) with type 1 diabetes. Capnography was felt to be of predictive value for DKA in combination with the clinical evaluation. ETCO2 values more than 30 could rule out DKA diagnosis with sensitivity of 100% and specificity of 86%.14
The study of Garcia et al15 on 126 DKA patients suggested a statistically significant and direct relation between ETCO2 and PaCO2 and pH.
In our study, we focused on predictive value of ETCO2 in the diagnosis of DKA in adult patients with blood sugar levels higher than 250 mg/dl and probable diagnosis of DKA.
ETCO2 levels were significantly lower in patients with DKA compared to other patients with high blood sugar levels. The more severe the acidosis and the more reduction in the blood bicarbonate levels, the more we found reduction in ETCO2 levels. Finally, based on our results, capnography can be used to rule out DKA in the patients with increased blood sugar levels; cut-off point of 24.5, sensitivity of 0.90 and specificity of 0.90.
We studied adults, and a larger sample of patients than previous investigators, 4 times (181 versus 42 people) and 3 times (181 versus 58 people) the studies of Dierdre11 and Gilhotra14, respectively.
LIMITATION
Our study had some limitations as it was of a descriptive nature and lacked a control group. Patient collection was performed in specific hours of the day only (8am until 4pm); we did not track nor report the number of the patients with high blood glucose levels referring to the ED.
Moreover, some patients were unable to undergo capnography due to their severe nausea and were excluded from the study (Figure 1). Based on the study design, we included the results of the ABG and capnography only once and did not evaluate the changes in ABG and capnography values throughout the treatment course.
CONCLUSION
DKA patients do require decisive and prompt treatment. The aim of the current study was to introduce capnography as a screening tool for DKA diagnosis. Capnography is a simple, noninvasive and inexpensive method that could be performed at bedside. A linear relation could be detected between capnography and blood bicarbonate values. Capnography could be used to rule out DKA in patients with increased blood sugar levels with a cut-off point of 24.5 mmHg, with sensitivity of 0.90 and specificity of 0.90.
Acknowledgments
The authors are grateful to all the health personnel and patients who participated in the study, in addition to the data collectors, supervisors and administrative staff of the Emergency Department of Imam Reza Hospital. Special thanks to Research Vice Chancellor Tabriz University of Medical Sciences for all the material and financial support in our study. This article was written based on a dataset of MD thesis, registered in Tabriz University of Medical Sciences.
Footnotes
Address for Correspondence: Hassan Soleimanpour, MD. Cardiovasular Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. Email: soleimanpourh@tbzmed.ac.ir. 11 / 2013; 14:590 – 594
Submission history: Revision received October 22, 2012; Submitted February 13, 2013; Accepted April 2, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Cydulka RK, Gerald E, Maloney Diabetes Mellitus and Disorders of Glucose Hemostasis. Rosen’s Emergency Medicine, 2, 7. 2010; :1633-1649
2. Eve D Losman: Weakness. Rosen’s Emergency Medicine, 1, 7. 2010; :87-92
3. Umpierrez GE, Kitabchi AE Diabetic ketoacidosis. risk factors and management strategies. Treat Endocrinol. 2003; 2:95-108
4. Micheal E, Chansky , Cary L Diabetic Ketoacidosis. Tintinalli’s Emergency Medicine, 1, 7. 2011; :1432-1438
5. Milzman Dave, Jancbar Tim Arterial Puncture and Cannulation. Clinical Procedures in Emergency Medicine, 1, 5. 2010; :349-363
6. Soleimanpour H, Gholipouri C, Golzari SEJ Capnography in the Emergency Department. Emergency Med. 2012; 2:e123
7. Soleimanpour H, Gholipouri C, Jafar R Role of anesthesiology curriculum in improving bag-mask ventilation and intubation success rates of emergency medicine residents: a prospective descriptive study. BMC Emerg Med. 2011; 11:8
8. Soleimanpour H, Salari SL, Mehryar H The Effect of Using Packed Gauze in the each buccal cavity of Edentulous Patients on facility of Bag Mask Ventilation after removing dentures. Urmia Med J. 2011; 22:195-202
9. Soleimanpour H, Sarahrudi K, Hadju S How to Overcome Difficult-Bag-Mask-Ventilation: Recents Approaches. Emergency Med. 2012; 2:e116
10. Soleimanpour H, Panahi JR, Mahmoodpoor A Digital intubation training in residency program, as an alternative method in airway management. Pak J Med Sci. 2011; 27:401-404
11. Deirdre M, Fearon , Dale W End-tidal Carbon Dioxide Predicts the Presence and Severity of Acidosis in Children with Diabetes. Acad Emerg Med. 2002; 9:1373-1378
12. Kartal M, Eray O, Rinnert S ETCO2: a predictive tool for excluding metabolic disturbances in nonintubated patients. Am J Emerg Med. 2011; :65-69
13. Agus MS, Alexander JL, Mantell PA Continuous non-invasive end-tidal CO2 monitoring in pediatric inpatients with diabetic ketoacidosis. Pediatr Diabetes. 2006; 7:196-200
14. Gilhotra Y, Porter P Predicting diabetic ketoacidosis in children by measuring end-tidal CO2 via non-invasive nasal capnography. J Paediatr Child Health. 2007; 43:677-680
15. Garcia E, Abramo TJ, Okada P Capnometry for noninvasive continuous monitoring of metabolic status in pediatric diabetic ketoacidosis. Crit Care Med. 2003; 31:2539-2543
16. Soleimanpour H, Gholipouri C, Salarilak S Emergency department patient satisfaction survey in Imam Reza Hospital, Tabriz, Iran. Int J Emerg Med. 2011; 4:2


