| Author | Affiliation |
|---|---|
| Andrew G DeNazareth, MD | Creighton University, Division of Internal Medicine, Omaha, Nebraska |
| Venkata M Alla, MD | Creighton University, Division of Cardiology, Omaha, Nebraska |
| Stephen J Lanspa, MD | Creighton University, Division of Gastroenterology, Omaha, Nebraska |
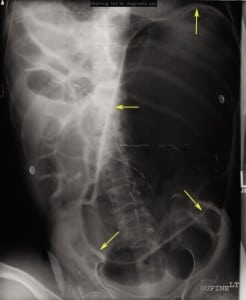
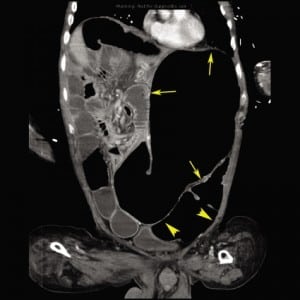
A 68-year-old male with moderate mental retardation presented to the emergency department with anorexia, constipation, and abdominal distension for 4 days. Medical history was significant for partial colon resection for presumed bowel obstruction 3 years previously (no true anatomic cause for obstruction was identified at surgery). On examination, he was dehydrated and tachycardic, with blood pressure of 90/60 mmHg and a distended, tympanic, and mildly tender abdomen. Metabolic panel, amylase, and lipase test results were otherwise normal. An abdominal radiograph demonstrated marked gastric distension with multiple dilated loops of small and large bowel (Figure 1). Computed tomography of the abdomen with contrast confirmed the above findings but did not identify any mechanical cause for bowel obstruction (Figure 2). The patient had significant symptomatic improvement after intravenous hydration, gastric decompression, and initiation of intravenous metoclopramide and erythromycin. Esophagogastroduodenoscopy revealed no evidence of gastric outlet obstruction.
Chronic intestinal pseudo-obstruction (CIPO) is a rare disorder of gastrointestinal motility characterized by repetitive/chronic symptoms of bowel obstruction in the absence of a mechanical or metabolic cause of obstruction.1,2 Radiation enteritis, drugs such as clonidine, opiates, systemic disorders such as diabetes, hypothyroidism, amyloidosis, scleroderma, and multiple sclerosis can also produce a similar clinical picture. Therefore, exclusion of aforementioned secondary causes is mandatory for the diagnosis of idiopathic CIPO. Abnormalities in the integrity of intestinal neural pathways, interstitial cells of Cajal, and smooth muscle cells of the gastrointestinal tract have been implicated in the causation of CIPO.
Acute management involves decompression, appropriate fluid and electrolyte replacement, and nutritional support.1 Prokinetic agents such as metoclopramide, erythromycin, octreotide, and neostigmine have been shown to help improve bowel transit times.1,2 Pacing of the stomach or intestine and intestinal transplantation are considered experimental. Increasing awareness about CIPO is essential to ensure early diagnosis, appropriate treatment, and hopefully avoid unnecessary abdominal surgeries in these patients.1
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted February 25, 2011; Accepted February 28, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.2.6734
Address for Correspondence: Andrew G. DeNazareth, MD
Creighton University Medical Center, Department of Internal Medicine, 601 N 30th St, Ste 5850, Omaha, NE 68131
E-mail: andrewdenazareth@creighton.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Antonucci A, Fronzoni L, Cogliandro L, et al. Chronic intestinal pseudo-obstruction. World J Gastroenterol. 2008;14:2953–2961. [PMC free article] [PubMed]
2. Merlin A, Soyer P, Boudiaf M, et al. Chronic intestinal pseudo-obstruction in adult patients: multidetector row helical CT features. Eur Radiol. 2008;18:1587–1595. [PubMed]


