| Author | Affiliation |
|---|---|
| Ashraf QaQa, MD | Seton Hall University/St.Michaels Medical Center, Department of Internal Medicine, Newark, NJ |
| Joseph Daoko, MD | Seton Hall University/St.Michaels Medical Center, Department of Cardiology, Newark, NJ |
| Nesreen Jallad, MD | Seton Hall University/St.Michaels Medical Center, Department of Cardiology, Newark, NJ |
| Omar Aburomeh, MD | St. Louis University Hospital, St. Louis, MO |
| Irvin Goldfarb, MD | Seton Hall University/St.Michaels Medical Center, Department of Cardiology, Newark, NJ |
| Fayez Shamoon, MD | Seton Hall University/St.Michaels Medical Center, Department of Cardiology, Newark, NJ |
ABSTRACT
Introduction:
Takotsubo syndrome (TTS) is a reversible cause of heart failure rarely described in African-American patients. This study aimed to compare and contrast the clinical characteristics of TTS in African-American (AA) and non-African-American (NAA) patients.
Methods:
We retrospectively reviewed the charts of eight patients (four AA and four NAA) diagnosed with TTS, between June 2006 and August 2008, in four different teaching hospitals: St Michael’s Medical Center, St Joseph’s Medical Center, Trinitas hospital and St Louis’ University Hospital. We compared the patients with regard to presenting symptoms, precipitating stressors, electrocardiographic findings, troponin levels, ejection fraction and in-hospital course.
Results:
All patients were females (mean age 64 for AA and 67 for NAA). All patients experienced chest pain and had elevated troponin levels. Two AA and three NAA patients had associated shortness of breath and one NAA had syncope. All AA and three NAA had T-wave inversions. Three NAA and one AA had ST segment elevation. Three patients in both groups developed prolongation of the QT interval. Coronary angiograms did not reveal any significant obstructive coronary artery disease. Three patients, all NAA, needed hemodynamic support during their hospital stay but none died.
Conclusion:
AA and NAA women with TTS have similar presenting symptoms but may differ in the electrocardiographic findings and in-hospital course of the disease.
INTRODUCTION
Takotsubo syndrome (TTS) is a transient acute cardiac disorder with a similar presentation to ST-segment elevation myocardial infarction (STEMI).1,2 TTS usually affects postmenopausal women and is characterized by a new cardiac motion abnormality that commonly involves the apex of the left ventricle in the absence of significant obstructive coronary artery disease.3 This interesting syndrome was first described in Japan about 16 years ago. In Japanese, takotsubo is the name given to the fishing jar used to catch an octopus. This jar has a wide base with a narrow neck, similar in shape to that of the clinical entity seen on left ventriculography in TTS.4 Many other names have been used for this syndrome, including transient left ventricular apical ballooning syndrome, stress-induced cardiomyopathy and ampulla cardiomyopathy.5–7
Awareness of this rare syndrome is increasing and cases of TTS have been diagnosed and reported in many areas of the world among different ethnic groups. Most of the case series and reports in the literature describe TTS in Asians and Caucasians, who are considered the most commonly affected ethnic groups.8–11 However, to our knowledge TTS has been described in African-American (AA) patients in only one case series and few case reports.12 To further investigate the nature of this syndrome and how it behaves in this ethnic group, we compared the clinical characteristics of TTS in AA patients with those in patients from other ethnicities.
METHODS
Institutions and settings
TTS is an infrequent syndrome that has been estimated to account for 1–2 % of patients diagnosed with STEMI.11 In this retrospective chart review study, we included eight patients who were divided into two groups, the first consisting of four AA patients and the other of four non-African American patients (NAA). All patients had been diagnosed with TTS between June 2006 and August 2008 in the following four teaching hospitals:
-
Saint Michael’s Medical Center, a 357-bed regional tertiary care, teaching, and research center in the heart of Newark, New Jersey
-
Saint Joseph’s Medical Center, a 642-bed teaching tertiary medical center and Level 2 Trauma Center, providing care to the residents of northern New Jersey
-
Trinitas Regional Medical Center, a 531-bed teaching hospital in Elizabeth, New Jersey
-
Saint Louis University Hospital, a 356-bed academic teaching hospital in St. Louis, Missouri
All patients had serial electrocardiograms (ECGs), serial cardiac biomarker level measurements, transthoracic two-dimensional echocardiography (2-D Echo) and invasive coronary angiogram or coronary computed tomography angiogram. All patients had repeated follow-up 2-D Echo.
Criteria
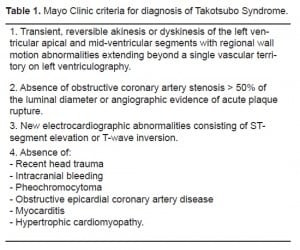
All patients fulfilled the suggested Mayo Clinic criteria for diagnosis of TTS (Table 1).2
RESULTS
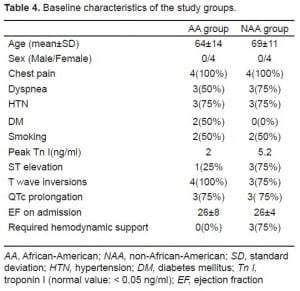
The demographics, clinical characteristics, ECG findings and echocardiographic results of the AA group are included in Table 2 and of the NAA group in Table 3. All patients were postmenopausal females.3 The mean age of the AA group was 64 ± 14 years, and the mean age in the NAA group was 69 ± 11 years. All patients had complained of chest pain at presentation and five had associated dyspnea (two AA and three NAA).
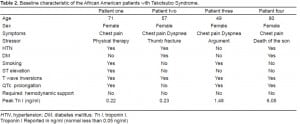
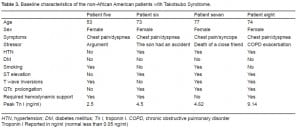
All study patients reported either emotional or physical stress within a few hours before admission. The stressors included exacerbation of chronic obstructive pulmonary disease, thumb fracture with severe pain, intensive physical therapy, a heated argument, the death of a close relative or friend and a son who was injured in a traffic accident.
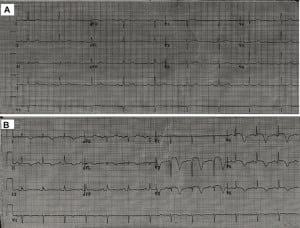
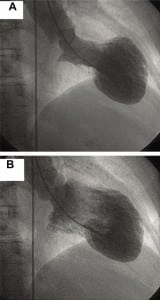
ST-segment elevation was observed in three NAA (3 of 4, 75%), but in only one AA patient (1 of 4, 25%). All AA patients (4 of 4, 100%) and three NAA (3 of 4, 75%) developed diffuse deep T-wave inversions (Figure 1). Prolongation of the QT interval was noticed with equal frequency in AA and NAA patients (3 of 4, 75%).
All patients had elevated cardiac biomarker levels, including troponin I. The mean peak troponin I level was 5.2 ng/ml in the NAA patients and 2.0 ng/ml in the AA patients.
All patients had 2-D Echo done at admission, and all had a low ejection fraction (EF) with a global wall motion abnormality of the left ventricle. The mean EF in AA patients was 25 ± 7% and that in NAA patients was 26 ± 5%.
All patients had an invasive coronary angiogram, except one AA patient who underwent a computerized tomography angiogram of the coronaries (the patient refused cardiac catheterization). None of the patients had evidence of significant obstructive coronary artery disease, and all patients who underwent an invasive coronary angiogram were assessed by left ventriculography, which confirmed a global left ventricular wall motion abnormality with apical ballooning (Figure 2 A and B). Of the eight patients, three (all NAA) developed hypotension and required hemodynamic support (intra-aortic balloon pump or vasopressors).
All patients improved clinically and the repeated 2-D Echo showed improvement of left ventricular function in all patients. The 2-D Echo of patient one showed resolution of the apical ballooning with improvement in EF from 20% to 35% within two weeks. In patient two, EF improved from 35% to 65% within 10 days. Patient three had an EF of 20% on admission that improved to more than 45% on repeated echo after six weeks. Patient four had an EF of 25% on admission that improved to 45% within two days. The EF of patients five and six increased from 20% and 30% to 65% and 60%, respectively, in two weeks. The EF of patient seven improved within six weeks (from 30% to 55%) and that of patient eight increased from 25% to 65% in about five weeks. The study results for the AA and NAA patients are summarized in Table 4.
DISCUSSION
Because little has been reported to date about the nature and clinical characteristics of TTS in African-American patients, our study is helpful in understanding this syndrome. We described TTS in this understudied ethnic group and highlighted the major differences observed in the characteristics of this group compared with those of patients from other ethnicities.
The most commonly reported presenting symptoms of TTS are chest pain and dyspnea, in 83.4% and 20.4% of patients, respectively.1,11 Our data were consistent with those findings, showing that chest pain followed by dyspnea are the most common presenting symptoms in both AA and NAA patients. This finding differs from that reported in a recent study by Patel et al.12 in which none of the AA patients experienced chest pain but most reported dyspnea at presentation.
Acute, severe emotional or physical stress is believed to be the main precipitating factor of TTS, but the exact pathogenesis is not well understood. Our data support this, with all patients in both groups reporting either major physical or emotional stressor preceding the onset of the symptoms. High catecholamine levels and microvascular dysfunction are thought to be important in TTS.8,9 These factors could explain part of the clinical and histological findings of this syndrome, including the contraction-band necrosis and mononuclear infiltrates that have been described in the endomyocardial biopsies of some patients with TTS.8
The clinical presentation of TTS classically is similar to STEMI: patients experience chest pain and have elevated troponin levels and ST-segment elevation.2 A recent systematic review of the literature found that ST-segment elevation was the most common ECG abnormality, reported in about 82% of patients, followed by T-wave inversion at 64%.11 Our study was consistent with these data in the NAA group but not in the AA group, in which T-wave inversions were the most common ECG abnormality; however, ST elevation was an infrequent finding. The AA patients in our study were more likely to present as Non STEMI (NSTEMI), whereas the NAA were more likely to have the classic STEMI presentation.
The T-wave inversions in our AA patients involved multiple leads and were the most common ECG abnormality in this group. The deep and wide shape of the T waves looked similar to that of the NAA group. From these observations, we think that the T-wave abnormality in AA patients may not differ from that described in Caucasians and Asians with TTS and that the T waves in this interesting syndrome will be shown to have a characteristic shape.
Our observations are consistent with the QT prolongation that has been reported in many studies.11–13 We found that QT prolongation in the AA group is as common as it is in the NAA group and that none of the patients in either group developed ventricular tachyarrhythmia during hospitalization, which has been reported in several case reports as a possible complication of TTS.11We think that serious tachyarrhythmias are not a common complication of TTS and that the prolonged QT interval associated with this syndrome generally has a benign course. However, larger follow-up studies are needed to form a solid conclusion about this issue and to report the incidence of this complication.
Several acute complications of TTS have been reported in the literature, including ventricular fibrillation, cardiogenic shock, pulmonary edema, and, rarely, left ventricular rupture.11–16 In our study, three patients developed hypotension and cardiogenic shock, all of whom were NAA patients and all of whom required hemodynamic support by intra-aortic balloon pump or vasopressors. These findings differed from those suggested in several reports about TTS in Caucasians and Asians, where the authors considered TTS a benign disease. From these observations, we think that close monitoring of patients with TTS is crucial, and we suggest conducting larger studies to address the in-hospital course of the disease and the short-term morbidity and mortality rates associated with it.
On the other hand, our study showed that none of the AA patients developed cardiogenic shock, although the mean EF of this group is almost the same as that for the NAA group. Why the AA patients in our study tolerated TTS better than the NAA patients and why none of them had hypotension or cardiogenic shock is unclear. Genetic background may be important, but more studies of AA patients with TTS are required to answer these questions and to explain the major differences we found in our study.
LIMITATIONS
There were some limitations in this study with respect to sample size and the study design. The number of the patients was small and all patients were females. The study was retrospective, which lacks the follow up to determine the long-term morbidity and mortality associated with TTS, if any. In addition, solid conclusions are difficult to form in this study; however, reporting these findings and differences may help to understand the nature of this syndrome
CONCLUSION
AA women with TTS have similar presenting symptoms as NAA women, however they may not have the classic ST segment elevation at presentation and may be more likely to present as NSTEMI. TTS is not always a benign condition and hemodynamic instability is a possible complication. Our AA patient group tolerated TTS better than the NAA group, and fewer developed hypotension or needed hemodynamic support.
Footnotes
Supervising Section Editor: Shahram Lotfipour, MD, MPH
Submission history: Submitted February 23, 2010; Revision received September 28, 2010; Accepted October 25, 2010
Reprints available through open access at http://scholarship.org/uc/uciem_westjem.
Address for Correspondence: Fayez E. Shamoon, MD, FACC, Department of Cardiology, St. Michael’s Medical Center, 111 Central Ave., Newark, NJ 07102, USA
Email: shucvd@smmcnj.org and Email: ayqs@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int J Cardiol. 2008 Mar 14;124(3):283–92. [PubMed]
2. Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med.2004;141(11):858–65. [PubMed]
3. Jabaudon M, Bonnin M, Bolandard F, et al. Takotsubo syndrome during induction of general anaesthesia. Anesthesia. 2007;62(5):519–23.
4. Brenner ZR, Powers J. Takotsubo cardiomyopathy. Heart Lung. 2008;37(1):1–7. [PubMed]
5. Mitchell JH, Hadden TB, Wilson JM, et al. Clinical features and usefulness of cardiac magnetic resonance imaging in assessing myocardial viability and prognosis in Takotsubo cardiomyopathy (transient left ventricular apical ballooning syndrome) Am J Cardiol. 2007;100(2):296–301.[PubMed]
6. Mitsuma W, Kodama M, Ito M, et al. Serial electrocardiographic findings in women with Takotsubo cardiomyopathy. Am J Cardiol. 2007;100(1):106–9. [PubMed]
7. Ito K, Sugihara H, Katoh S, et al. Assessment of Takotsubo (ampulla) cardiomyopathy using 99mTc-tetrofosmin myocardial SPECT-comparison with acute coronary syndrome. Ann Nucl Med.2003;17(2):115–22. [PubMed]
8. Yoshida T, Hibino T, Kako N, et al. A pathophysiologic study of tako-tsubo cardiomyopathy with F-18 fluorodeoxyglucose positron emission tomography. Eur Heart J. 2007;28(21):2598–604.[PubMed]
9. Kume T, Akasaka T, Kawamoto T, et al. Assessment of coronary microcirculation in patients with takotsubo-like left ventricular dysfunction. Circ J. 2005;69(8):934–9. [PubMed]
10. Donohue D, Movahed MR. Clinical characteristics, demographics and prognosis of transient left ventricular apical ballooning syndrome. Heart Fail Rev. 2005;10(4):311–6. [PubMed]
11. Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27(13):1523–9. [PubMed]
12. Patel HM, Kantharia BK, Morris DL, et al. Takotsubo syndrome in African-American women with atypical presentations: a single-center experience. Clin Cardiol. 2007;30(1):14–8. [PubMed]
13. Ghosh S, Apte P, Maroz N, et al. Takotsubo cardiomyopathy as a potential cause of long QT syndrome and torsades de pointes. Int J Cardiol. 2009;136(2):225–7. [PubMed]
14. Sharkey SW, Lesser JR, Zenovich AG, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005;111(4):472–9. [PubMed]
15. Tsuchihashi K, Ueshima K, Uchida T, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001;38(1):11–8.[PubMed]
16. Akashi YJ, Tejima T, Sakurada H, et al. Left ventricular rupture associated with Takotsubo cardiomyopathy. Mayo Clinic Proceedings. 2004;79(6):821–4. [PubMed]


