| Author | Affiliation |
|---|---|
| Karl Marzec, MD | Los Angeles County + University of Southern California Medical Center, Department of Emergency Medicine, Los Angeles, California |
| Thomas Mailhot, MD | Los Angeles County + University of Southern California Medical Center, Department of Emergency Medicine, Los Angeles, California |
| Phillips Perera, MD | Los Angeles County + University of Southern California Medical Center, Department of Emergency Medicine, Los Angeles, California |
ABSTRACT
Flank pain with hematuria is a common chief complaint in the emergency department (ED). Patients are often diagnosed with renal calculi or pyelonephritis and discharged with analgesics or antibiotics and follow-up. This case study describes a patient who presented to the ED with a 1 week history of flank pain and hematuria and was subsequently found to have a large renal mass on bedside ultrasound.
INTRODUCTION
A 45-year-old male with no previous medical history presented to the emergency department (ED) with 1 week of hematuria and left flank pain. The patient had noted that over the preceding 4 days his urine had progressed from a pink color to dark red. He had also experienced left flank pain that was sharp, non-radiating, and increasing in severity over the week prior to presentation. He denied a history of renal calculi, weight loss, fevers, fatigue, or abdominal masses.
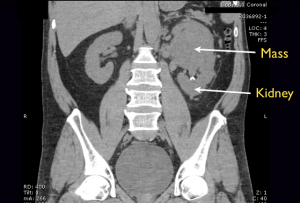
Upon physical examination, his vital signs included blood pressure of 157/89 mmHg, heart rate of 64 beats/min, temperature of 97.4 °F, respiratory rate of 18 breaths/min, and oxygen saturation of 99% on room air. The patient appeared comfortable. His abdomen was soft, non-tender and non-distended. The patient had left-sided costo-vertebral angle tenderness to palpation. There was frank hematuria in the urine sample at bedside. Subsequent microscopic analysis revealed > 50 red blood cells and 4–10 white blood cells. Bedside emergency ultrasound (EUS), initially performed to look for hydronephrosis, showed a large left renal mass ( Video). A computed tomography (CT) of the abdomen and pelvis was subsequently obtained, revealing a 13 × 9.5 × 14.7 cm exophytic anterior left renal mass with calcifications and areas of necrosis, consistent with renal cell carcinoma (Figure).
Urology consultation was immediately obtained. The patient was scheduled for a close outpatient appointment for this newly diagnosed renal tumor, which likely would require future surgical resection. In the interim period, he was referred for an outpatient CT urogram with contrast to better delineate the mass. The patient was also scheduled for follow up with oncology service. Unfortunately, the patient did not return for any of his scheduled appointments. Further attempts to reach the patient by phone and by mail were unsuccessful.
DISCUSSION
Renal cell carcinoma (RCC) constitutes approximately 3% of all adult malignancies and 80–85% of primary renal cancers.1,3,6 In 2010, an estimated 58,000 persons in the United States (U.S.) were diagnosed with RCC and about 13,000 died from the disease.6,8,9 Although the incidence of RCC in the U.S. has increased since 1975 (partly due to the increased use of noninvasive abdominal imaging), the 5-year survival rate has more than doubled over the past 50 years from 34% to 69%.6,8–10 The improved survival rate is partly attributed to earlier diagnosis, with subsequent earlier surgical intervention.6
While ultrasound (US) is less sensitive than CT for detecting renal masses, it is a convenient imaging modality with many potential benefits for the initial ED workup of flank pain and hematuria.7 Its power lies in the ability to accurately detect hydronephrosis, a clinical sign often indicative of renal colic.1–3 In fact, in prior years, the evaluation of kidney stones was performed with a combination of US and an intravenous pyelogram. However, more recently, the pendulum has moved toward the inclusion of CT imaging in many patients presenting to the ED with potential renal colic. CT has the advantage of being extremely accurate in the diagnosis of renal stones, allowing the clinician to determine both the location and the size of the stone. It also has the advantage of being able to rule out alternative and potentially serious diagnoses. However, with these benefits come some associated drawbacks. The first is the risk of radiation inherent in a CT.5 More recent data suggests that a CT of the abdomen and pelvis imparts between 10–16 mSv.14 The conversion rate most commonly used for quantification of radiation dosing, between millisieverts (mSV) and rems or rads, is 10 mSV = 1 rem or rad. While most CTs performed to assess for renal colic are protocoled without intravenous (IV) contrast, some institutions require a comprehensive CT with IV contrast for all patients with abdominal pain. This can increase the amount of radiation given during the scan, due to the CT protocols required to best assess contrast in the body. While 1 CT may not seem like an undue amount of radiation given to any patient, many patients present with repeated occurrences of renal colic and some of these patients will receive a number of CTs over their lives. It should be emphasized that it is this cumulative dose of radiation over a patient’s lifetime that has the best correlation to the risk of cancer.14
In addition to the radiation dose given during the administration of a CT, there are also economic costs to be considered when ordering all imaging tests. Bedside EUS is now routinely performed in many EDs. Some facilities are currently billing these exams under a limited code and more billing through the ED will likely occur in the future. However, at this time the vast majority of the bedside US exams performed by the emergency physician (EP) are not being billed for. Looking directly at the newest California CPT codes for CTs (74176, 74177, 74178), the California Medi-Cal website shows the following costs: For a non-contrast CT of the abdomen and pelvis (74176), the basic charge is $195.24, for a CT of the abdomen and pelvis with IV contrast (74177), the basic charge is $311.37 and for a focused CT abdomen and pelvis with IV contrast (74178), the basic charge is $395.37.15 These charges should be interpreted in terms of the relatively lower amounts allowed by Medi-Cal in relation to the billed hospital costs of these tests, as well as the differing coverages provided by other private insurance. Many patients may be forced to pay a significant co-payment out of pocket to cover the expense of a CT. Looking at the costs of US, there is a noticeable decrease in charges in relation to CT. A formal comprehensive abdominal US (76700) has a basic charge of $83.20 and a limited abdominal US (76705) has a basic charge of $60.74. Thus, there is a considerable difference in economic cost to the patient in selecting a CT versus an US.
Considering these facts, US would appear to have many benefits over CT in the initial evaluation of many patients presenting with flank pain and possible renal colic. Many urologists would argue that a first-time presentation of renal colic would best be evaluated with a CT. However, US may potentially be as efficacious in the assessment of renal colic in the younger patient with an uncomplicated case. This is especially true if the patient improves clinically in the ED and can get access to good medical follow-up. Where CT might have more of a role is in the evaluation of the older patient, especially those over 65 years of age, presenting with potential first-time renal colic to exclude alternative serious pathology. However, because many patients presenting to the ED with renal colic are young and healthy and often have repeated presentations of this disease, US offers a less expensive means for their assessment, without the undue added risk of repeated radiation doses.
This case brings up some important learning points as this patient was in the minority of patients presenting with a clinical constellation that was very similar to renal colic, yet ultimately had a more ominous diagnosis. This is why standard training courses in bedside EUS that are now integrated into the current mandated Emergency Medicine Residency Curriculum emphasize the typical findings of renal colic, as well as demonstrating when the findings are abnormal.4,7 Physicians encountering these abnormal findings on EUS are urged to order a formal study through radiology, as the investigation of renal tumors on bedside US is not within this scope of practice. Especially as physicians learn the skills of bedside US and establish their abilities in this imaging modality, performing US in a quality assurance system with over-reading and review, together with a low threshold for confirmatory testing, is a prudent strategy. However, as with any test performed by the EP in the clinical evaluation of the patients in the ED; like auscultation of the heart and lungs, interpretation of a chest radiograph or reading of an electrocardiogram-most physicians understand that an abnormal finding on patient evaluation should prompt some type of further evaluation. It follows that if the clinician encounters an abnormal finding on bedside US of the kidneys, a formal radiology performed US might be the appropriate next step. CT or MRI could then follow, if an abnormality like renal cell cancer is found and there is a time sensitive need to establish the spread of the disease to best decide the treatment course. However, the potential to diagnose a cancer sooner, like RCC, through the more widespread use of bedside EUS may contribute to an earlier work-up and potential better patient outcomes.
This case emphasizes that while renal calculi are the most common cause of flank pain and hematuria, it is prudent to also closely examine the kidneys on bedside EUS for abnormal findings beyond the mere presence or absence of hydronephrosis.1,4,7,12,13 In the patient described above, a left-sided complex renal mass was detected on EUS during the routine evaluation for hydronephrosis. The US demonstrated an upper pole left renal mass with areas of anechoic and isoechoic composition, suspicious for tumor ( Video). The normal architecture of the kidney can be seen on the right side, or inferior aspect, of the video image. Anechoic regions of renal masses are fluid-filled or cystic areas, while the isoechoic regions are solid portions of the mass.1 Renal masses with both solid and cystic structures are considered to be complex. Based on this classification scheme, this complex renal mass would be very suspicious for a renal tumor.1 In contrast, a simple renal cyst is fluid-filled, or anechoic in appearance, with a bright posterior wall due to the increased through transmission of sound. Simple renal cysts are often located to the periphery of the kidney and distort the outer architecture of the organ. Complex masses, like RCC, often arise peripherally, but grow with time to invade the central portion of the kidney. The follow-up CT (Figure) confirmed the US findings of a large and complex left renal mass, with mixed cystic and solid components. The formal radiology report noted that the mass was invading into the left renal collecting system, likely explaining the presence of gross hematuria. Several renal calculi were noted incidentally to be present in the lower pole of the left renal collecting system.
CONCLUSION
In this case study, EUS helped to identify a renal mass in a patient who presented with hematuria and left flank pain, initially thought to be renal colic on clinical evaluation. While looking for hydronephrosis, a left renal abnormality was recognized and prompted further work-up with a CT of the abdomen and pelvis. Interestingly, this patient denied any weight loss, fevers, fatigue or abdominal masses, which are all recognized clinical features associated with RCC.1,11 Like most renal tumors, this patient’s symptoms overlapped with the typical presentation of renal calculi.13 It was the findings on EUS that helped to identify the correct diagnosis and prompted the appropriate consultations. While the further evaluation prompted by the EUS did lead to the correct diagnosis and appropriate ED consultations, unfortunately the patient was lost to follow up for further outpatient visits. This course of events highlights the difficulty of current systems based healthcare practice in the United States. Perhaps, in the future an argument should be made to primarily admit such patients who have findings suspicious for RCC for further workup, thereby facilitating timely treatment and avoiding potential delays in care.
Footnotes
Supervising Section Editor: Rick A. McPheeters, DO
Submission history: Submitted May 4, 2012; Revisions received July 15, 2012; Accepted August 7, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.8.12595
Address for Correspondence: Phillips Perera, MD, Los Angeles County and University of Southern California, Department of Emergency Medicine, 1200 N State St., Los Angeles, CA 90189. Email: pperera1@mac.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Mandavia DP, Pregerson B, Henderson SO. Ultrasonography of flank pain in the emergency department: renal cell carcinoma as a diagnostic concern. JEM. 2000;18(1):83–86. [PubMed]
2. Henderson SO, Hoffner RJ, Aragona J, et al. Bedside emergency department ultrasonography plus radiography of the kidneys, ureters and bladder vs intravenous pyelography in the evaluation of suspected ureteral colic. Acad Emerg Med. 1998;5:666–671. [PubMed]
3. Atkins MB. Clinical manifestations, evaluation and staging of renal cell carcinoma. Up To Date Web site. Available at: http://www.uptodate.com/index. Accessed October 11, 2011.
4. Heller M, Melanson S. Applications for ultrasonography in the emergency department. Emerg Med Clin NA. 1997;15:735–744. [PubMed]
5. Brenner DJ, Hall EJ. Computed tomography-an increasing source of radiation exposure. N Engl J of Med. 2007;357:2277–2284. [PubMed]
6. Atkins MB, Choueiri TK. Epidemiology, pathology, and pathogenesis of renal cell carcinoma. Up To Date Web site. Available at: http://www.uptodate.com/index. Accessed October 11, 2011.
7. Emergency Ultrasound Guidelines; Policy Statement. Annals of Emerg Med. 2009;53(4):550–570.[PubMed]
8. Curhan GC, Aronson MD, Preminger GM. Diagnosis and acute management of suspected nephrolithiasis in adults. Up To Date Web site. Available at: http://www.uptodate.com/index. Accessed October 11, 2011.
9. Chow WH, Devasa SS, Warren JL, et al. Rising incidence of renal cell cancer in the United States.JAMA. 1999;281:1628. [PubMed]
10. Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations) Available at: http://www.seer.cancer.gov/csr/1975_2009_pops09/. Accessed October 11, 2011.
11. Skinner DG, Monte JE, Correa RJ, et al. Manifestations of renal cancer. Urology. 1976;8:201.[PubMed]
12. Teichman JM. Clinical Practice; Acute renal colic from ureteral calculus. NEJM. 2004;350:684.[PubMed]
13. Elton TJ, Roth CS, Berquist TH, et al. A clinical prediction rule for the diagnosis of ureteral calculi in the emergency department. Jour of Gen Int Med. 1993;8:57. [PubMed]
14. Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common CT examinations and the associated lifetime attributable risk of cancer. Arch of Int Med.2009;169(22):2078–2086. [PubMed]
15. California Government Department of Health Care Services Website, Medi-Cal Section. Available at: http://files.medi-cal.ca.gov/pubsdoco/rates/rates_information.asp?num=18&first=72142&last=79020. Accessed June 5, 2012.