| Author | Affiliation |
|---|---|
| Jason A. Hoppe, DO | Department of Emergency Medicine, University of Colorado School of Medicine, Denver, Colorado |
| John Houghland, MD | Denver Health Residency in Emergency Medicine, Denver, Colorado |
| Michael Yaron, MD | Department of Emergency Medicine, University of Colorado School of Medicine, Denver, Colorado |
| Kennon Heard, MD | Department of Emergency Medicine, University of Colorado School of Medicine, Denver, Colorado Rocky Mountain Poison and Drug Center, Denver Health, Denver, Colorado |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: To use Colorado’s prescription drug monitoring program (PDMP) to describe the recent opioid prescription history of patients discharged from our emergency department (ED) with a prescription for opioid pain medications.
Methods: Retrospective cohort study of 300 adult ED patients who received an opioid prescription. We abstracted prescription histories for the six months prior to the ED visit from the PDMP, and abstracted clinical and demographic variables from the chart.
Results: There were 5,379 ED visits during the study month, 3,732 of which were discharged. Providers wrote 1,165 prescriptions for opioid analgesics to 1,124/3,732 (30%) of the patients. Median age was 36 years. Thirty-nine percent were male. Patients were 46% Caucasian, 26% African American, 22% Hispanic, 2% Asian and 4% other. These were similar to our overall ED population. There was substantial variability in the number of prescriptions, prescribers and total number of pills. A majority (205/296) of patients had zero or one prescription. The 90th percentile for number of prescriptions was seven, while the 10th percentile was zero. Patients in the highest decile tended to be older, with a higher proportion of Caucasians and females. Patients in the lowest decile resembled the general ED population. The most common diagnoses associated with opioid prescriptions were abdominal pain (11.5%), cold/flu symptoms (9.5%), back pain (5.4%), flank pain (5.0%) and motor vehicle crash (4.7%).
Conclusion: Substantial variability exists in the opioid prescription histories of ED patients, but a majority received zero or one prescription in the preceding six months. The top decile of patients averaged more than two prescriptions per month over the six months prior to ED visit, written by more than 6 different prescribers. There was a trend toward these patients being older, Caucasian and female.
INTRODUCTION
Prescription drug abuse is an increasing public health problem in the United States (U.S.). 1 Opioids are commonly prescribed for the relief of acute and chronic pain from multiple ambulatory settings, including pain clinics, office practices, dental practices and the emergency department (ED). However, access to these medications for the purposes of abuse is not uncommon; an estimated 10% of Americans report prescription drugs as their drug of choice for abuse;2 and among patients of chronic pain clinics, opioid abuse has been reported in up to 24% of individuals.3 An estimated 4.7 million people in the U.S. have taken opioids for nonmedical uses in the past month.4 Given the increased use and abuse of these medications prescription opioids have become the number 1 cause of poisoning deaths in the U.S., surpassing cocaine and heroin as causes of drug-associated death.5 The total number of prescription opioid related-deaths in the U.S. more than tripled from 1999–2006.6 The most recent estimate is that prescription opioids are responsible for 73.8% (14,800/20,044) of the prescription drug overdose deaths per year.7
Emergency medicine providers care for patients with pain from many different etiologies. The treatment of pain is frequently initiated without the benefit of an established doctor-patient relationship and often in an environment of limited time and resources. Patients and physicians may have different expectations for pain control. This may lead to frustrated or unsatisfied patients as reflected by the recent Institute of Medicine report suggesting that pain is undertreated in the ED.8 Opioids are an important component of acute and chronic analgesia. However, physicians must balance the need for adequate pain relief with the risk for misuse, abuse and diversion.
The National Institute on Drug Abuse has suggested that a large number of prescriptions from multiple providers is a marker of prescription drug abuse, but it has been difficult to accurately asses the number of prescriptions until recently.9 The National All Schedules Prescription Electronic Reporting (NASPER) Act of 2005 was established to support a controlled substance monitoring program in each state for the purpose of giving physicians a tool to aid in both prescribing controlled substances and identification of illicit fraud and abuse.10 Prescription drug monitoring programs (PDMP) seek to provide a balanced approach to protect public safety and public health while supporting legitimate medical practice. Colorado obtained funding for a PMDP in 2006 to monitor Schedule II, III, IV, and V prescriptions. Data collection began in July 2007 and went live to providers in February 2008, providing prescription profiles for providers and pharmacists.
The purpose of this study was to characterize the recent opioid prescription history of patients discharged from the ED with a prescription for opioid pain medications. As a secondary aim we described 2 subpopulations, the top decile and the bottom decile in terms of number of prescriptions, to explore potential markers that could characterize subjects who may be at increased risk of seeking opioid prescriptions for abuse and diversion or poorly controlled chronic pain.
METHODS
Study Design and Setting
The local human subject research committee approved this retrospective cohort study and waived informed consent as the study used retrospective data. The study institution is an urban, university-affiliated ED with approximately 55,000 visits annually and an admission rate of approximately 25%. Our ED records are generated by an ED information system (EDIS; Pulsecheck, Picis Inc, Wakefield, Illinois), and all prescriptions are generated electronically and printed for the patient.
Colorado’s prescription drug monitoring program tracks all dispensed prescriptions for controlled medications (excluding prescriptions dispensed at a Veterans Administration pharmacy), including opioids, in a database available to all providers with a Drug Enforcement Administration number. The database includes date filled, physician’s name, drug, dose, quantity of pills prescribed, days supply, class of drug, type of insurance and pharmacy name and city. It does not identify if the prescriber is affiliated with a hospital, office or ED. The state board of pharmacy is in charge of program operation and oversight. Information is uploaded by pharmacies on a bimonthly basis. The longest possible delay between filling a prescription and the information being uploaded is 28 days. Once uploaded, the information is immediately available to users.
Selection of participants
Eligible participants were 18 year or older, had been discharged from the ED, and had received a prescription at discharge for a controlled opioid-containing medication between October 1, 2009 and November 1, 2009. Subjects were excluded if they only received a cough preparation containing hydrocodone or codeine. For subjects with more than 1 visit where an opioid was prescribed, only the first visit during the month was considered. Subjects were selected by entering all records for the month into a spreadsheet (Microsoft office excel 97–2003), assigning each subject a random number using the RAND function and sorting the records using the random number assigned to each record. We then selected the first 300 records as study subjects.
Data collection
The data from the ED and the prescription drug monitoring program were collected by 2 separate teams and assigned random patient identifiers to preserve the confidentiality of personal health information. We are able to use our EDIS to automatically populate our data collection spreadsheet (Microsoft Office Excel 97–2003) with fields collected on all patients (e.g. age, sex, ethnicity, etc). Background data for our ED in the month of October was abstracted electronically from the EDIS. Demographic data for our study population (age, gender, and race) was abstracted electronically from the EDIS. Two trained physician investigators manually abstracted ED charts to determine if the patient reported a preexisting medical condition expected to cause chronic pain, if the patient reported an opioid as a medication, and social history. A history of any of the following was considered a chronic pain condition: fibromyalgia, complex regional pain syndrome/ reflex sympathetic dystrophy, or any pain syndrome described by the patient as chronic and documented in the ED chart (e.g., chronic low back pain, chronic abdominal pain, chronic headaches, etc). Investigators were blinded to PDMP data but not to the study hypothesis. Ten percent of the data from the EDIS automated abstraction and 20% of the data from manual chart abstraction were randomly selected for double abstraction to assess inter-rater agreement. The 2 trained abstractors reconciled disagreements.
The information from the prescription database was separately abstracted by 2 pharmacists affiliated with and familiar with the program who were blinded to the clinical data and the study hypothesis. The Colorado PDMP was searched by entering the patient name and birth date. Patients were identified in the database when both the name and birth date matched. Subjects were considered to be the same person if names were very similar and birthdates matched (i.e. Jon Smith and John Smith), or if they were hyphenated and birthdates matched (i.e. Jane Smith and Jane Smith-Jones). The abstractors reviewed the prescription records for the 6 months preceding, but not including the incident ED visit. Data abstracted included: number of prescriptions, number of pills, number of providers writing a prescription, number of pharmacies where prescriptions were filled and number of different payer sources. All of the information was deidentified and entered into a spreadsheet by study number only. Finally we merged the 2 de-identified spreadsheets by study number.
Methods of measurement
Race was coded as African-American, Asian, Caucasian, Hispanic, or other/unknown. We defined an allergy to opioids as a self-report of allergy to any opioid but not to tramadol. An allergy to other analgesics was defined as a self-report of allergy to acetaminophen, aspirin, tramadol or as an allergy to non-steroidals (as a group or individual medications). Alcohol use, tobacco use and illicit drug use were determined by selfreport. The variables obtained from the PDMP were abstracted as summary data (number of prescriptions, pills, and providers) for each patient rather than as individual data for each prescription. We did not record the specific medications a patient received.
We characterized patients in the top and bottom decile for number of opioid prescriptions in the 6 months preceding their ED visit. We selected number of prescriptions rather than total pills as our primary measure of use because we recognized that some chronic pain patients may require significant amounts of analgesic medications to treat their symptoms, but considered that optimal management for these cases would be fewer prescriptions for a larger total number of pills rather than many prescriptions for smaller numbers of pills.
Specific aims
Our primary aim was a characterization of the prescription history of patients who received opioid prescriptions in our ED. Our a priori secondary aim was a description of demographic and clinical characteristics of the top and bottom deciles in terms of number of prescriptions.
Analysis and Data Presentation
As we had no formal hypothesis for this exploratory study, we did not perform a power calculation and we used descriptive statistics. We used a sample size of 300 subjects as this provides a precision of plus/minus 6% for binomial variables with a frequency of 50%. Many of the variables were not normally distributed, so we used non-parametric statistics. For nominal data we determined proportions and for continuous data we used medians as a measure of central tendency and ranges and inter-quartile ranges as measures of variance.
RESULTS
In October 2009 our ED had 5,379 visits and 3,732 of those patients were discharged. The median age was 38 years with an interquartile range of 26 to 52 years. Fortyone percent were male. Patients were 46% Caucasian, 26% African American, 22% Hispanic, 2% Asian and 4% other or unknown. Providers wrote 1,165 prescriptions for opioid medications to 1,124/3,732 (30%) of the patients treated in the ED. The majority were for acetaminophen/hydrocodone (n=544), acetaminophen/oxycodone (n=347) or oxycodone alone (n=102). These 3 products accounted for 86% of all opioid prescriptions written that month.
The trained abstractors checked the electronic abstraction tool for accuracy. Ten percent of the charts were manually abstracted to verify the accuracy of the tool. Agreement between the abstraction tool and the abstractors for patient data (age, gender, chief complaint, prescription given, medications administer in the ED) was 99%. Each abstractor then reviewed 10% of the other abstractor’s charts to verify the accuracy between the 2. Inter-investigator agreement was 100%. The tool was not built to abstract chronic pain, so after electronic abstraction the presence of these conditions was reviewed for each patient by the 2 abstractors. Five disagreements regarding whether a given patient did or did not have a chronic pain syndrome among 296 (1.7%) patients were reconciled by joint chart review.
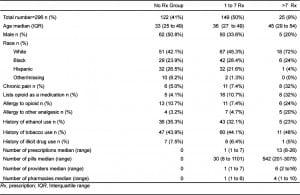
We did not initially filter our 300 study records by subject age and therefore 4 subjects younger than 18 were excluded from the preliminary analysis. The remaining 296 subjects were of similar age (median 36 years, IQR 27 to 74 years), gender (39.5% male) and racial distribution (46% Caucasian, 26% African American, and 22% Hispanic) as our overall ED population. The most common chief complaints for patients who received opioid prescriptions in this study were abdominal pain (34, 11.5%), cold/flu symptoms (28, 9.5%), back pain (16, 5.4%), flank pain (15, 5.0%) and motor vehicle crash (14, 4.7%).
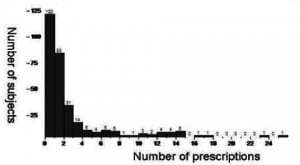
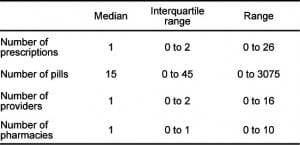
Overall, 205/296 (69%) patients who received a prescription for an opioid from our ED had 0 or 1 prescription for opioid-containing medications in the 6 months preceding their ED visit (Figure 1). There was substantial variation in the number of prescriptions, the total number of pills prescribed, the number of providers writing prescriptions and the number of pharmacies (Table 1). The 90th percentile for number of prescriptions in the 6 months preceding the ED visit was 7, while the 10th percentile was 0. As there were 122 patients with 0 prescriptions, we included all patients with 0 prescriptions in our description of the lowest decile.
The patients with 0 opioid prescriptions in the preceding 6 months resembled the general ED population in terms of age, gender and race. The patients in the highest decile appeared to be older, and had a higher proportion of Caucasians and females than our overall ED population (Table 2). More than 60% of patients in the highest decile did not report a chronic pain condition or opioids as a medication. For the highest decile, the median number of prescriptions per provider was 2, with a range from 1 to 6.5 and an interquartile range of 1.3 to 3.5.
DISCUSSION
The ED is a common destination for both patients seeking pain relief and those seeking to obtain prescription opioids for nonmedical use. To understand the breadth of the problem we need to first describe the population involved. Recent pharmacy data suggest that greater than 50% of outpatient opioid prescriptions were dispensed to patients who had already received an opioid prescription in the preceding month.11 However, we found that a majority of patients discharged form the ED with an opioid prescription received ≤ 1 opioid prescription in the preceding 6 months. A small percentage received a large number of prescriptions.
We describe patients in the highest decile of number of prescriptions who averaged greater than 2 prescriptions per month and received prescriptions from an average of 6 providers over the study period. These patients received significantly higher amounts of opioid pain medications than a majority of our ED patients. Our study design does not allow us to determine if these patients were abusing or diverting opioids. It appears that this group was certainly at risk for these costly and dangerous behaviors. A large number of prescriptions from multiple providers has been suggested by the National Institute on Drug Abuse as a marker of prescription drug abuse.9 If these patient were taking these pain medications as prescribed, they may have been at increased risk of death as recent data has described a strong association between the amount of opioids prescribed and risk of death.11,12
This study should not be interpreted as a call to decrease the number of appropriate opioid prescriptions provided to patients treated in the ED or to be in conflict with recent evidence that ED providers should be more aggressive in their treatment of pain.8,13–18 Our ultimate goal is to determine if PDMPs can be used to decrease inappropriate prescriptions while maintaining appropriate prescriptions and adequate pain management. This study represents 1 of the initial steps in that process by describing populations involved, specifically the ED population.
Similar PDMP systems are now available in 40 states, while 8 additional states have enacted legislation but are not yet operational.19 These programs provide objective information regarding a patient’s prescription history. It has been recommended that they be used in appropriate pain management, but there is little research on how to interpret this information.20 A number of states have begun using prescription monitoring program data as an epidemiologic tool. The present study is the first to combine this tool with clinical information to describe the recent prescription history and characteristics of patients receiving prescription opioids from the ED. Our study suggests there is substantial variability in the prescription histories of ED patients. Baehren et al. recently reported PDMP data among 179 ED patients, among which there was similar wide variability of number of recent prescriptions. In that study, clinician’s review of PDMP data resulted in a change in prescribing behavior in 41% of cases, resulting in a reduction of or no opioids being prescribed 61% of the time, but an increase in the amount of opioids in 39% of the cases .21
While we recognize that prescription history must be considered within the context of other clinical information, we believe that developing a “high risk” prescription profile would help physicians identify patients who have received a large number of opioid prescriptions and who may be at risk for abuse or poor pain management. Patients identified using these methods could be further screened for drug abuse in the ED, undergo a brief intervention, be referred for substance abuse treatment or have their pain management plans modified to improve their quality of care. Furthermore, real-time methods of screening patients for potential drug abuse and diversion need to be explored, including potentially the automatic inclusion of a patient’s PDMP data with his or her background medical data when seen for a clinic appointment or admission to the ED.
Acknowledgments
The authors would like to thank Amy Zosel, MD for her help in the preparation and proofreading the manuscript. The authors would like to acknowledge the Colorado Prescription Drug Monitoring Program for their assistance with this data abstraction and cooperation with this project.
LIMITATIONS
This study was performed at a single center with a small number of patients, which may not describe the population at large or apply to other settings. Physicians were not mandated to look up patients, and there is no way to track which patients were reviewed on the PDMP prior to receiving a prescription. This may have led to selection bias as a review of the PDMP by the individual provider may have affected the choice to prescribe opioids and prevented some frequent users from receiving a prescription and inclusion in our study. Our ascertainment of patient characteristics was limited by the retrospective data collection and manual provider data entry; it is possible that some information may have been incorrectly entered at the time of the ED visit.
Because our PDMP system relies on manual data entry to populate the databasethere is a potential for some inaccurate entries. We attempted to accommodate for this by including entries that were hyphenated or had similar spellings and the same birth date. It is also possible that drug-seeking individuals used several identities when acquiring prescription medications, which would result in several PDMP profiles and an underestimate of the amount of prescriptions identified in this study. The delay in pharmacies uploading data could potentially be as long as 28 days depending on when the prescription was filled. This was not an issue in this study as we chose a time period which would be outside the delay period. Methadone treatment programs and the Veteran Affairs Hospital are not required to participate in PDMP reporting in Colorado so it’s possible some patients may have additional prescribed opioids not identified by our search. The PDMP lists providers by name but not affiliation or address. Therefore, it is possible that prescriptions may appear to have come from different providers when in fact they were from providers working together within the same office or clinic.
Finally, our conclusions are limited by the study design. While we believe that some of the prescription patterns in the months preceding the ED visit are suggestive of drug abuse or misuse, the appropriateness of the opioid prescription written in the ED during the incident visit cannot be determined using this study design.
CONCLUSION
Footnotes
Supervising Section Editor: Brandon Wills, DO, MS
Submission history: Submitted October 14, 2011; Revision received January 17, 2012; Accepted February 20, 2012
Full text available through open access at http://escholarship.og/uc/uciem_westjem
DOI: 10.5811/westjem.2012.2.6915
Address for Correspondence: Jason Hoppe, DO, Department of Emergency Medicine, University of Colorado School of Medicine,
Mail stop B215, Aurora, CO 80045. Email: jason.hoppe@ucdenver.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed: Kennon Heard was supported by Award Number K08DA020573 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
REFERENCES
1. Cicero TJ, Dart RC, Inciardi JA. The development of a comprehensive risk-management program for prescription opioid analgesics: researched abuse, diversion and addiction-related surveillance (RADARS)Pain Med. 2007;8:157–170. et al. [PubMed]
2. Batten H, Prottas J, Horgan C. Drug Services Research Survey. Phase II Final Report. Submitted to the National Institute on Drug Abuse. Institute for Health Policy, Brandeis University; Waltham, MA: 1993.
3. Manchikanti L, Pampati V, Damron KS. Prevalence of opioid abuse in interventional pain medicine practice settings: a randomized clinical evaluation. Pain Physician. 2001;4:358–365. et al. [PubMed]
4. National Survey on Drug Use and Health. Available at: https://nsduhweb.rti.org/. Accessed May 31, 2010.
5. Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States.Pharmacoepidemiol Drug Saf. 2006;15:618–627. [PubMed]
6. CDC data brief. Increase in Fatal Poisonings Involving Opioid Analgesics in the United States, 1999–2006. Available at: http://www.cdc.gov/nchs/data/databriefs/db22.pdf. Accessed January 15, 2012.[PubMed]
7. Paulozzi LJ, Jones CM, Mack KA. Vital Signs: Overdoses of Prescription Opioid Pain Relievers –- United States, 1999–2008. MMWR. 2011;60:1487–1492. et al. [PubMed]
8. Cone DC, Richardson LD, Todd KH. Health care disparities in emergency medicine. Acad Emerg Med.2003;10:1176–1183. et al. [PubMed]
9. National Institute on Drug Abuse. Research Report Series: Preventing and recognizing Drug Abuse. Available at: http://www.nida.nih.gov/ResearchReports/Prescription/prescription6.html#Preventing. Accessed August 1, 2010.
10. Manchikanti L, Whitfield E, Pallone F. Evolution of the National All Schedules Prescription Electronic Reporting Act (NASPER): a public law for balancing treatment of pain and drug abuse and diversion. Pain Physician. 2005;8:335–347. [PubMed]
11. Volkow ND, McLellan TA, Cotto JH. Characteristics of opioid prescriptions in 2009. JAMA.2011;305:1299–1300. et al. [PMC free article] [PubMed]
12. Bohnert AS, Valenstein M, Bair MJ. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. at al. [PubMed]
13. Gomes T, Mamdani MM, Dhalla IA. Opioid dose and drugrelated mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171:686–691. et al. [PubMed]
14. Blank F, Mader T, Wolfe J. Adequacy of pain assessment and pain relief and correlation of patient satisfaction in 68 ED fast-track patients. J Emerg Nurs. 2001;27:327–334. et al. [PubMed]
15. Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med.1989;7:620–623. [PubMed]
16. Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department.J Emerg Med. 2000;18:7–12. [PubMed]
17. Brown JC, Klein EJ, Lewis CW. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42:197–205. et al. [PubMed]
18. Katz N, Houle B, Fernandez KC. Update on prescription monitoring in clinical practice: a survey study of prescription monitoring program administrators. Pain Med. 2008;9:587–594. et al. [PubMed]
19. Satus of State Prescription Drug Monitoring Programs. Available athttp://www.namsdl.org/documents/StatusofStates011112.pdf. Accessed January 11, 2012.
20. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305:1346–1347. [PubMed]
21. Baehren DF, Marco CA, Droz DE. A statewide prescription monitoring program affects emergency department prescribing behavior. Ann Emerg Med. 2010;56:19–23. et al. [PubMed]


