| Author | Affiliation |
|---|---|
| Claudia A. Santucci, MD | Kern Medical Center, Department of Emergency Medicine |
| Thomas B. Purcell, MD | Kern Medical Center, Department of Emergency Medicine |
| Carlo Mejia | Kern Medical Center, Department of Emergency Medicine |
ABSTRACT
Introduction:
The objective of this study was to determine if the white blood cell count can predict severity of injury in blunt trauma victims.
Methods:
This was a retrospective study comparing two groups of blunt trauma victims by severity of injury, one with significant injury and one without significant injury, and comparing their initial WBC in the emergency department (ED). We also examined if WBC correlates with degree of injury using Injury Severity Score (ISS) in both groups combined. Further, we examined the WBC as a predictor of serious injury.
Results:
Our study showed a difference in mean WBC between the two groups that was statistically significant (p<0.001). A positive relationship between ISS and WBC was found, although the association was weak (correlation coefficient = 0.369). While the WBC had moderate discriminatory capability for serious injury, it could not, in isolation, reliably rule in or out serious injury. Nevertheless, this study supports using WBC on presentation to the ED as an adjunct for making disposition decisions.
Conclusion:
A significant elevation in WBC in a blunt trauma patient, even with minimal initial signs of severe injury, should heighten suspicion for occult injury.
INTRODUCTION
Identifying significant injury in the trauma patient remains a difficult task. Having early markers of injury may help the clinician prevent serious decompensation of patients and thus improve their outcome and hasten their disposition. We set out to determine if WBC can aid physical exam, history, and other tests in detecting severe injury in blunt trauma victims.
Leukocytosis in trauma/stress is due to neutrophilia, caused by neutrophil margination, and not due to increased marrow production or release of immature cells or bands. The phenomenon is short-lived, lasting only minutes to hours.1 In theory, patients with significant injury should have a higher degree of leukocytosis compared to patients with minor injuries. Since the CBC is one of the first tests obtained from trauma patients in the emergency department (ED), WBC level could serve as an easy-to-obtain marker for serious injury.
METHODS
The study was conducted at Kern Medical Center, a metropolitan county teaching hospital, Level II trauma center with approximately 50,000 yearly ED visits, and 2,400 trauma activations per year. The hospital is the only trauma center in Kern County, California, serving a population of approximately 800,000. This study was a retrospective analysis. Initial patient identification utilized the hospital trauma database. Entry criteria included all ED patients treated for blunt trauma, whether admitted or discharged from the ED, between January 1, 2003 and July 31, 2004. Exclusion criteria were non-blunt trauma (such as penetrating trauma or burn victims), or lack of white blood cell count determination on admission. Medical records for all entered patients were retrieved and examined by a single research assistant. Accuracy was reviewed by a 100 percent review of all charts and data by the principal investigator for the data outlined below. Standard definitions and criteria were used to obtain the data. IRB approval was obtained for this study.
Data collected included WBC on admission, patient age, sex, race, co-morbid conditions, prescription medication use, drug/alcohol intoxication, presenting Injury Severity Score (ISS), disposition, and time elapsed between injury and WBC blood draw. Co-morbid conditions that might affect the degree of leukocytosis were recorded, including pregnancy, chronic infection, diabetes, cardiovascular disease, pulmonary disease, cancer, liver disease, pancytopenia on presentation, and immunologic diseases. Prescription drug use such as steroids, immuno-suppressants, lithium, beta agonists, as well as recreational drug use and drug toxicology results, including methamphetamine, cocaine, opiates, benzodiazepines, and alcohol, were also recorded.
Patients were divided into two groups by severity, one with significant injury and one without significant injury. Significant injury was defined as any of the following injuries: all intra-abdominal and intracranial injuries, spinal and skull fractures, pelvic diastasis, pulmonary contusions, hemothorax, pneumothorax, flail chest, and bronchial tree, great vessel or major arterial injuries. These injuries were documented in the medical records either on admission, via radiologic or operative reports, during the hospital course, or on discharge diagnosis. Also included in the significant injury group were all patients with associated symptoms of hypotension (systolic blood pressure equal to or less than 90 mmHg) on arrival in the ED, death, requirement of transfusion, or operative management within the initial 24 hours following injury. Patients requiring operative management within 24 hours included injuries such as severe degloving injuries, pelvic fractures, severe facial injuries, bronchial tree lacerations, arterial injuries, open extremity fractures, open joint injuries, urogenital injuries requiring surgery.
The non-significant injury group included all remaining patients with minor injuries not meeting the significant injury specifications outlined above, such as patients with non-emergent extremity fractures, as well as all patients that may have been admitted for observation who did not develop significant injuries.
A one-tailed design was selected, since prior reports have not shown trauma to be a cause of lowered, only elevated, white counts. Assuming an alpha error of 0.05, a beta error of 0.20, a standard deviation of 5,000 WBC and a detectable effect size of 1500 WBC/mm3, 137 patients per group would be required. Evaluation of whether a significant difference between groups existed was determined by assessing WBC as a predictor of serious injury and carried out using receiver operator characteristic (ROC) analysis. Continuous data were summarized as mean ± one standard deviation, and were compared using the student’s t-test. Categorical data were compared using the chi-square test. Statistical significance was set at an alpha error of 0.05.
Outcome among patients discharged home from the ED was assessed by review of the entire patient’s medical record, which include all patient visits. Records were reviewed for each study participant. If patients were followed up in trauma clinic or other specialty clinic visits, the clinic visit was available for review in medical records.
RESULTS
A total of 279 blunt trauma patient records were reviewed. Of these, 142 were found to have significant injury and 137 did not have significant injury. Of those patients with significant injury, seven were dead on arrival or died in the ED, 127 were admitted to the hospital (44 via the operating room), seven were transferred to another institution, and one was discharged home after observation. Of those without significant injury, 85 were admitted and 52 were discharged home.
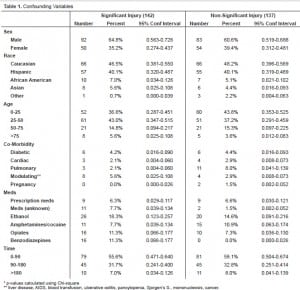
Confounding variables were compared and occurred with similar frequency in the two groups with some exceptions (Table 1). Pulmonary co-morbidities were more frequent in the non-injury group (8% vs. 2%); prescription medication use was more common in the significant injury group (7.7% vs. 1.5%) and positive benzodiazepine screens were seen more often in patients with significant injury (11% vs. 0%). The mean WBC for the significant injury group was 16,900 ± 7,590. Mean WBC for the non-significant injury group was 11,050 ± 4,560. The difference in WBC values between the two groups was statistically significant (Student’s t=7.77, p<0.001).
In order to examine the relationship between admission WBC and Injury Severity Score (ISS) we combined groups (Figure 1). Although a positive relationship between ISS and WBC was found (ISS = 0.69 × WBC + 4.1) the association was weak (correlation coefficient = 0.369).
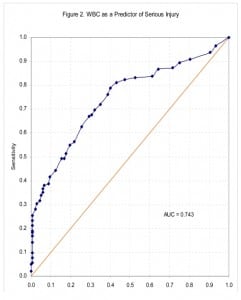
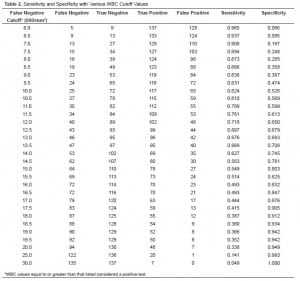
We next examined the admission WBC as a predictor of serious injury. After ranking subjects in order of ascending WBC values, sensitivities and specificities were calculated for various cut-offs for WBC values. Among patients with WBC values at or above the cut-off level, those with serious injury were counted as true positives, those without serious injury as false positives. Among patients with WBC values below the cut-off, those with no serious injury were counted as true negatives, those with serious injury as false negatives (Table 2). An ROC curve plot of the results of this analysis is shown in Figure 2. The area under the resulting ROC curve was 0.743 (moderate discriminating power).
DISCUSSION
Even among patients not sustaining significant injury, patients presenting to the ED following blunt trauma tended to have elevated, or at least high normal, WBC values, suggesting that the stress of the trauma incident itself can result in marked demargination, even in the absence of major injury. It is clear from our sample that WBC levels falling within the normal range cannot be used to rule out major injury. While WBC alone cannot be used to effectively rule in or rule out serious injury, its moderate ability to discriminate between patients with and without serious injury suggests that it may contribute meaningfully to the constellation of data used to make disposition decisions. Further study incorporating this variable into prediction models would clarify its value in this regard.
Past studies have either focused on subpopulations of blunt trauma patients, i.e., pediatric or head trauma patients, or studied several variables affecting WBC, and have shown mixed results. Review of the literature reveals several related studies:
Akköse et al2 performed a retrospective study evaluating 713 blunt trauma patients showing that WBC was positively correlated with ISS. Chang et al3 prospectively studied 882 patients admitted to a Level 1 trauma center evaluating admission WBC (only available for 786 patients) and GCS, race, injury mechanism, BP, and patients requiring early transfusion vs. no early transfusion, and found that only ISS greater than 15, GCS less than or equal to 8, and white race were associated with increases in white blood cell count. Harris et al4 retrospectively studied 46 patients after blunt abdominal trauma. They found that, in patients without obvious indications for invasive evaluation of the abdomen (e.g., peritoneal lavage, laparoscopy, laparotomy), leukocytosis was associated with intestinal injury.
Holmes et al5 retrospectively evaluated 1040 patients <15 years of age with blunt traumatic injury admitted to Level 1 trauma center and concluded that in children hospitalized for blunt torso trauma who are at moderate risk for intraabdominal injury, elevated WBC was associated with intra-abdominal injury.
Rovlias et al6 prospectively studied 624 patients with head injury and found patients with severe head injury had significantly higher WBC than those with moderate or minor injury. In severe head injury patients, WBC was also associated with unfavorable outcome.
LIMITATIONS
Our study sample of all patients presenting to a trauma center included patients admitted and discharged from the ED. However, our trauma study population proved to be predominantly young (mostly under 50 years of age) and white/hispanic.
Retrospective analysis is always limited to available data within medical records. In order to more accurately apply results of this study to our typical patient population, we elected not to exclude patients with conditions that may affect the degree of leukocytosis, such as age, medical history, prescription medication use, or drug/alcohol intoxication. Some of these confounding variables may have skewed the results.
Assessment of outcome was limited to patients seen at Kern Medical Center. It was assumed that patients with new or recurrent symptoms would return to their initial visit site at Kern Medical Center, the only trauma center in Kern County. However, any patients that may have left the county or returned to an outside hospital may have been missed. No follow-up calls to discharged patients were conducted.
CONCLUSION
The white blood cell count, taken in isolation, cannot be relied upon to rule in or rule out serious injury in blunt trauma patients. Nevertheless, this study supports using WBC on presentation to the ED as an adjunct for making disposition decisions. A significant elevation in WBC in a blunt trauma patient, even with minimal initial signs of severe injury, should heighten suspicion for occult injury.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted June 27, 2007; Revision Received December 5, 2007; Accepted January 31, 2008.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Claudia Santucci, M.D., 320 Lincoln Street, Bakersfield, CA 93305
E-mail: fusillikopf@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Abramson N, Becky M. Leukocytosis: basics of clinical assessment. American Family Physician. 2000;62:2053–2060. [PubMed]
2. Akköse S, Bulut M, Erol A, Veysel B, et al. Does the leukocyte count correlate with the severity of injury? Turkish Journal of Trauma and Emergency Surgery. 2003;9:111–113. [PubMed]
3. Chang DC, Cornwell EE, 3rd, Phillips J, Paradise J, et al. Early leukocytosis in trauma patients: what difference does it make? Curr Surg. 2003;60:632–635. [PubMed]
4. Harris HW, Morabito DJ, Mackersie RC, Halvorsen RA, et al. Leukocytosis and free fluid are important indicators of isolated intestinal injury after blunt trauma. J Trauma.1999;46:656–659. [PubMed]
5. Holmes JF, Sokolove PE, Land C, Kuppermann N. Identification of intra-abdominal injuries in children hospitalized following blunt torso trauma. Acad Emerg Med.1999;6:799–806. [PubMed]
6. Rovlias A, Kotsou S. The blood leukocyte count and its prognostic significance in severe head injury. Surg Neurol. 2001;55:190–196. [PubMed]