Archives
Endemic Infections
Dengue, Zika and Chikungunya: Emerging Arboviruses in the New World
Westjem Read More
Treatment Protocol Assessment
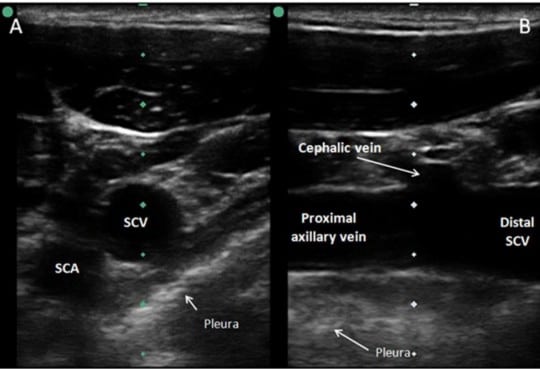
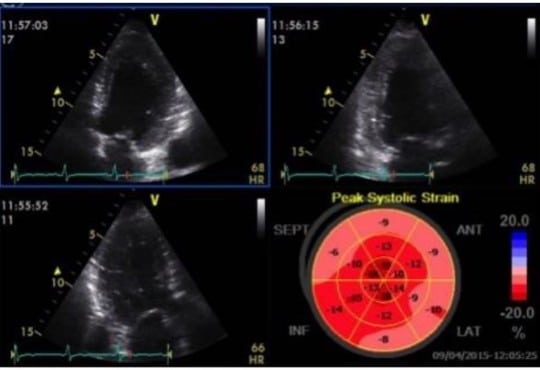
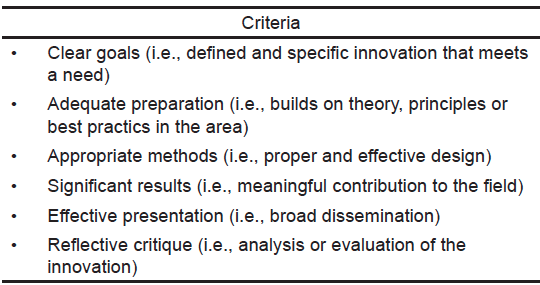
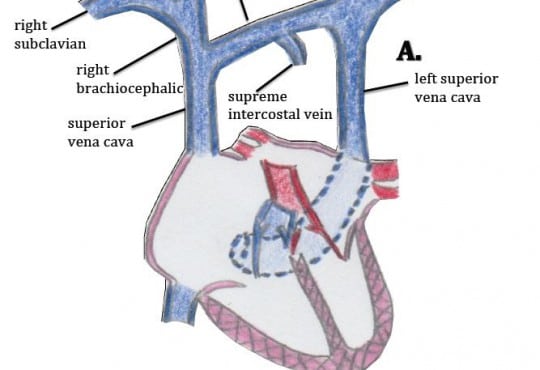
Emergency Department Management of Suspected Calf-Vein Deep Venous Thrombosis: A Diagnostic Algorithm
Westjem Read More
Patient Communication