| Author | Affiliation |
|---|---|
| Craig Harrison, MD, MPH | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
| Wirachin Hoonpongsimanont, MD, MS | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
| Craig L. Anderson, MPH, PhD | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
| Samer Roumani, BS | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
| Jie Weiss, PhD | Department of Health Science, California State University Fullerton, Fullerton, California |
| Bharath Chakravarthy, MD, MPH | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
| Shahram Lotfipour, MD, MPH | Center for Trauma and Injury Prevention Research, Department of Emergency Medicine, School of Medicine, University of California Irvine, Irvine, California |
Introduction
Methods
Results
Discussion
Limitations
Future research
Conclusion
ABSTRACT
Introduction
The primary objective was to identify the most common reasons for intending to cut back on alcohol use, in emergency department (ED) and trauma patient populations. The secondary objective was to determine the association between reason to cut back on alcohol and education level.
Methods
We conducted the study at a level one trauma center in California between 2008 and 2012. This was a retrospective analysis of data collected from computerized alcohol screening and intervention (CASI). We excluded patients who drank too little, and those whose scores were consistent with dependency (Alcohol Use Disorders Identification Test [AUDIT]>19). The CASI database includes the patient’s age, gender, language, education level, an AUDIT score (1–40 scale), a readiness to change score (1–10), and the option to choose any of 10 “reasons to cut back” on their alcohol consumption.
Results
From 10,537 patients, 1,202 met criteria for the study (848 ED, 354 trauma). Overall, the most common reasons cited for cutting back on alcohol were “To avoid health problems” (68.5%), “To avoid getting a DUI” (43.6%), “It could save me money” (42.0%), and “To avoid situations where I could get hurt” (41.0%). Trauma patients cited the following reasons significantly more than ED patients: “To avoid situations where I could get hurt” (46.3% versus 38.8%, respectively), “So I can be in control of my behavior” (40.7% versus 32.2%), and “My partner or spouse wants me to stop” (20.1% versus 15.0%). Additionally, those patients who cited “To avoid health problems” reported 1.2 points higher than average (p<0.001) on the 10-point readiness to change scale. Those who have completed some college or an associate degree cited “To avoid health problems” less often than high school graduates (odds ratio [OR] 0.45), while they cited “To avoid situations where I could get hurt” (OR 2.5) and “To avoid being in a car crash caused by alcohol use” (OR 3.8) more often than high school graduates.
Conclusion
Health, injury, finances, and legal issues remain top concerns for patients, while trauma patients specifically had proportionately more concerns with situations where they could get hurt. [West J Emerg Med. 2014;15(3):337–344.]
INTRODUCTION
Alcohol is a major ongoing public health concern, with evidence of potential for chronic erosion of family structure, employment, and overall health.1 More significantly, alcohol is a major cause of motor vehicle collisions, along with the subsequent injuries, hospitalizations and deaths.2 The Centers for Disease Control (CDC) data show that the average annual alcohol-attributable mortality due to excessive use in the United States from 2001–2005 included 36,643 deaths due to chronic causes (cancer, liver cirrhosis, and heart disease) and 43,731 deaths attributed to acute alcohol-induced causes.1 Motor-vehicle traffic crashes, homicide, and suicide composed 31.6%, 17.8%, and 16.5% of alcohol-attributable deaths respectively. The CDC2 further indicates that there were 112 million incidents of alcohol-impaired driving in 2010, thus highlighting the magnitude of this problem nationwide.
Numerous public health campaigns regarding the perils of alcohol-impaired driving and alcohol dependence have been conducted over the past several decades. While these need to continue, more innovative solutions are required, as the data are suggestive of a worsening nationwide problem. Recent data showed that the incidence of alcohol-impaired driving appears to be increasing, up 12.9% from 75.7 million in 2004 to 85.5 million just 4 years later.3 Additionally, certain predictors of hazardous drinking behavior in adult trauma patients are increasingly recognized, such as male gender, younger age, and higher blood alcohol concentrations.4 In response to this ongoing public health problem, emergency departments (ED) have been actively involved in alcohol screening and providing intervention through programs such as Screening, Brief Intervention, and Referral to Treatment (SBIRT) and Computerized Alcohol Screening and Intervention (CASI). CASI uses an Alcohol Use Disorders Identification Test (AUDIT) score to categorize patient drinking behavior.
Newer research, however, based upon these AUDIT scores and CASI exams, is revealing additional valuable data, regarding the importance of knowing the intended reasons for cutting back on drinking. For example, Barnett et al5 were able to demonstrate in the college-aged population that the motivation for changing alcoholic behavior is strongly associated with a patient’s attribution of alcohol to certain events. Specifically, the authors noted that a “perceived aversiveness of the incident predicted motivation to change drinking and heavy drinking” (p. 760). Walton et al6 further supported this in showing that patients in the ED are more receptive to brief interventions (BIs) when they attribute their hospital visit to a period of drinking.
Few studies exist that show associations between reason to cut back and educational attainment, although some recent research reveals associations between educational attainment and early alcohol dependency.7 After adjusting for shared familial contributions to educational attainment, researchers found in co-twin studies that the likelihood of completing less than 16 years of education was significantly higher for those who used alcohol before age 18 or for those with a lifetime alcohol dependence diagnosis.
The primary objective of this study was to identify the most common reasons for intending to cut back on alcohol usage, through an examination of data collected from CASI in an ED setting. We compared reasons to cut back for trauma and ED patients, and also looked for differences in readiness to change among patients citing different reasons to cut back. A secondary objective was to look at associations between reasons to cut back and education level.
METHODS
Study Design and Protocol
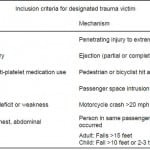
This was a retrospective analysis of a convenience sample, whose responses were collected via CASI at an urban level I trauma center university hospital in California, between November 2008 and January 2012. Figure 1 shows the subject selection process, which began with the exclusion of 8,469 patients because they reported drinking within the NIAAA-recommended drinking limits. We excluded 264 patients with an AUDIT score >19 (consistent with a dependency on alcohol), and 602 incomplete surveys were also removed, leaving 1202 complete responses from non-dependent drinkers exceeding the NIAAA-recommended drinking limits. Patients included in the study were aged 18 and over, and their responses had been collected via CASI, 7 days a week by trained research associates. ED patients in this study are classified as non-trauma patients. We identified trauma patients using the inclusion criteria as shown in Table 1. Patients were excluded from the study if they were medically unstable, under an involuntary psychiatric hold, currently intoxicated, or under police custody. Approximately 160,000 patients were treated in this ED during the 4-year time of this study, but the number of patients who were ineligible or did not consent was not specifically recorded.
Figure 1. Patient record selection flow chart.
Table 1. University hospital trauma activation criteria, modified from Orange County emergency medical services policy.27
Once participants gave verbal consent, the CASI system recorded patients’ self-reported data, including basic demographic background, number of drinks per day, drinks per week, reasons to cut back, and the subsequently calculated AUDIT score and “Readiness to change” scale. The survey was available in both English and Spanish, both written and audio. The study was reviewed and deemed exempt by the Human Subjects Research Institutional Review Board.
CASI Tablet
CASI is a self-administered computer-administered questionnaire used primarily for screening purposes. Studies showed that CASI was effective at identifying at-risk and consistent-with-dependency drinkers in less than 7 minutes, and demonstrated good acceptability by patients. It can be implemented in bilingual settings (English and Spanish) with minimal time commitment, and has shown to be an effective tool among the Spanish-speaking population in the ED.8,9 A follow-up study by Vaca et al10 supported the use of such SBIRT systems as holding “promise as a viable screening and intervention modality for a wide range of emergency department patients,” with up to 47% reduction in drinking amongst at-risk patients, 6 months afterwards.
The tablet can be administered at the bedside for ED and trauma patients. The technology employs a user-friendly text, touch-screen interface with an option for text-to-speech. Patient privacy is enhanced with options for Bluetooth technology and headphones. Patients receive a customized alcohol reduction plan and/or counselling referral information. The CASI alcohol screening section was first established based upon the National Institute on Alcohol Abuse and Alcoholism (NIAAA) guideline and AUDIT score.11 The CASI tablet screening interview time was decreased for non-drinkers and drinkers whose alcohol consumption was within recommended limits established by NIAAA. Lotfipour et al12 showed trauma patients found the CASI tablet to be both easy to use (92%) and a comfortable form of answering questions (87%).
Measurements
Demographics
CASI assessed basic respondent self-reported demographics such as gender, age, education level and language.
AUDIT score
AUDIT was first introduced in 1989 by the World Health Organization (WHO) and is now in its second edition.13 Studies continue to demonstrate superior sensitivity, specificity, reliability, and internal consistency for the AUDIT over other self-reporting methods.14 AUDIT also has good reliability across both field and web-based administrations, and has recently been used extensively with patients in the ED setting as a validated tool for CASI.15,8,10 According to the AUDIT scoring, patients were defined as “low-risk” when they are scored 0–7, and “at-risk” patients with an AUDIT score of 8–19. Patients in either group who drank more than NIAAA-recommended limits received a computer-guided brief interview, which included customized feedback, an assessment of readiness to change, reasons to cut back on drinking, goal setting, and a printed personal alcohol reduction plan.8,10 Patients who had an AUDIT score of 20 or more were “consistent-with-dependency” on alcohol, and received a follow-up consultation with a social worker.
NIAAA recommendation
The limits that have been set are defined as no more than 4 drinks per day, and no more than 14 drinks per week, for men under the age of 65, and no more than 3 drinks per day and no more than 7 drinks per week for women of all ages and men age 65 years and older.16,17
Readiness to change scale
As part of the intervention, CASI also subsequently assessed patients with drinking behavior above the NIAAA recommendations, by asking how ready they are to change their drinking behavior on a readiness to change scale from 1 to 10 (1=“not at all ready” and 10=“extremely ready”).18 Visual analogue scales for readiness to change (RTC) were introduced by Stott et al19 and applied to substance abuse interventions by Bernstein et al20. Such measures of RTC were related to a decrease in alcohol consumption among inpatients receiving a brief intervention and to expressed intentions to decrease drinking among young males.21,22
Reasons to cut back on alcohol
For those who drank more than the NIAAA-recommended limits, CASI inquired regarding the “reasons you want to cut back” on alcohol consumption, allowing users to choose any of 10 options as listed in Table 3. Users were allowed to choose more than one option, or no option, in this portion of the survey.
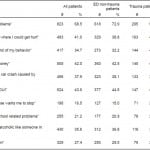
Table 3. Frequency, odds ratio (OR), and confidence interval (CI) regarding patient responses to “Reasons you want to cut back on alcohol consumption,” n=1,202, emergency department (ED) non-trauma versus trauma.
*OR and CI are from logistic regression adjusting for gender, age, language, and the number of other reasons cited by ED non-trauma and trauma patients.
Education level
Patients were also queried regarding their highest degree or level of education completed. Responses adapted from the United States Census,23 were collected in 9 different categories and were grouped into 4 categories for analysis: less than high school graduate, high school graduate, some college or associate degree, and bachelor’s or advanced degree.
Analyses
The data were saved by CASI as comma-separated text files. We imported these files into Stata (version 12.1, StataCorp, College Station, TX). We excluded incomplete records and records with identification numbers that indicated staff tests. Numeric variables were summarized with the median and interquartile range (IQR). We calculated the frequency of positive responses to “Reasons to cut back” and the chi-square test for independence to compare ED and trauma populations. Since a higher percentage of young males were trauma patients compared with ED patients, we used logistic regression to compare frequency of each positive response in ED patients to that in designated trauma patients, adjusting for gender, age in six categories, and the number of other responses checked. The responses of patients with the other 3 categories of education were compared to high school graduates, with adjustment for gender, age in 6 categories, the number of other responses checked, and ED versus designated trauma patient. We used linear regression to estimate the difference in the readiness to change scale (1 to 10), adjusting for age (in the same categories), gender, ED versus trauma patients, and AUDIT score.
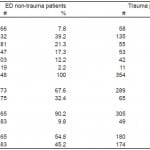
RESULTS
As described in the methods, we analysed 1,202 complete responses from non-dependent drinkers exceeding the NIAAA recommended drinking limits. These included 848 (70.6%) who were ED patients and 354 (29.4%) who were trauma patients. Patient demographic characteristics are shown in Table 2. The median age for the group was 30 (IQR 23–43). The largest portion of responses, 38.9%, was from patients in the 21–29 age group. More than twice the number of males compared to females (71.7% males overall) completed the survey, and this proportion was even more pronounced in trauma patients (81.6% male, p<0.001). Eleven percent of patients selected the Spanish-language option when taking CASI. The median AUDIT score was 7 (IQR 5–11), and the readiness to change scale (1–10) for these patients had a median of 8 (IQR 5–10).
Table 2. Patient characteristics by age, gender, language, and audit score, n=1,202, emergency department (ED) non-trauma versus trauma.
*p-values are from the chi-square test for independence, comparing the difference between ED non-trauma patients. p<0.05 was considered to be significant.
As shown in Table 3, the most common reason reported for cutting back on alcohol consumption was “To avoid health problems” (68.5%). This was followed by “To avoid getting a ‘driving under the influence’ (DUI)” (43.6%), “It could save me money” (42.0%), and “To avoid situations where I could get hurt” (41.0%). As shown in Table 3, respondents cited the other 6 reasons less than 38.0% of the time.
We found that trauma patients cited 3 particular reasons significantly more often than ED patients, both when assessed by chi-squared and logistic regression. These were: “To avoid situations where I could get hurt” (46.3% versus 38.8% respectively, odds ratio (OR) 0.48, 95% confidence interval (CI) 0.34–0.68), “So I can be in control of my behavior” (40.7% versus 32.2%, OR 0.49, 95% CI 0.35–0.70), and “My partner or spouse wants me to stop” (20.1% versus 15.0%, OR 0.62, 95% CI 0.43–0.89).
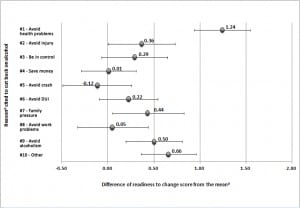
As shown in Figure 2, patients who cited “To avoid health problems” as a reason to cut back, reported 1.2 points higher than average (p<0.001) on the readiness to change scale, adjusted for other reasons cited, age, gender, AUDIT score, and patient type. Those who mentioned 3 other reasons, “My partner or spouse wants me to stop” (p=0.027), “Not to become an alcoholic like someone in my life” (p=0.001), and “Some other reason” (p<0.001), also reported slightly higher than average values on the readiness to change scale. The difference shown in Figure 2 were not substantially influenced by adjustment for age, gender, AUDIT score, and patient type, but were exaggerated if the other reasons were excluded from the regression.
Figure 2. Difference of readiness to change score from the mean versus reason cited to cut back on alcohol, mutually adjusted using linear regression (see text). Error bars show 95% confidence intervals.
aMean readiness to change score =7.24
bFull text of reasons cited: #1)“To avoid health problems”, #2)“To avoid situations where I could get hurt”, #3)“So I can be in control of my behavior”, #4)“It could save me money”, #5)“To avoid being in a car crash caused by alcohol use”, #6)“To avoid getting a DUI”, #7)“My partner or spouse wants me to stop”, #8)“To avoid work or school related problems”, #9)“Not to become an alcoholic like someone in my life”, #10)“Some other reason”
Those who had completed some college or an associate degree cited “To avoid health problems” less often than high school graduates (OR 0.45, 95% CI 0.23–0.90). They also reported cutting back on drinking “To avoid situations where I could get hurt” (OR 2.5, 95% CI 1.1–5.8) and “To avoid being in a car crash caused by alcohol use” (OR 3.8, 95% CI 1.5–9.7) more often than high school graduates. No other statistically significant correlations between reason to cut back and education level were found.
DISCUSSION
Several novel and first-reported findings were identified through this study, regarding reasons for intending to cut back on alcohol usage, readiness to change, and educational attainment. The most common reasons cited for cutting back on alcohol consumption were avoidance of health problems, avoidance of getting a DUI, cost savings, and avoidance of injury. In our investigation of the literature, there was no comparable study looking at these reasons. Trauma patients cited the following reasons significantly more frequently than ED patients: avoidance of injury, better control of behavior, and influence from spouse. Additionally, those patients who cited “To avoid health problems” as a reason to cut back also reported “a higher readiness to change.” This is an association that has not previously been reported. Analysis of education levels showed those who have completed some college or an associate degree had cited “To avoid health problems” less often than high school graduates, while they cited “To avoid situations where I could get hurt” and “To avoid being in a car crash caused by alcohol use” more often than high school graduates. This provides some further insight into the associations between educational levels and alcohol dependency as studied by Grant et al7.
Our study found that patients are more concerned with the impact of alcohol on their health, finances, and legal problems, than any other reasons provided to them. Based on these findings, the implications may be significant, as interventions that are customized to a patient’s CASI results can be more effective. As Leontieva et al25 illustrated, the setting of patient goals and referrals made to addiction facilities during the SBIRT phase were the most critical components in discriminating which patients generally improved. We suggest using the patient’s own intention to change as part of their brief intervention program, especially for those 823 (68.5%) patients in this study who specifically cited a desire to avoid health problems. In addition, the trauma patients in particular were proportionately more concerned with avoidance of situations where they could get hurt than their ED counterparts, which was another new finding not seen in the literature in the setting of alcohol drinkers.
It is noteworthy that health, injury, finances, and legal issues remain top concerns listed as reasons to cut back, for the patients surveyed in this study. Especially for those who had listed “To avoid health problems,” it is particularly important to take advantage of their reported higher readiness to change. Furthermore, trauma patients had proportionately more concerns with situations where they could get hurt, as an example, and this is critical information that could be leveraged into a teachable moment.12 Taking into account the education level of the respondent may also further direct treatment plans to those most interested.7 Such tailored treatments might include customized information and signed behavioral contracts that incorporate the same “Reasons to cut back” cited by the patients themselves. This would ideally lead to an even more sophisticated set of customized interventions that can be offered to patients prior to discharge, thus taking advantage of this unique brief opportunity for intervention with these patients.
LIMITATIONS
This study has some limitations to consider. Although the CASI and AUDIT score are validated tools, these results are nonetheless based upon self-reported data, which does lend itself to some degree of inaccuracy.8,14 Within the reasons to cut back on alcohol, there may be some bias introduced, given the order of reasons listed, as users may choose the first few reasons more often than the last few reasons. Additionally, the tenth reason provided to respondents, “Some other reason,” may contain some additional valuable data, which could be further dissected in future studies. External validity of this study may be somewhat limited with non-drinkers, or the heaviest drinkers, given the exclusion of those patients from this data set due to their higher rates of relapse.24 Thus, these results don’t generalize to those with AUDIT score <1, or those drinkers with an AUDIT score >19 (consistent with dependency). It is also worth noting that this was a convenience sampling of subjects enrolled in the study. The subjects were derived from patients in the ED and included non-trauma or trauma patients. As a result of this the data contain unequal sample sizes and may be less generalizable.
FUTURE RESEARCH
There remains room for further research in this area. Tailoring these brief interventions to specific populations may allow for customized healthcare reference material, highlighting the health risks of continued drinking. Studies have recently shown that patients whose brief intervention included a “behavioral contract,” attendance prompt, and subsequent reinforcers (CPR), were more likely to complete treatment programs, and remain abstinent for at least one year.26 Given sufficient time and resources, patients may be able to present their behavioral contract to a counselor from a 12-step or other substance abuse program. Such studies would produce even more valuable data on the utility of such an intervention, and allow for an examination of how intentions actually influence the reduction of at-risk drinking behavior over time.
CONCLUSION
Health, injury, finances, and legal issues remain top concerns for patients in this study, particularly the 68.5% who cited “To avoid health problems” as the most common reason for cutting back on alcohol consumption. Furthermore, trauma patients had proportionately more concerns with situations where they “could get hurt” compared to ED patients, and this is critical information that could be leveraged into a teachable moment. Future brief intervention could be more effective if tailored to address unique concerns of these 2 patient populations.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Shahram Lotfipour, MD, MPH, University of California Irvine, Department of Emergency Medicine, 101 The City Drive Rte 128-01, Orange, CA 92868. Email: shl@uci.edu. 5 / 2014; 15:337 – 344
Submission history: Revision received January 6, 2013; Submitted April 25, 2013; Accepted August 27, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 . Centers for Disease Control and Prevention (CDC). Alcohol-Related Disease Impact (ARDI) application. Atlanta, GA: United States Department of Health and Human Services, CDC, 2008. Available at: http://www.cdc.gov/alcohol/ardi.htm. Accessed February 01, 2012.
2 . Centers for Disease Control and Prevention (CDC). Vital Signs. Drinking and Driving: A Threat to Everyone. Atlanta, GA: United States Department of Health and Human Services, CDC, 2011. Available at: http://www.cdc.gov/vitalsigns/drinkinganddriving/?s_cid=vitalsigns-092-bb. Accessed February 01, 2012.
3 Lotfipour S, Mortazavi R, Chakravarthy B. Commentary: Alcohol and motor vehicle-related crashes-driver attitudes need further intervention. Ann Emerg Med. 2011;57(4):406-408.
4. Ewing T, Barrios C, Lau C, et al. Predictors of hazardous drinking behavior in 1,340 adult trauma patients: a computerized alcohol screening and intervention study. J Am Coll Surg. 2012;215:489-495.
5. Barnett NP, Goldstein AL, Murphy JG, et al. I’ll never drink like that again”: characteristics of alcohol-related incidents and predictors of motivation to change in college students. J Stud Alcohol. 2006;67(5):754-763.
6. Walton MA, Goldstein AL, Chermack ST, et al. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69:550-560.
7. Grant JD, Scherrer JF, Lynskey MT, et al. Associations of alcohol, nicotine, cannabis, and drug use/dependence with educational attainment: evidence from cotwin-control analyses. Alcohol Clin Exp Res. 2012;36(8):1412-1420.
8. Vaca FE, Winn D, Anderson CL, et al. Feasibility of emergency department bilingual computerized alcohol screening, brief intervention, and referral to treatment. Subst Abus. 2010;31:264-269.
9. Lotfipour S, Cisneros V, Anderson C, et al. Assessment of alcohol use patterns among Spanish-speaking patients. Subst Abus. 2013;34(2):155-161.
10. Vaca FE, Winn D, Anderson CL, et al. Six-month follow-up of computerized alcohol screening, brief intervention, and referral to treatment in the emergency department. Subst Abus. 2011;32:144-152.
11. National Institute on Alcohol Abuse and Alcoholism (NIAAA), of the National Institute of Health. Alcohol alert – Screening for alcohol use and alcohol related problems. 2005; 65. Available at: http://pubs.niaaa.nih.gov/publications/aa65/AA65.htm. Accessed February 28, 2012.
12. Lotfipour S, Cisneros V, Chakravarthy B Assessment of readiness to change and relationship to AUDIT score in a trauma population utilizing computerized alcohol screening and brief intervention. Subst Abus. 2012;33(4):378-386.
13. Babor TF, Higgins-Biddle JC, Saunders JB, et al. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in primary care, 2nd Edition. World Health Organization, Department of Mental Health and Substance Dependence. 2001;(WHO/MSD/MSB/01.6a). Geneva, Switzerland. Available at: http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf. Accessed January 21, 2012.
14. Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): A review of recent research. Alcohol Clin Exp Res. 2002;26(2):272-279.
15. Celio MA, Vetter-O’Hagen CS, Lisman SA, et al. Integrating field methodology and web-based data collection to assess the reliability of the Alcohol Use Disorders Identification Test (AUDIT). Drug Alcohol Depend. 2011;119:142-144.
16. World Health Organization. Drinking and Driving: a road safety manual for decision-makers and practitioners. 2007. Available at: http://www.who.int/roadsafety/projects/manuals/alcohol/drinking_driving.pdf. Accessed June 02, 2012.
17. United States Department of Health & Human Services. A Clinician’s Guide, Updated 2005 Edition – Helping Patients Who Drink Too Much. 2005. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Accessed January 02, 2013.
18. Hesse M. The Readiness Ruler as a measure of readiness to change poly-drug use in drug abusers. Harm Reduct J. 2006;3(3).
19. Stott NCH, Rollnick S, Rees MR Innovation in clinical method: diabetes care and negotiating skills. Fam Pract. 1995;12(4):413-418.
20. Bernstein E, Bernstein J, Levenson S. Project ASSERT: An ED–based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30:181-197.
21. Bertholet N, Cheng DM, Palfai TP, et al. Does readiness to change predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use?. Addict Behav. 2009;34(8):636-640.
22. LaBrie JW, Quinlan T, Schiffman JE, et al. Performance of alcohol and safer sex change rulers compared with readiness to change questionnaires. Psych Addict Behav. 2005; 19:112-115
23. United States Department of Commerce – Bureau of the Census. United States Census 2000. 2000. Available at: http://www.census.gov/dmd/www/pdf/d02p.pdf. Accessed February 01, 2012.
24. Cox WM, Klinger E A motivational model of alcohol use: determinants of use and change. Handbook of Motivational Counseling: Goal-Based Approaches to Assessment and Intervention with Addiction and Other Problems, Second Edition. 2011;131-149.
25. Leontieva L, Horn K, Helmkamp J, et al. Counselors’ reflections on the administration of screening and brief intervention for alcohol problems in the emergency department and 3-month follow-up outcome. J Crit Care. 2009;24:273-279.
26. Lash SJ, Stephens RS, Burden JL, et al. Contracting, prompting, and reinforcing substance use disorder continuing care: a randomized clinical trial. Psych Addict Behav. 2007;21(3):387-397.
27. University Hospital Trauma Activation Criteria. Modified from: Orange County EMS Policy/Procedure–Trauma Triage. 2011. Available at: http://healthdisasteroc.org/civicax/filebank/blobdload.aspx?BlobID=12145. Accessed January 3, 2013.