| Author | Affiliation |
|---|---|
| Amit Chandra, MD | New York Hospital Queens, Department of Emergency Medicine |
| Todd Mastrovitch, MD | New York Hospital Queens, Department of Emergency Medicine |
| Heidi Ladner, MD | New York Hospital Queens, Department of Emergency Medicine |
| Vincent Ting | New York Hospital Queens, Department of Emergency Medicine |
| Michael S. Radeos, MD | New York Hospital Queens, Department of Emergency Medicine |
| Sandeep Samudre, PhD, MPH | Eastern Virginia Medical School, Norfolk, Virginia |
ABSTRACT
Introduction:
Recent case reports have shown that ultrasonography can be used to diagnose ocular pathology in an emergency setting. Ultrasound may be especially useful when periorbital edema and pain interfere with the examination of the post-traumatic eye. This study evaluated the ability of emergency physicians to detect a ruptured globe in an ex-vivo porcine model.
Methods:
Following a brief training lecture, 15 emergency medicine residents and 4 emergency medicine attending physicians used ultrasonography to evaluate 18 porcine eyes, randomized as normal, ruptured, or completely devoid of vitreous humor. The consequences of ultrasound applanation with this method were evaluated by measuring intraocular pressure changes with and without a 1mm clear plastic shield.
Results:
Our study participants were able to identify abnormal eyes with a sensitivity of 79% (95% CI 73% to 84%) and a specificity of 51% (95% CI 41% to 61%). Intraocular pressure increased 5% with ultrasound applanation, though with a 1mm thick plastic shield there was no measurable change.
Conclusion:
Ultrasound imaging may be a future modality to be used by trained emergency physicians to expedite the identification of a rupture globe, but it is unlikely to replace more definitive imaging techniques. The use of a clear plastic barrier in this porcine model prevents an increase in intra-ocular pressure without affecting image quality, and should be used in any future studies on this method.
INTRODUCTION
Ocular trauma, including a ruptured globe, is associated with pain and surrounding soft tissue edema that can impede the direct physical examination of the affected eye in an emergency setting. Limited access to ophthalmologic specialists and equipment may lead to significant delays in the diagnosis and treatment of traumatic pathology.
Ultrasonography has been widely used in investigation of abnormal orbital pathology, especially in cases with lens or ocular media opacifications.1 Using variations like a-scan, b-scan, Doppler, and three-dimensional approaches, ultrasonography is used to diagnose and follow up orbital diseases.2
The evaluation of ruptured globes with ultrasound presents an interesting dilemma, as management of the condition requires protection against any pressure to the globe. Globe rupture occurs following blunt or penetrating ocular trauma and is considered an ophthalmologic emergency. External signs of a ruptured globe include hyphema, irregular pupils, and a shallow anterior chamber.3 Immediate treatment when this diagnosis is suspected includes the placement of a metal shield over the eye. The potential of a ruptured globe is therefore a relative contraindication to ultrasonographic applanation (i.e. the application of pressure over the cornea) due to the theoretical risk of intraocular content extrusion.
This study focused on the ability of emergency physicians to identify sonographic changes and detect a ruptured globe in a porcine model. Additionally, changes in intraocular pressure (IOP) during probe applanation with and without a clear plastic barrier were measured in order to evaluate the consequences of this technique.
METHODS


After the initial study, a subset of normal (unruptured) eyes was cannulated and attached to a pressure sensor to evaluate intraocular pressure (IOP) changes during the procedure (Figure 4). We selected normal eyes for this aspect of the study to detect the pressure applied on the closed (vs. open) system of an intact globe. The utility of a clear plastic barrier (1mm thick) to alleviate this pressure differential was also assessed. We cut a 2 x 4 inch acrylic plastic shield 1/16” thick (US Plastics, Lima, OH) to cover the bony superior and inferior orbit. Ultrasonography was then performed using the plastic barrier to alleviate additional pressure.

Prior to this study, the investigators received a letter of exemption from the NY Hospital Queens institutional review board.
RESULTS
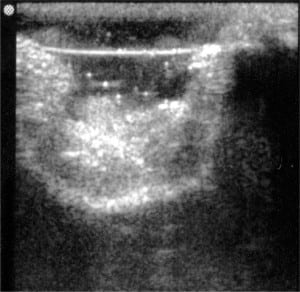
Sonography of ruptured globes revealed a number of findings indicating the diagnosis, including loss of spherical shape, scalloping of posterior globe away from the orbital wall, and lens dislocation (Figure 2). The investigation noted that at least one third of the participants consistently verbalized a correct visualization of a rupture or vitrectomy yet noted the opposite finding on their questionnaire. This confusion reflected the participants’ misunderstanding of the definitions of rupture (MVL) versus vitrectomy (CVL). To preserve the source data, their inconsistency was not corrected during the study, but the final data was merged to allow any indication of an abnormal globe (moderate or complete vitreous loss) to be a positive finding if the experimental eye in question was indeed abnormal. In other words, a participant could identify an MVL eye as a vitrectomy or a CVL as a rupture.
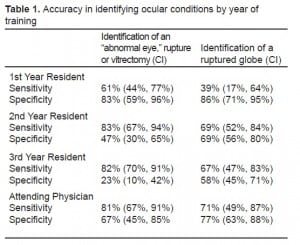
The sensitivity of this technique to identify globe rupture, using this merged data set, was 79% (95% CI 73% to 84%). The specificity was 51% (95% CI 41% to 61%). Using an unmerged data set, i.e. giving credit only for correct identification of a rupture, the sensitivity was 64% (95% CI 54% to 73%), and the specificity was 71% (95% CI 64% to 77%). Based on training level, attending emergency physicians (EPs) were consistently more accurate than residents in identifying ocular conditions, although second-year residents as a group had the highest scores. A breakdown of results (with 95% confidence intervals) by level of training is summarized in Table 1.
When maximal pressure was applied with the probe on normal eyes, IOP increased by 17%. IOP increased by only 5% when using the minimal amount of pressure to obtain a clear image. The probe did not cause a measurable increase in IOP nor was the ultrasound image quality altered when a plastic shield was used.
DISCUSSION
Ultrasonography provides a readily available, rapid, non-invasive imaging modality to evaluate the traumatic eye. An ultrasound machine can be available for use where the diagnosis would otherwise be delayed by limited access to ocular computed tomography, magnetic resonance imaging, and ophthalmologic consultation.
Recent studies have shown that EPs can use ultrasound to diagnose ocular pathology. Blaivas et al.4showed ultrasound’s capability in diagnosing ruptured globes, retinal detachments, lens dislocations, and central retinal artery occlusions in 26 out of 61 patients with acute visual changes or ocular trauma. A subsequent study by Shriver5 in 2005 demonstrated the ability of ultrasonography to detect intraocular metallic foreign bodies. Other than the Blaivas article, this specific method of evaluation has not been described previously as a technique to identify a ruptured globe.
This study demonstrated that ultrasound may one day be used by appropriately trained EPs in the future to expedite the diagnosis of globe rupture; however, the sensitivity and specificity of this test indicate that it is unlikely to replace more definitive imaging modalities. The use of a clear plastic barrier prevents an increase in IOP without affecting image quality, and future research should employ this technique. The higher sensitivity of second-year residents may be explained by an increased comfort level with ultrasonography as a result of a dedicated one-month ultrasound training course initiated for them over the previous year (and therefore not inclusive of first-or third-year residents). This study had several limitations: the porcine model; the limited pre-study training in ocular ultrasound; and the confusion on the study day between a rupture and vitrectomy. The porcine model allowed participants to identify abnormalities in the globe’s shape, the location of the lens, and the volume of vitreous humor; however, it did not allow for a simulation of vitreous hemorrhage, which is often associated with traumatic globe rupture.
Future research in a live animal or cadaveric human model, with a longer training lecture that stressed the difference between the positive control and experimental group, would be helpful in evaluating this diagnostic technique further before any practical recommendations can be made.
Footnotes
The authors would like to thank Dr. Jim Ryan, Dr. Jay Gupta, Dr. William Manson, Ms. Lily Kwan, Dr. Michael Radeos, Dr. Frank Lattanzio Jr., and Dr. Fernando Silva for their contributions to this study.
Supervising Section Editor: J. Christian Fox, MD
Submission history: Submitted October 30, 2008; Revision Received March 2, 2009; Accepted March 22, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Amit Chandra, MD, Department of Emergency Medicine, New York Hospital Queens, 56-45 Main Street, Flushing, NY 11355
Email: Amitchandra2002@hotmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Restori M, McLeod D, Wright JE. Diagnostic ultrasound in ophthalmology. J R Soc Med.1980;73:273–8. [PMC free article] [PubMed]
2. Fledelius HC. Ultrasound in ophthalmology. Ultrasound Med. Biol. 1997;23:365–75. [PubMed]
3. Mitchell J. Ocular emergencies. In: Tintinalli JE, Kelen GD, Stapczynski, et al., editors. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw-Hill; 2004. pp. 1449–64.
4. Blaivas M, Theodoro D, Sierzenski P. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9:791–9. [PubMed]
5. Shriver SA, Lyon M, Blaivas M. Detection of metallic ocular foreign bodies with handheld sonography in a porcine model. J Ultrasound Med. 2005;24:1341–6. [PubMed]


