Treatment Protocol Assessment
Treatment Protocol Assessment
Emergency Department Patient Satisfaction with Treatment of Low-risk Pulmonary Embolism
Westjem Read More
Treatment Protocol Assessment
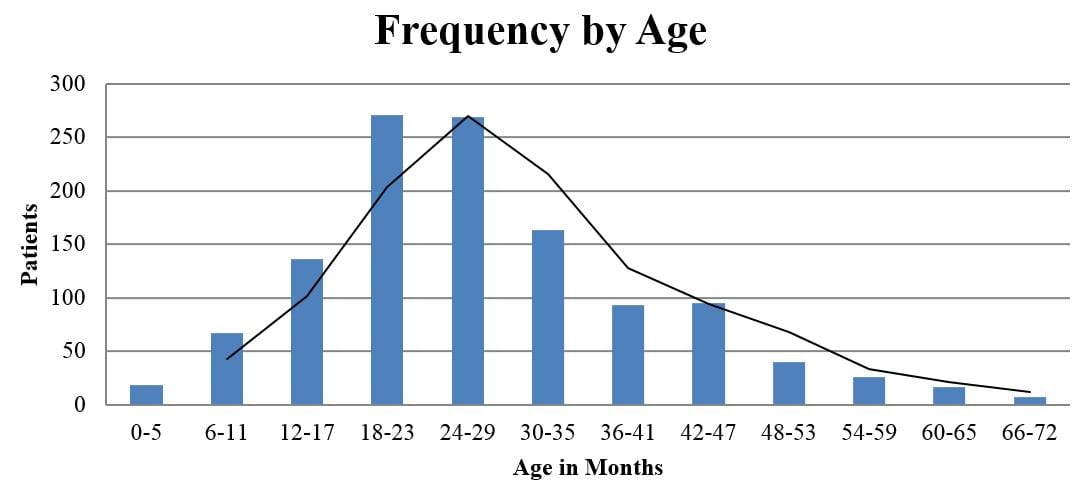
Multicenter Study of Albuterol Use Among Infants Hospitalized with Bronchiolitis
Westjem Read More
Treatment Protocol Assessment
Ruling out Pulmonary Embolism in Patients with High Pretest Probability
Westjem Read More
Treatment Protocol Assessment
Head CT for Minor Head Injury Presenting to the Emergency Department in the Era of Choosing Wisely
Westjem Read More
Treatment Protocol Assessment
Emergency Department Pain Management Following Implementation of a Geriatric Hip Fracture Program
Westjem Read More
Treatment Protocol Assessment
A Patient-Centered Emergency Department Management Strategy for Sickle-Cell Disease Super-Utilizers
Westjem Read More
Treatment Protocol Assessment
Emergency Department Management of Suspected Calf-Vein Deep Venous Thrombosis: A Diagnostic Algorithm
Westjem Read More
Treatment Protocol Assessment
Prospective Validation of Modified NEXUS Cervical Spine Injury Criteria in Low-risk Elderly Fall Patients
Westjem Read More
Treatment Protocol Assessment
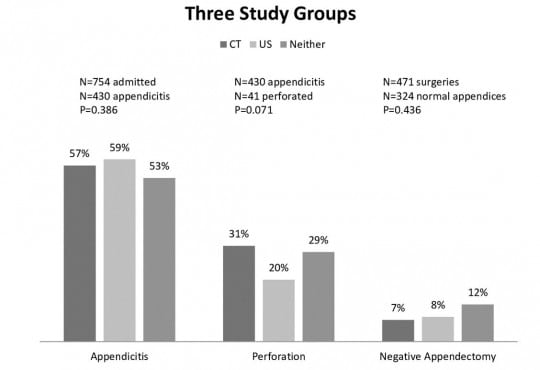
Abdominal CT Does Not Improve Outcome for Children with Suspected Acute Appendicitis
Westjem Read More
Treatment Protocol Assessment
Triple Rule Out versus CT Angiogram Plus Stress Test for Evaluation of Chest Pain in the Emergency Department
Westjem Read More
Treatment Protocol Assessment
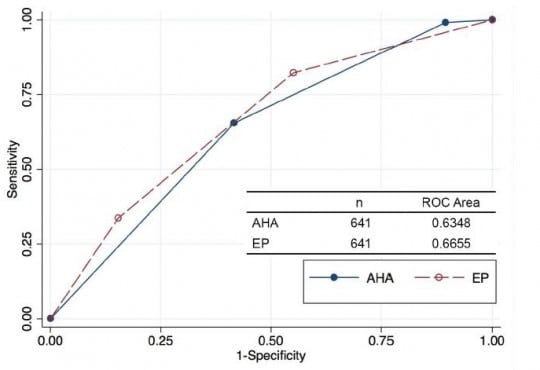
Comparing an Unstructured Risk Stratification to Published Guidelines in Acute Coronary Syndromes
Westjem Read More
Treatment Protocol Assessment
Comparison of Preloaded Bougie versus Standard Bougie Technique for Endotracheal Intubation in a Cadaveric Model
Westjem Read More
Treatment Protocol Assessment